Adenomyosis is a benign Benign Fibroadenoma uterine condition characterized by the presence of ectopic endometrial glands and stroma within the myometrium. Adenomyosis is a common condition, affecting 20%–35% of women, and typically presents with heavy menstrual bleeding Heavy menstrual bleeding Excessive menstrual blood loss (objectively defined as > 80 mL blood loss/cycle). Can be based on heavy flow, as determined by the patient Abnormal Uterine Bleeding and dysmenorrhea. Diagnosis is often made with pelvic imaging. Usually, transvaginal ultrasound Transvaginal Ultrasound Obstetric Imaging is adequate, though MRI can be helpful in indeterminate cases. Management is based on the patient’s preference regarding future childbearing and may include hysterectomy (definitive treatment), other surgical options, or medical hormonal suppression Suppression Defense Mechanisms (usually with progestins Progestins Compounds that interact with progesterone receptors in target tissues to bring about the effects similar to those of progesterone. Primary actions of progestins, including natural and synthetic steroids, are on the uterus and the mammary gland in preparation for and in maintenance of pregnancy. Hormonal Contraceptives).
Last updated: Mar 19, 2025
Adenomyosis is the presence of ectopic endometrial glands and stroma located within the myometrium:
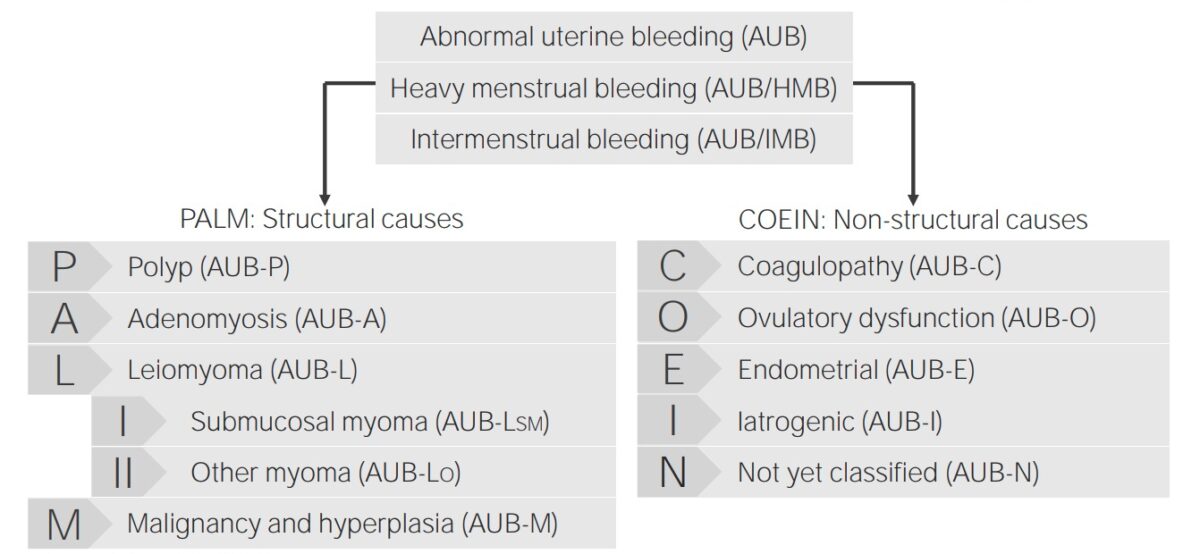
Classification of abnormal uterine bleeding and its causes
Image by Lecturio.The exact etiology is unknown.
Inappropriate endometrial tissue Endometrial tissue The mucous membrane lining of the uterine cavity that is hormonally responsive during the menstrual cycle and pregnancy. The endometrium undergoes cyclic changes that characterize menstruation. After successful fertilization, it serves to sustain the developing embryo. Endometriosis proliferation within the myometrium can lead to heavy menstrual bleeding Heavy menstrual bleeding Excessive menstrual blood loss (objectively defined as > 80 mL blood loss/cycle). Can be based on heavy flow, as determined by the patient Abnormal Uterine Bleeding ( HMB HMB Excessive menstrual blood loss (objectively defined as > 80 mL blood loss/cycle). Can be based on heavy flow, as determined by the patient Abnormal Uterine Bleeding) and dysmenorrhea.
Physical exam may reveal a uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy that is:
The diagnosis relies on history, exam, and imaging. Laboratory evaluation is not helpful.
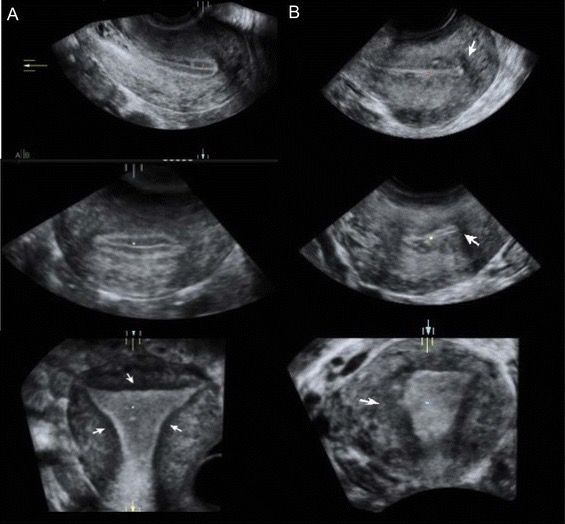
Transvaginal ultrasound demonstrating a uterus with adenomyosis:
A: ultrasounds of normal uterus
B: ultrasound images in a patient with adenomyosis: Notice the asymmetric thickening of the myometrium, particularly posteriorly. The arrows point to the junctional zone, which appears thickened and irregular.
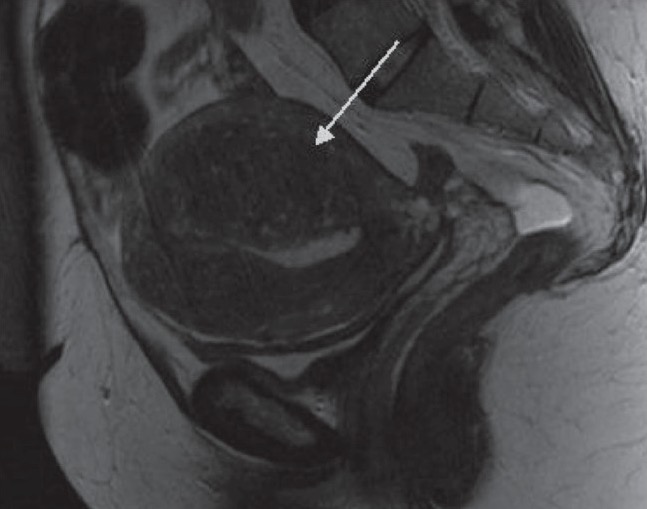
Pelvic MRI of a uterus with adenomyosis:
This MRI shows thickening of the junctional zone, which is most marked posteriorly (arrow). Several small cystic spaces can be seen within it.
Management is directed primarily by the patient’s desire for future fertility.