Atrioventricular septal defects (AVSDs) are a category of congenital defects of the endocardial cushion Endocardial cushion A fetal heart structure that is the bulging areas in the cardiac septum between the heart atria and the heart ventricles. During development, growth and fusion of endocardial cushions at midline forms the two atrioventricular canals, the sites for future tricuspid valve and bicuspid valve. Development of the Heart and atrioventricular valves (AVVs) resulting in abnormal interatrial and/or interventricular communication Communication The exchange or transmission of ideas, attitudes, or beliefs between individuals or groups. Decision-making Capacity and Legal Competence. Severe forms present early during infancy with failure to thrive Failure to Thrive Failure to thrive (FTT), or faltering growth, describes suboptimal weight gain and growth in children. The majority of cases are due to inadequate caloric intake; however, genetic, infectious, and oncological etiologies are also common. Failure to Thrive and recurrent pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia, and require early surgical correction to avoid pulmonary hypertension Pulmonary Hypertension Pulmonary hypertension (PH) or pulmonary arterial hypertension (PAH) is characterized by elevated pulmonary arterial pressure, which can lead to chronic progressive right heart failure. Pulmonary hypertension is grouped into 5 categories based on etiology, which include primary PAH, and PH due to cardiac disease, lung or hypoxic disease, chronic thromboembolic disease, and multifactorial or unclear etiologies. Pulmonary Hypertension.
Last updated: Jan 26, 2025
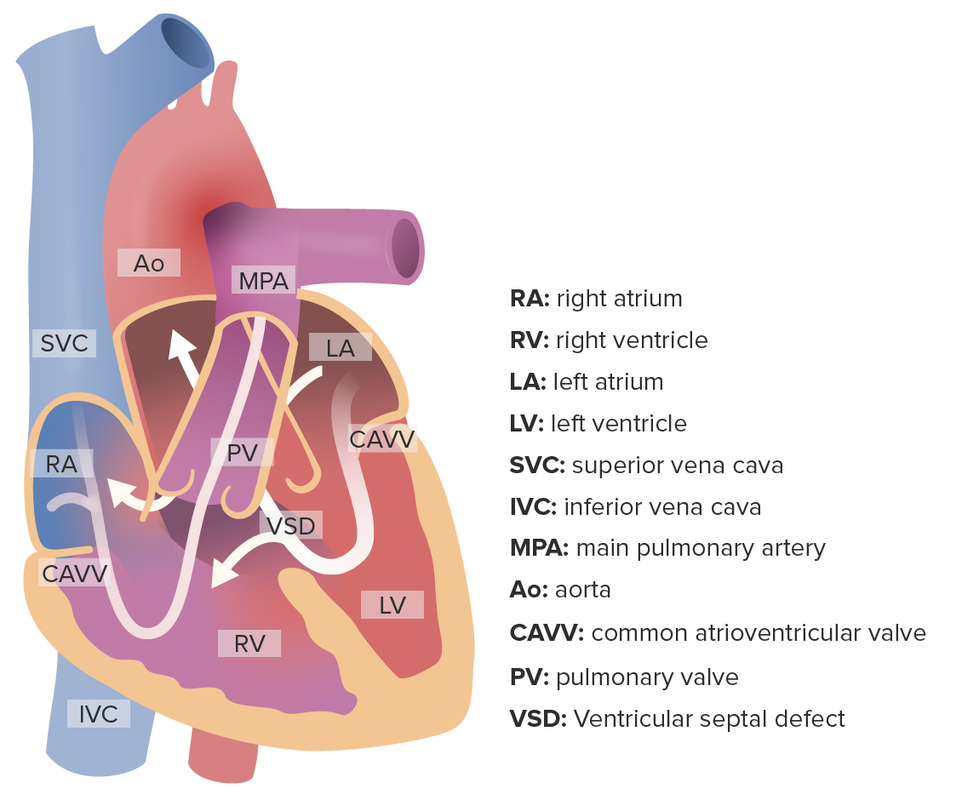
Complete atrioventricular septal defect: Notice the simultaneous flow of blood from the left atrium and ventricle to their right counterparts.
Image by Lecturio.Classification of AVSD is based on anatomy of defect:
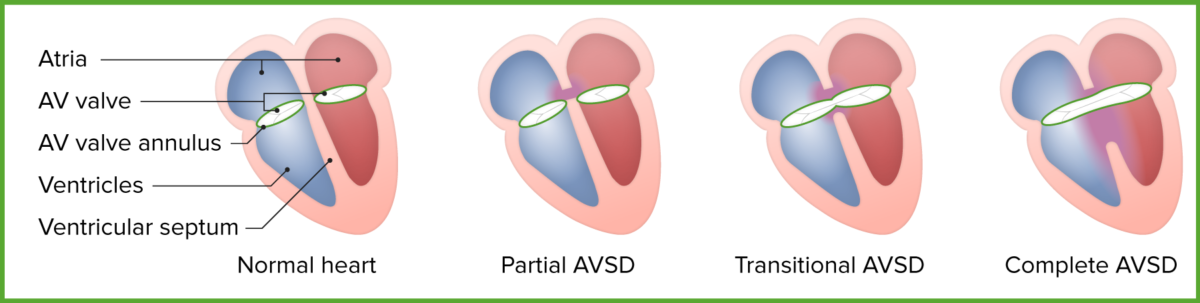
Forms of atrioventricular septal defect
Image by Lecturio.Symptoms of AVSD ( cyanosis Cyanosis A bluish or purplish discoloration of the skin and mucous membranes due to an increase in the amount of deoxygenated hemoglobin in the blood or a structural defect in the hemoglobin molecule. Pulmonary Examination, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), and pulmonary hypertension Pulmonary Hypertension Pulmonary hypertension (PH) or pulmonary arterial hypertension (PAH) is characterized by elevated pulmonary arterial pressure, which can lead to chronic progressive right heart failure. Pulmonary hypertension is grouped into 5 categories based on etiology, which include primary PAH, and PH due to cardiac disease, lung or hypoxic disease, chronic thromboembolic disease, and multifactorial or unclear etiologies. Pulmonary Hypertension) are due to excessive blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure in the pulmonary system.
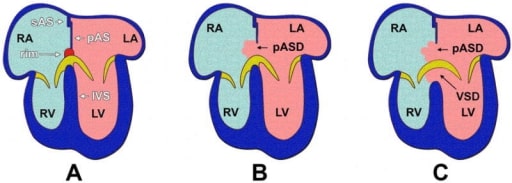
Anatomy of the atrioventricular septation complex in a human 4-chambered heart with normal anatomy and in hearts with AVSDs.
(A) shows a properly septated heart with a complete atrial and ventricular septum;
(B) depicts a heart with an incomplete AVSD; and in
(C) a heart with a complete AVSD is shown.
Note that when a primary atrial septal defect is observed, the muscular rim at the base of the atrial septum is missing.
IVS = interventricular septum,
pAS = primary atrial septum,
pASD = primary atrial septal defect,
LA = left atrium,
LV = left ventricle,
RA = right atrium,
RV = right ventricle,
VSD = ventricular septal defect.
Severe partial or complete atherosclerotic cardiovascular disease (ASCVD): large cardiac silhouette with a prominent pulmonary artery Pulmonary artery The short wide vessel arising from the conus arteriosus of the right ventricle and conveying unaerated blood to the lungs. Lungs: Anatomy arch and increased pulmonary vascularity
Significant changes seen with complete ASCVD:
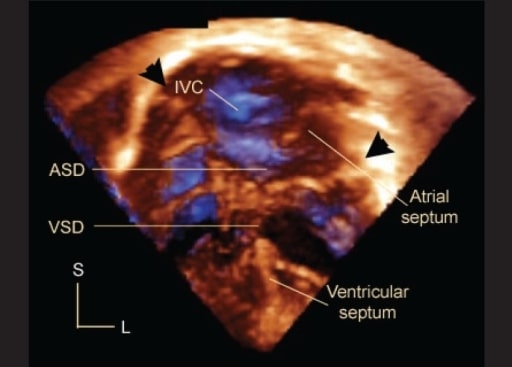
An apical 4-chamber 3-D echocardiogram in a patient with AVSD. Arrowheads mark the hinges of the common atrioventricular junction. The bridging leaflets divide the defect into an interatrial (ASD) and interventricular (VSD) component. Note the posterior location of the inferior vena caval orifice (IVC) relative to the septal structures. L, left; S, superior.
Image: “Three dimensional echocardiography in congenital heart defects” by Department of Pediatrics, Medical University of South Carolina, USA. License: CC BY 2.0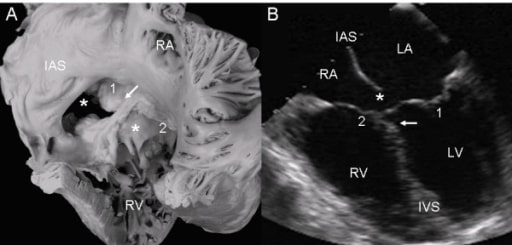
Atrioventricular septal defect with 2 separate atrioventricular valves.
(A): Internal view of right chambers, left (1) and right (2) atrioventricular valves, ostium primum (asterisk), and arrow pointing to the insertion of the septal leaflets of the left valve in the crest of the interventricular septum. Note the confluence of the ostium primum with the atrioventricular septal defect (upper asterisk), the commissure that separates those leaflets, the ample commissure between the septal leaflets, and the anterior leaflet of the right atrioventricular valve (lower asterisk).
(B): The 2 separate atrioventricular valves (1 and 2) and the fusion of the septal leaflets to the crest of the interventricular septum that closes the ventricular septal defect (arrow) can be seen. IAS: interatrial septum.