The bones of growing children exhibit unique characteristics, which, combined with the unique mechanisms of injury seen in children, result in fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures patterns differing significantly from those common in adults. The greenstick fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures is an incomplete fracture Incomplete Fracture Buckle or Torus Fracture usually seen in long bones Long bones Length greater than width. Bones: Structure and Types. The bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types is typically bent, and the fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures extends only partway through the bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types. Greenstick fractures Greenstick Fractures Osteomalacia and Rickets are at high risk for refracture and should be completely immobilized. Greenstick fractures Greenstick Fractures Osteomalacia and Rickets rarely require reduction but should be managed cautiously to prevent malunion Malunion Hip Fractures or angulation Angulation Buckle or Torus Fracture deformities. A patient with a greenstick fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures should be referred for orthopedic follow-up.
Last updated: Jan 21, 2025
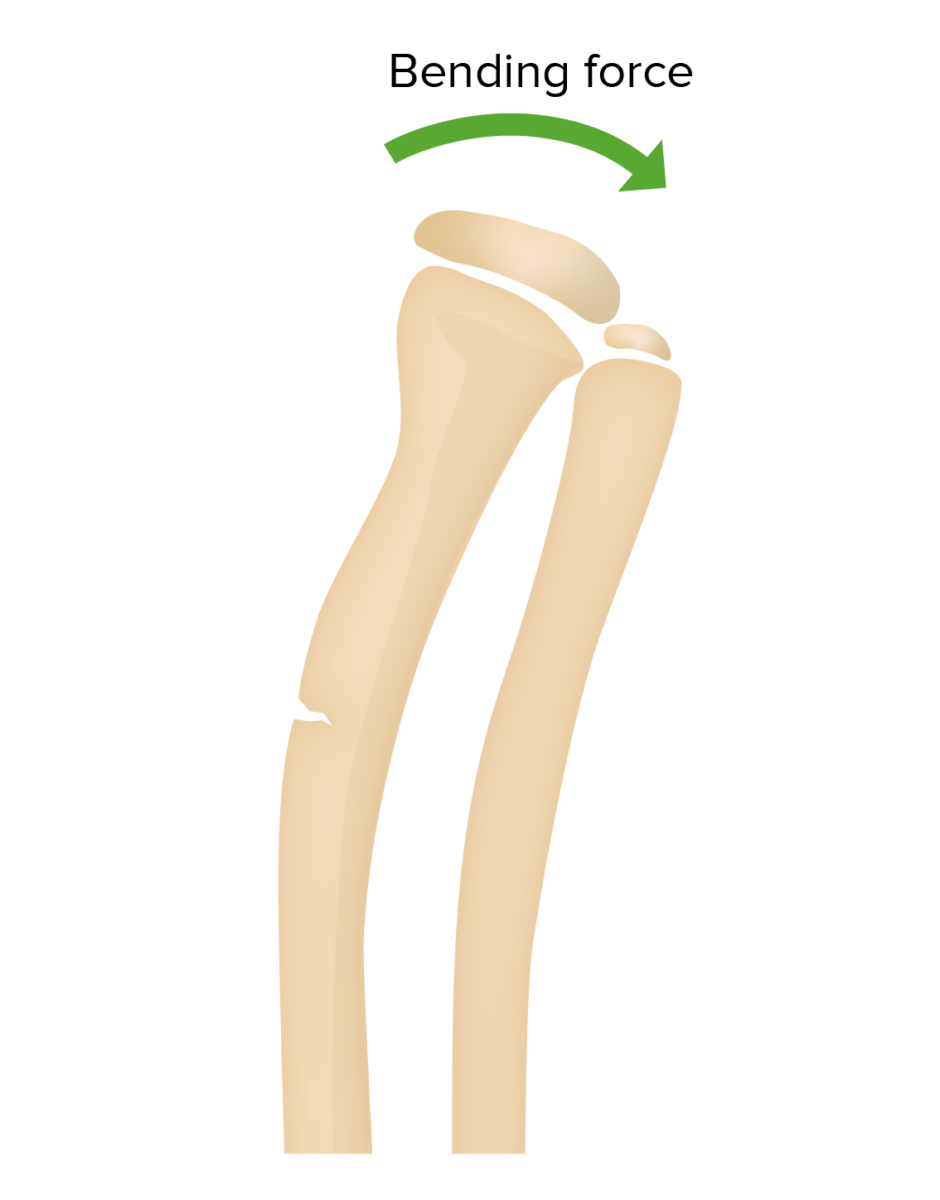
A greenstick fracture is a partial thickness fracture, which involves a complete fracture of the cortex and periosteum on only 1 side of the bone. The fracture is termed “greenstick” as it resembles the break in a live, green twig where 1 side of the stick remains intact.
Greenstick fracture of the radius:
Greenstick fractures feature disruption of the periosteum and cortex of the bone on only 1 side. A plastic deformity of the ulna can also sometimes be seen.
Location:
Causes:
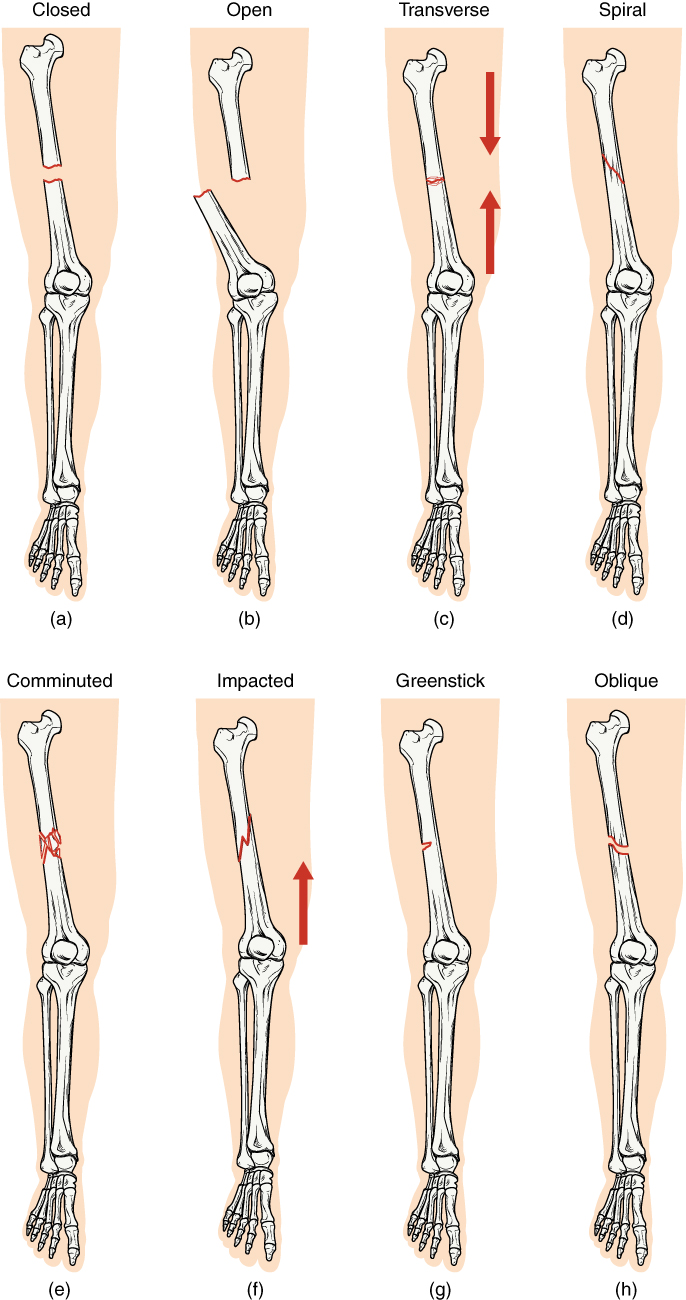
Comparing healthy bone with different types of fractures:
(a) closed fracture
(b) open fracture
(c) transverse fracture
(d) spiral fracture
(e) comminuted fracture
(f) impacted fracture
(g) greenstick fracture
(h) oblique fracture
Clinical presentation of pediatric patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with greenstick fractures Greenstick Fractures Osteomalacia and Rickets is similar to other pediatric fractures.
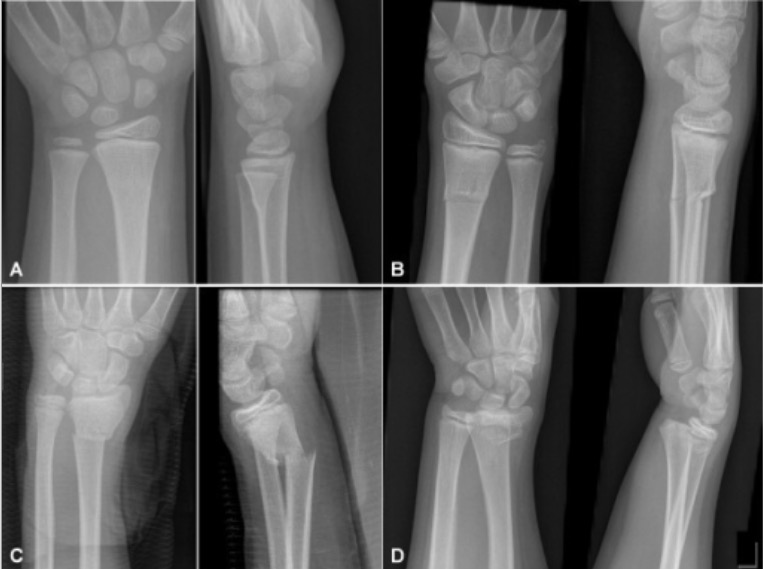
Examples of fractures from each category:
A: buckle fracture, rated as “buckle” on all readings
B: greenstick fracture, rated as “greenstick” on 20 of 24 readings
C: complete fracture, rated as “complete” on all readings
D: physeal fracture, as rated by all raters on both readings

Greenstick type fracture of the mid-shaft of right tibia:
Note the fracture on 1 side of the bone and the slight angular deformity (buckle) on the opposite side.
Management of a greenstick fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures is based on displacement Displacement The process by which an emotional or behavioral response that is appropriate for one situation appears in another situation for which it is inappropriate. Defense Mechanisms and the amount of angulation Angulation Buckle or Torus Fracture of the fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures.
Additional important pediatric skeletal injuries: