Perianal and perirectal abscesses are collections of pus in the enclosed space near the perirectal tissues. These infections originate from obstruction of anal crypt glands. Patients present with severe pain in the anal or rectal area. Finding a tender, fluctuant mass on physical exam can provide the diagnosis. Management requires prompt surgical incision and drainage, which may be followed by a course of antibiotics in some cases. Untreated, these abscesses can lead to the formation of fistulas.
Last updated: Mar 4, 2024
Anal glands, found in the intersphincteric Intersphincteric Perianal and Perirectal Abscess plane, drain into crypts found along the circumference of the dentate/ pectinate line Pectinate line Rectum and Anal Canal: Anatomy. Infection of an obstructed glandular crypt may occur due to:
Common bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology:
The classification of anorectal abscesses is based on their location.
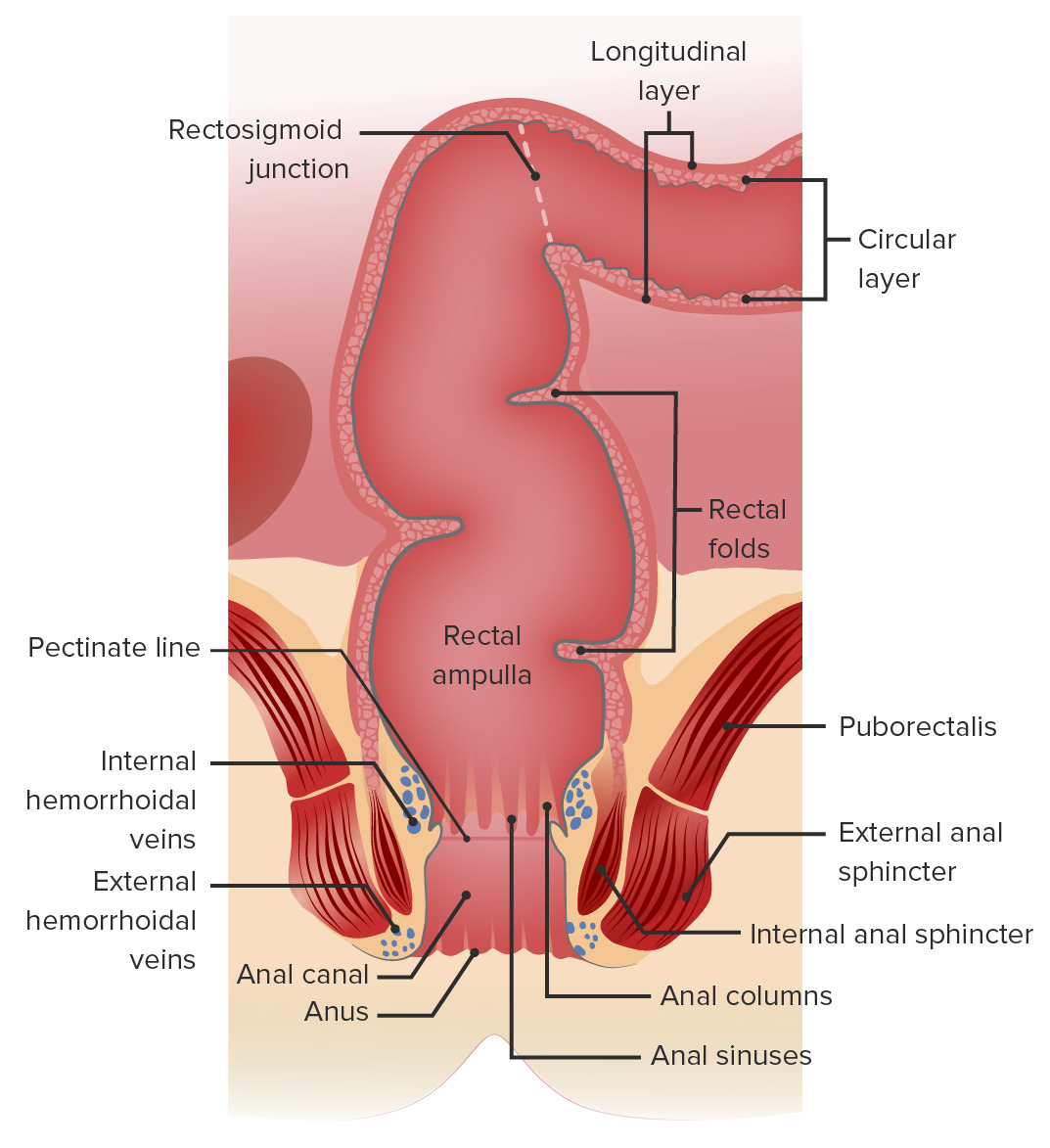
Relevant anatomy of the anus and rectum:
The perianal space surrounds the anus. The ischiorectal space extends laterally from the external sphincter to the ischium. The intersphincteric space is the area between the external and internal anal sphincters. The supralevator space is above the levator ani (the puborectalis is part of the levator ani complex).
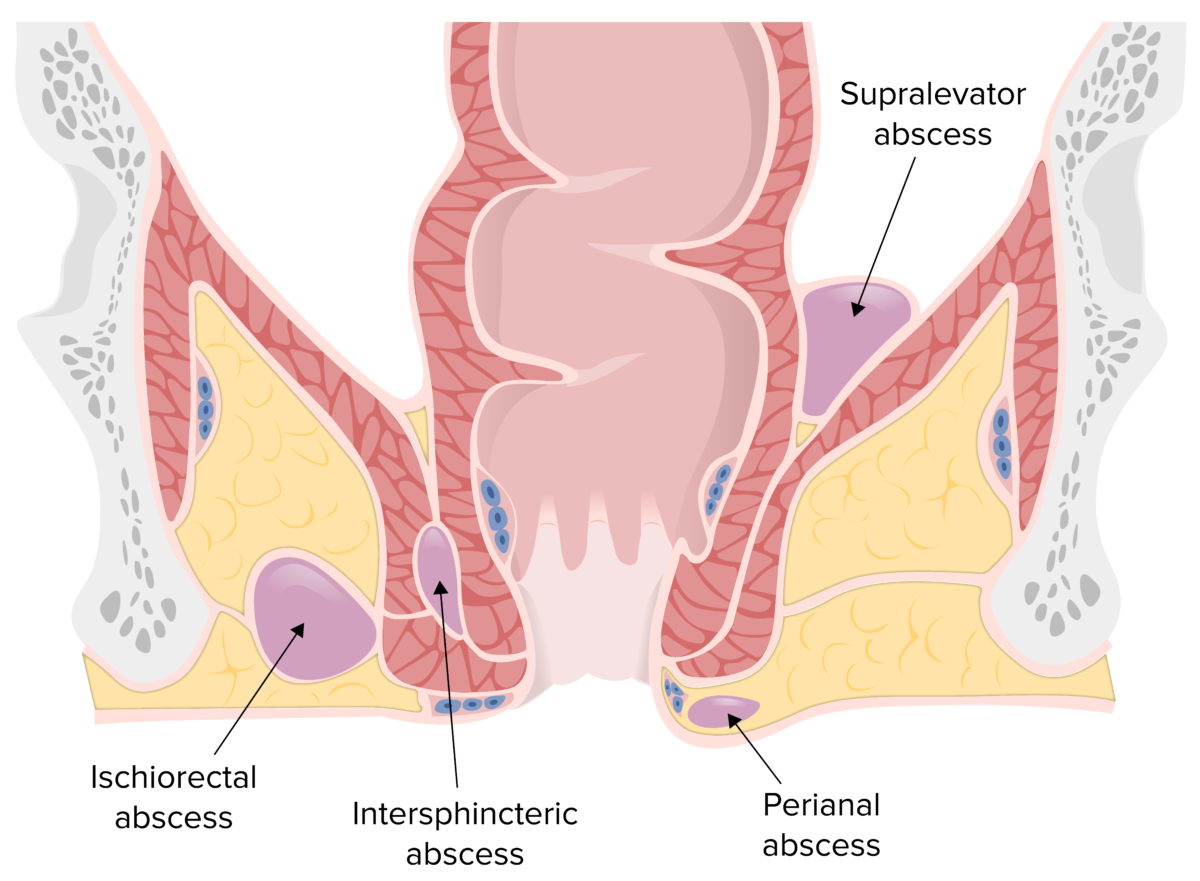
Locations of perianal, ischiorectal, intersphincteric, and supralevator abscesses
Image by Lecturio.The symptoms of a perirectal or perianal abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease can vary based on its location, but may include:

Perianal swelling, erythema, and drainage due to a perianal abscess
Image: “Localization of the perianal abscess” by Department of Urology, University Hospital Center, Fez, Morocco. License: CC BY 2.0The diagnosis of a perianal or ischiorectal Ischiorectal Perianal and Perirectal Abscess abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease is usually made clinically. However, CT, MRI, or ultrasonography may be useful for identifying:
Diagnostic approach:[2,4,5,9–11,14]
Note: The following diagnostic measures are summarized from different sources. Recommendations may vary based on practice location.
Note: The following surgical principles are based on practices in the United States. Specific recommendations may vary based on practice location (see article on UK and European management).
Postoperative care Postoperative care After any procedure performed in the operating room, all patients must undergo close observation at least in the recovery room. After larger procedures and for patients who require hospitalization, observation must continue on the surgical ward. The primary intent of this practice is the early detection of postoperative complications. Postoperative Care: [2,4,5,8]