Infant care is provided primarily by the child’s parents or other caregiver. A physician can greatly impact the quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement of this care during the regularly scheduled outpatient visits, also known as well-child visits. During these visits, the physician has an opportunity to perform a comprehensive assessment of the child’s health, gauge caregivers’ apprehension about their role, and evaluate the overall growth environment of the child. Routine visits should be scheduled at regular Regular Insulin intervals, with additional visits for acute concerns. The physician should conduct a history and physical examination; assess growth, development, and nutritional status; encourage administration of vaccinations; and provide anticipatory guidance and counseling to parents or caregivers, making sure to address any questions and concerns and to foster optimal development and support.
Last updated: Nov 2, 2023
Well-child checks are visits scheduled at crucial ages in a child’s development. These checks are necessary to assess overall health, to provide preventive services, for early detection of disease and abnormalities, and for prompt management of health concerns.
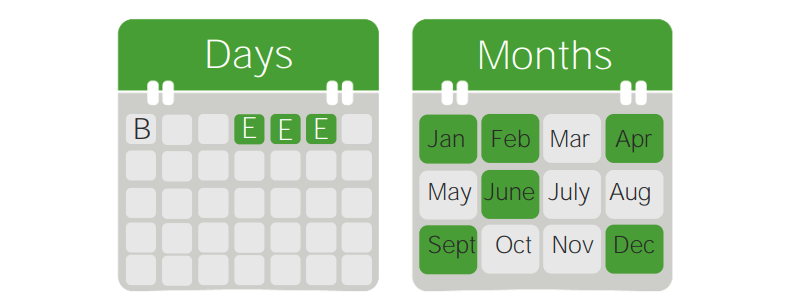
Schedule for a baby born on January 1
B: birth
E: exam
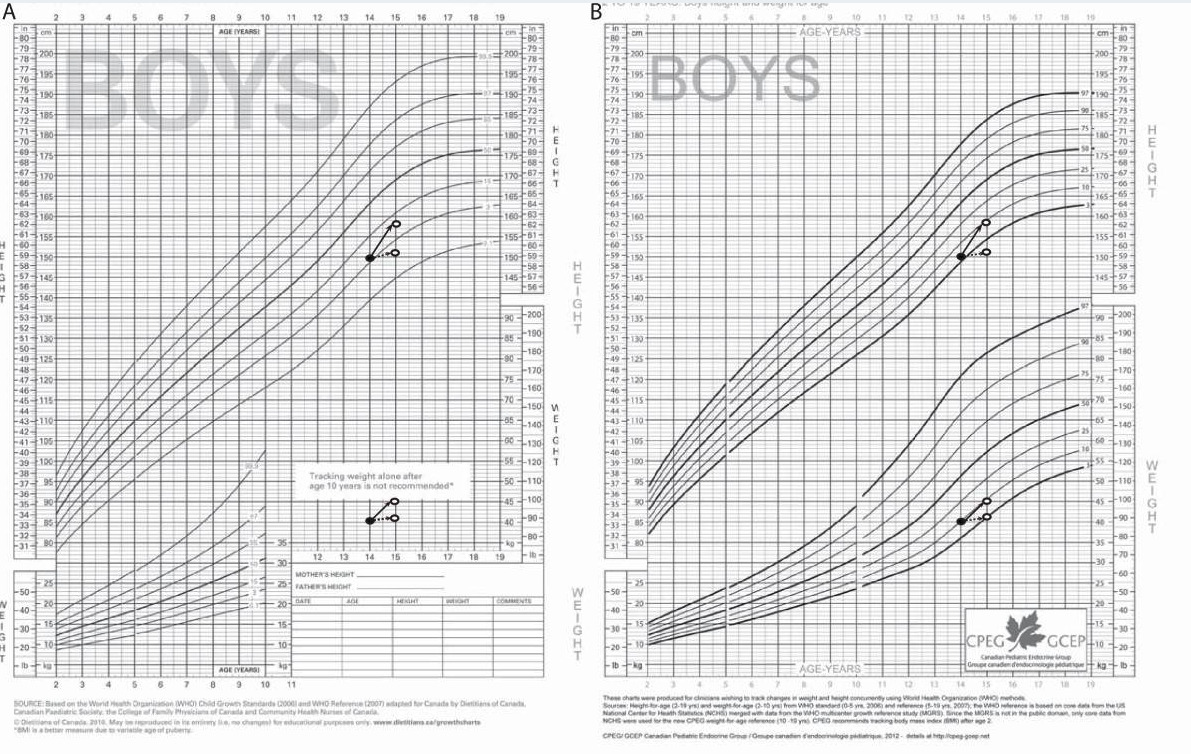
Growth charts:
Height and weight should be recorded at every well-child visit (head circumference until 3 years old). The results are plotted on standardized growth charts to monitor growth progression along percentile lines.
Breastfeeding Breastfeeding Breastfeeding is often the primary source of nutrition for the newborn. During pregnancy, hormonal stimulation causes the number and size of mammary glands in the breast to significantly increase. After delivery, prolactin stimulates milk production, while oxytocin stimulates milk expulsion through the lactiferous ducts, where it is sucked out through the nipple by the infant. Breastfeeding is the primary source of nutrition for infants and is recommended as the exclusive means of feeding for the 1st 6 months of life, with continuation up to 2 years of age.
Mature human milk contains necessary nutrients for infant and provides antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions formed by the mother, protecting the baby against infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease as the immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs develops.
Benefits to infant:
Benefits to mother:
Breast milk storage:
If there are challenges with breastfeeding Breastfeeding Breastfeeding is often the primary source of nutrition for the newborn. During pregnancy, hormonal stimulation causes the number and size of mammary glands in the breast to significantly increase. After delivery, prolactin stimulates milk production, while oxytocin stimulates milk expulsion through the lactiferous ducts, where it is sucked out through the nipple by the infant. Breastfeeding, expressed breast milk should be given to infant.
Breastfed infants should not be encouraged to drink formula except in the following situations:

Breastfeeding an infant
Image: “Breastfeeding infant” by Ken Hammond. License: Public DomainIf an infant is formula-fed, it is important to discuss the type of formula used:
Appropriate mixing and ratio of powdered formula to water should be reviewed.
| Age | Gross motor Gross Motor Developmental Milestones and Normal Growth | Fine motor Fine Motor Developmental Milestones and Normal Growth | Language | Social/cognitive |
|---|---|---|---|---|
| 1 month |
|
Hands clenched in fists brought near face most of the time | Makes sounds |
|
| 2 months |
|
|
|
|
| 4 months |
|
|
|
|
| 5 months |
|
|
|
|
| 6 months | Sits for brief moment propped on hands |
|
|
Stranger anxiety Anxiety Feelings or emotions of dread, apprehension, and impending disaster but not disabling as with anxiety disorders. Generalized Anxiety Disorder |
| 7 months | Sits steadily without support | Grasps using side of hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy (radial– palmar grasp Palmar Grasp Primitive Reflexes) |
|
|
| 9 months |
|
Grasps with 2 fingers and thumb below (radial–digital or 3-finger grasp) |
|
|
| 10 months |
|
Grasps pellet with side of index finger and thumb (inferior pincer grasp) | Says “dada” (specific) |
|
| 12 months | Takes 1st independent steps (walk might be delayed up to 18 months) |
|
Says at least 1 word other than “dada” or “mama” |
|
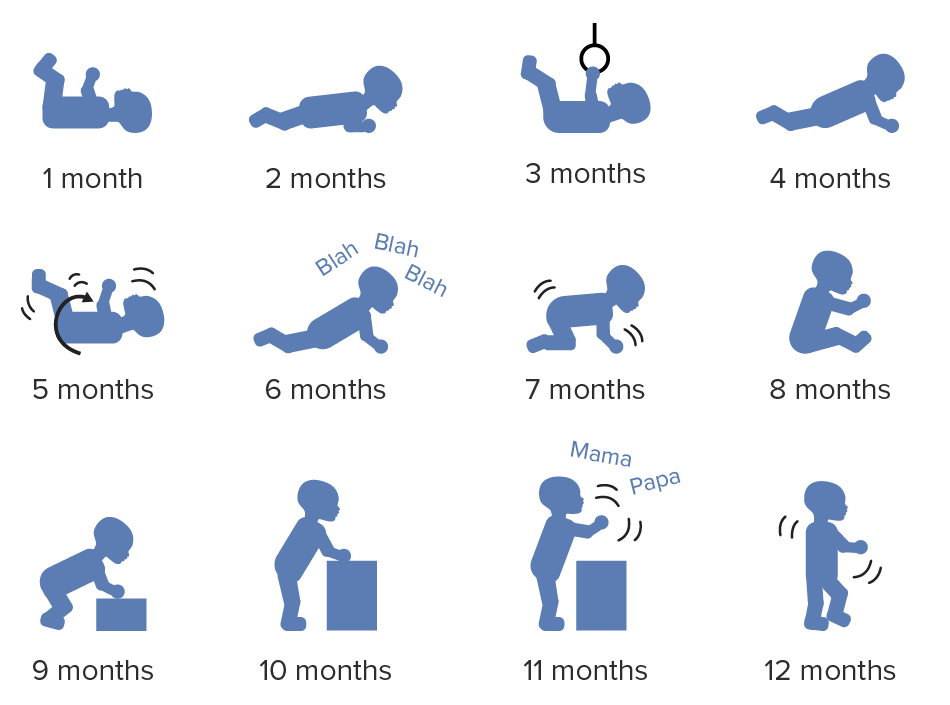
Gross motor development of the baby during the 1st year of life
Image by Lecturio.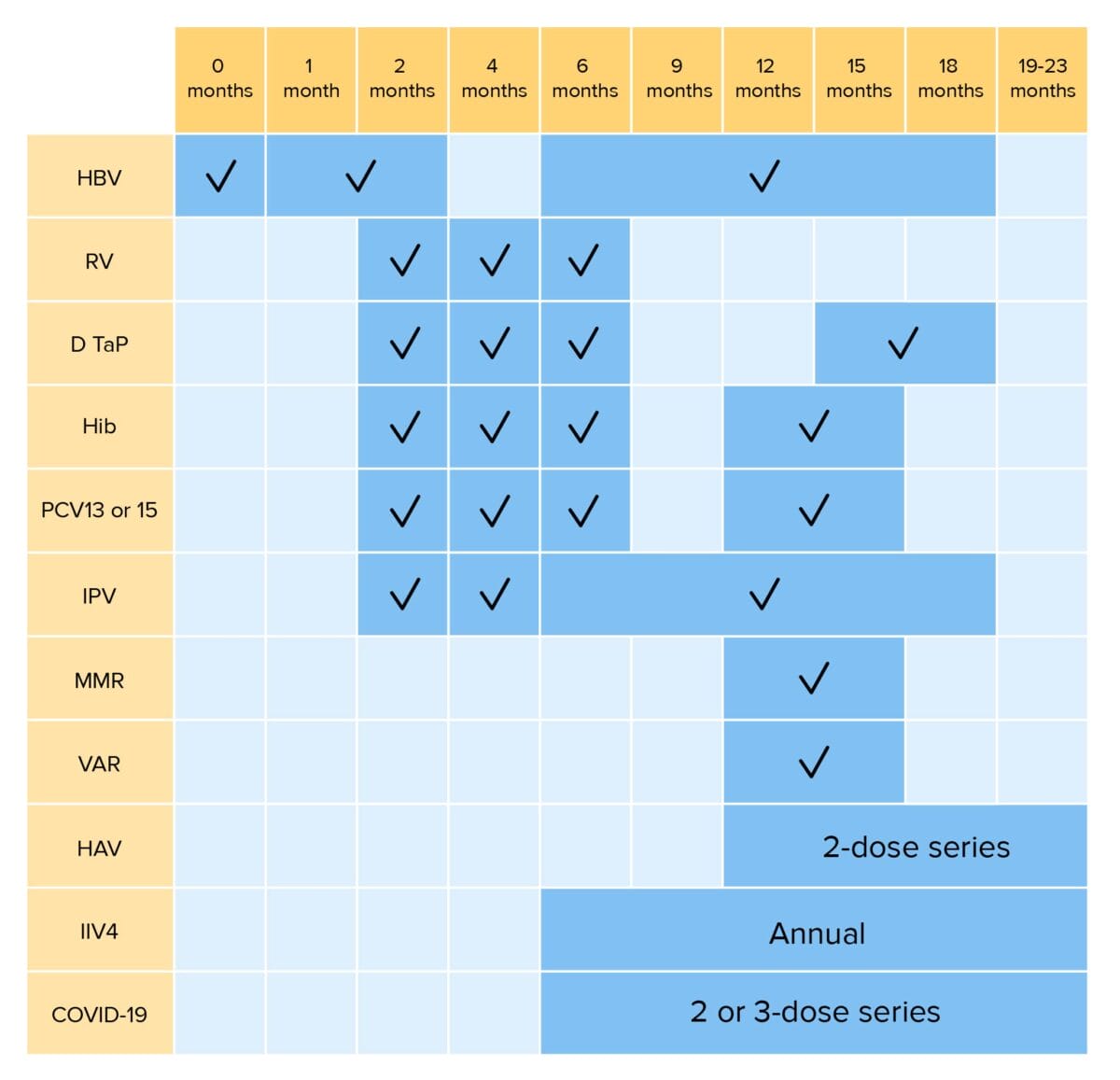
Routine vaccinations for children up to 23 months of age:
HBV: hepatitis B virus vaccination
RV: rotavirus vaccination
DTaP: diphtheria, tetanus, and pertussis vaccination
Hib: Haemophilus influenzae type b vaccination
PCV: pneumococcal conjugate vaccination
IPV: inactivated poliovirus vaccination
MMR: measles, mumps, and rubella vaccination
VAR: varicella vaccination
HAV: hepatitis A virus vaccination
IIV4: quadrivalent inactivated influenza vaccination
COVID-19: coronavirus disease 2019 vaccination (bivalent)
*RV1 is a 2-dose series; RV5 is a 3-dose series
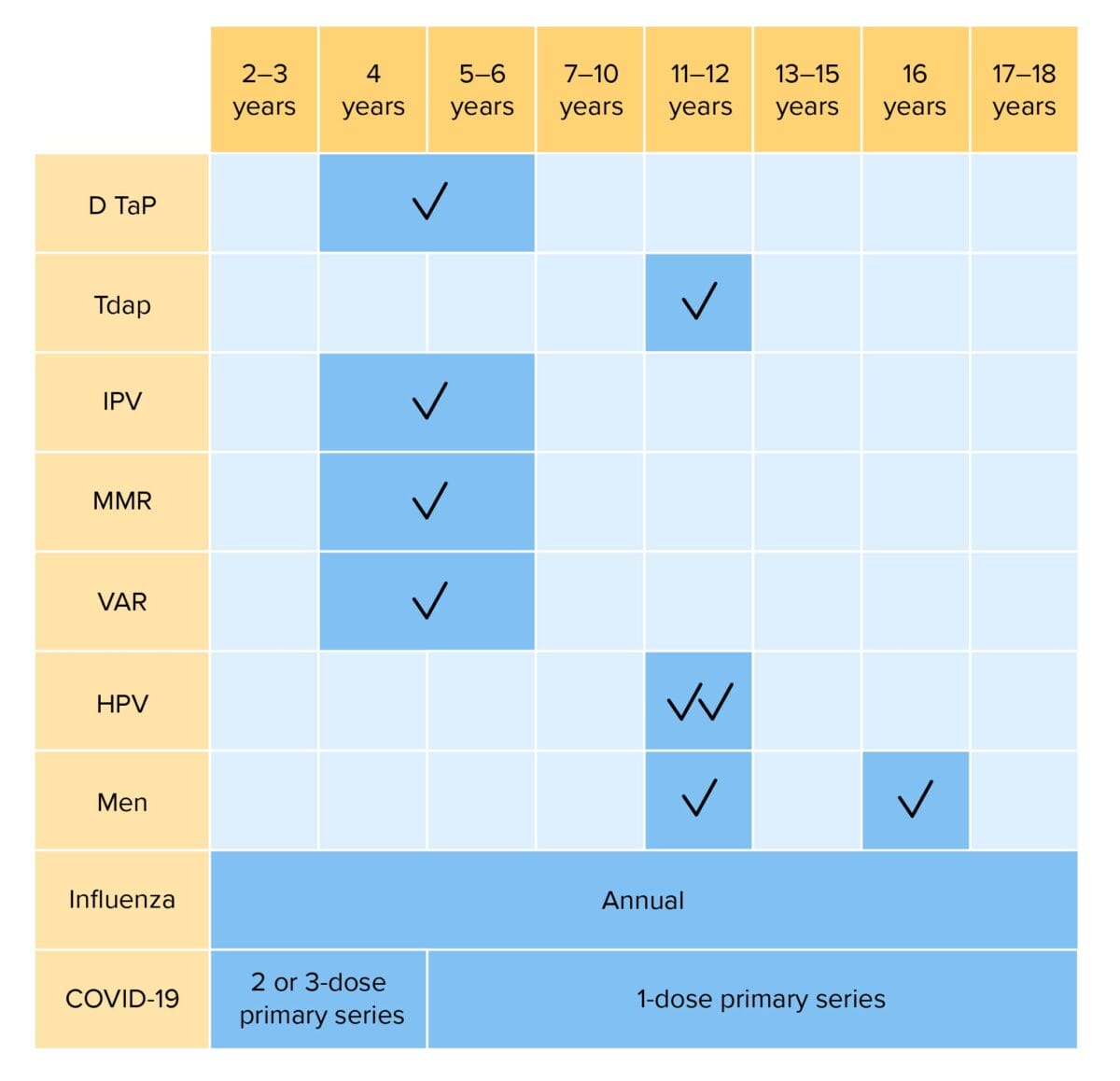
Routine vaccinations for children 2–18 years of age:
DTaP: diphtheria, tetanus, and acellular pertussis vaccination
Tdap: tetanus, diphtheria, and acellular pertussis vaccination
Hib: Haemophilus influenzae type b vaccination
IPV: inactivated poliovirus vaccination
MMR: measles, mumps, and rubella vaccination
VAR: varicella vaccination
HPV: human papillomavirus vaccination
Men: meningococcal vaccination
COVID-19: coronavirus disease 2019 vaccination (bivalent)
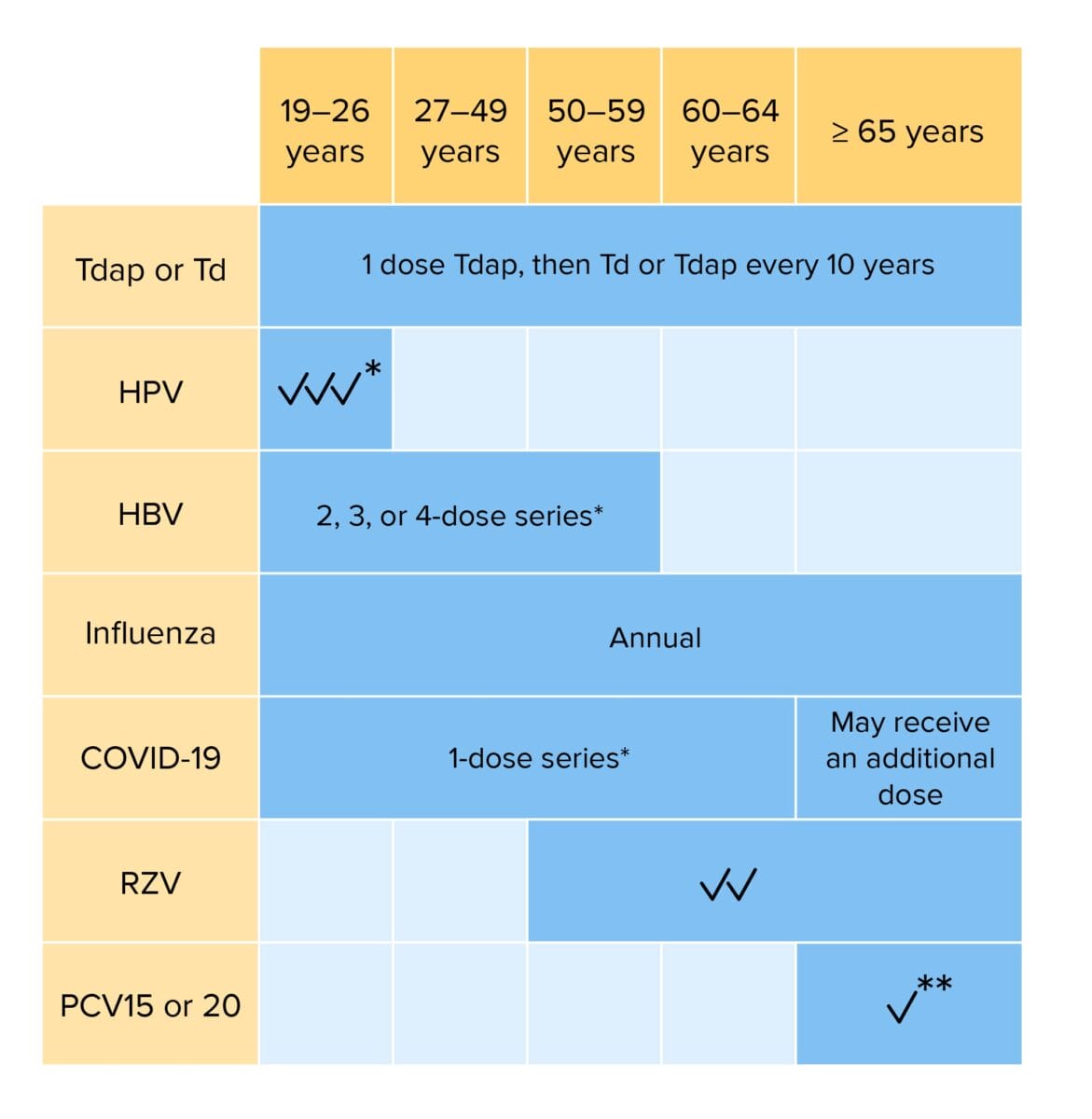
Routine vaccination for adults:
Individuals with risk factors may require additional vaccinations or alterations in dosing schedule.
Tdap: tetanus, diphtheria, and acellular pertussis vaccination
Td: tetanus and diphtheria vaccination
HPV: human papillomavirus vaccination
HBV: hepatitis B virus vaccination
COVID-19: coronavirus disease 2019 vaccination (bivalent)
RZV: recombinant zoster vaccination
PCV: pneumococcal conjugate vaccination
*If not previously vaccinated
**If PCV15 is given, should be followed PPSV23 (pneumococcal polysaccharide vaccination)
Caregivers should be counseled to seek further evaluation immediately if any of the following signs or symptoms occur.

Peripheral cyanosis over a palm
Image: “Showing peripheral cyanosis over a palm” by Department of Biochemistry, University of Allahabad, Allahabad-211002, India. License: CC BY 2.0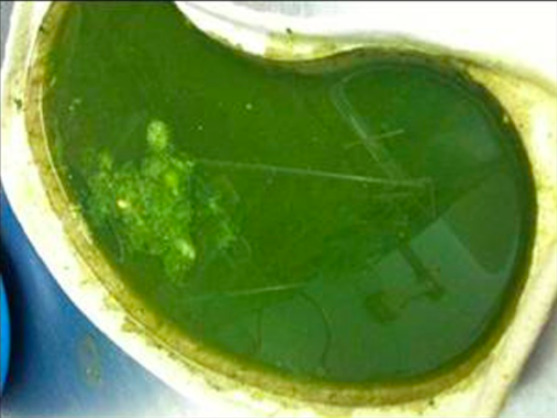
Typical dark green vomit often referred to as bilious vomiting
Image: “Typical dark green vomit” by Department of Paediatric Surgery, Leeds General Infirmary, United Kingdom LS1 3EX. License: CC BY 3.0
A day-old baby with its cord stump still attached
Image: “A day-old baby with its cord stump still attached” by Evan-Amos. License: Public Domain
Mild benign diaper rash in breastfed, cloth-diapered male infant 3 weeks of age
Image: “Irritant diaper dermatitis” by Dailyboth. License: CC0 1.0The following conditions are relevant to those seen in the course of providing infant care.

Neonatal jaundice in a newborn undergoing phototherapy
Image: “Jaundice phototherapy” by Martin Pot. License: CC BY 3.0