Hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia is defined as a decreased serum sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia (sNa+) concentration less than 135 mEq/L. Serum sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia is the greatest contributor to plasma osmolality Plasma osmolality Volume Depletion and Dehydration, which is very tightly controlled via antidiuretic hormone Antidiuretic hormone Antidiuretic hormones released by the neurohypophysis of all vertebrates (structure varies with species) to regulate water balance and osmolarity. In general, vasopressin is a nonapeptide consisting of a six-amino-acid ring with a cysteine 1 to cysteine 6 disulfide bridge or an octapeptide containing a cystine. All mammals have arginine vasopressin except the pig with a lysine at position 8. Vasopressin, a vasoconstrictor, acts on the kidney collecting ducts to increase water reabsorption, increase blood volume and blood pressure. Hypernatremia (ADH) release from the hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus and by the thirst mechanism. The basic pathophysiology of all etiologies of hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia is an abnormal relative increase in total body water Total body water Body Fluid Compartments ( TBW TBW Body Fluid Compartments), which dilutes the total body sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia (TBNa+) concentration. The clinical presentation varies greatly, from asymptomatic to subtle cognitive deficits, seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures, and death. Management is guided by etiology, acuity, and duration of symptoms, usually involving oral fluid restriction or administration of IV fluids IV fluids Intravenous fluids are one of the most common interventions administered in medicine to approximate physiologic bodily fluids. Intravenous fluids are divided into 2 categories: crystalloid and colloid solutions. Intravenous fluids have a wide variety of indications, including intravascular volume expansion, electrolyte manipulation, and maintenance fluids. Intravenous Fluids that contain Na. Sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia must be replaced slowly, as overly rapid correction of hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia can lead to irreversible neurologic complications and death, known as osmotic demyelination Demyelination Multiple Sclerosis syndrome (ODS). Note: SIADH SIADH Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). SIADH is characterized by impaired water excretion leading to dilutional hyponatremia, which is mainly asymptomatic but may cause neurologic symptoms. S Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) has a separate clinical concept page.
Last updated: Mar 4, 2024
The etiology of hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia is determined by knowing the volume status Volume Status ACES and RUSH: Resuscitation Ultrasound Protocols, as well as the serum and urine osmolality Osmolality Plasma osmolality refers to the combined concentration of all solutes in the blood. Renal Sodium and Water Regulation.
Hypovolemic:
Euvolemic Euvolemic Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH):
Hypervolemic:
Hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia usually reflects an excess of total body water Total body water Body Fluid Compartments and not a deficiency in total body sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia.[2,4,7,8]
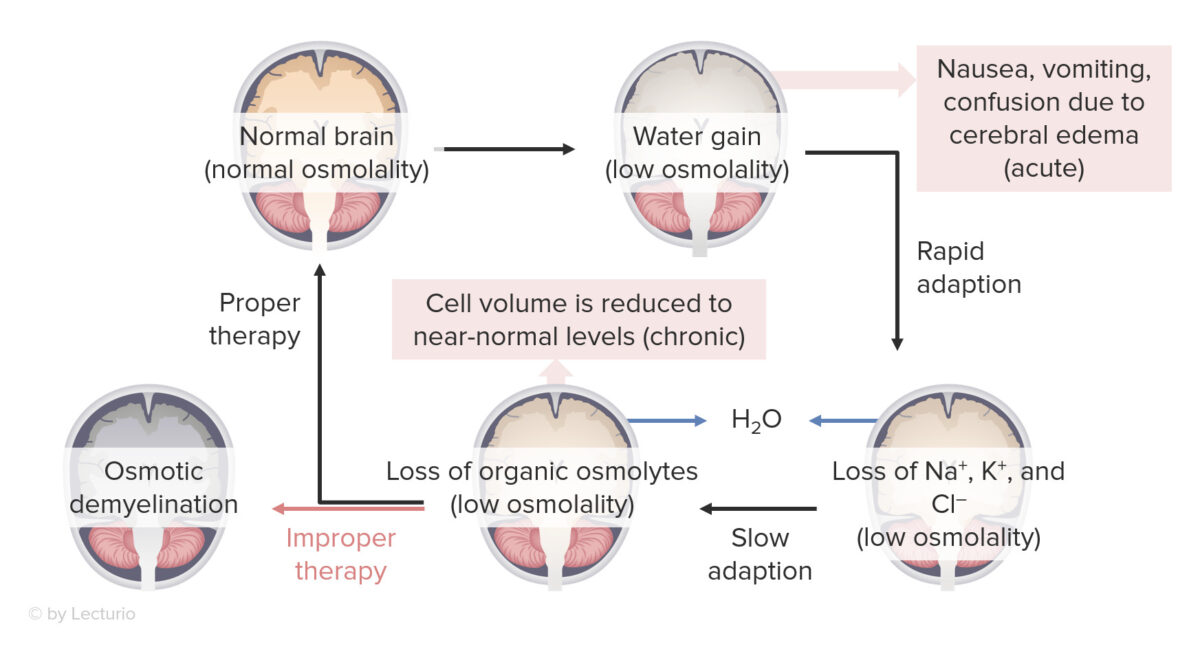
Effects of hyponatremia on the brain:
Osmotic demyelination syndrome can occur with overly rapid correction of severe hyponatremia (≤ 120 mEq/L).
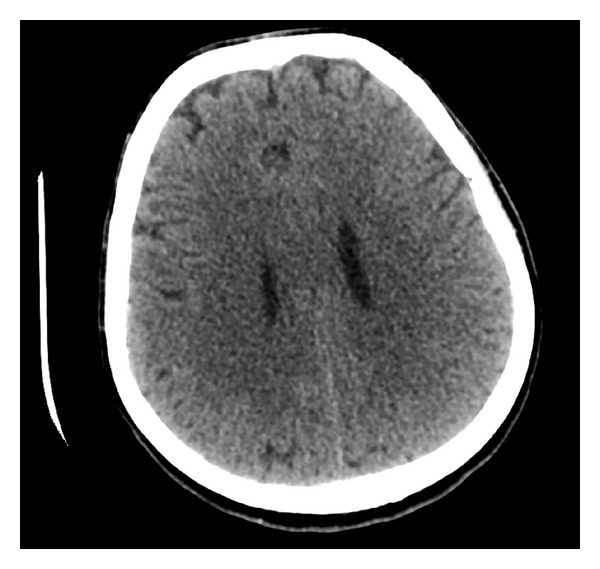
Supratentorial cerebral edema:
CT scan of a marathon runner with acute hyponatremia showing diffuse supratentorial cerebral edema
The 3 most important tests that need to be completed are:[6]
Note: If someone is presenting with severe symptoms, do not wait for diagnostic tests Diagnostic tests Diagnostic tests are important aspects in making a diagnosis. Some of the most important epidemiological values of diagnostic tests include sensitivity and specificity, false positives and false negatives, positive and negative predictive values, likelihood ratios, and pre-test and post-test probabilities. Epidemiological Values of Diagnostic Tests before starting urgent treatment.
Urinary sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia must be interpreted in the context of volume status Volume Status ACES and RUSH: Resuscitation Ultrasound Protocols.
Note: UNa cutoff values vary depending on the literature source (generally, ranges from 20 to 40 mEq/L).
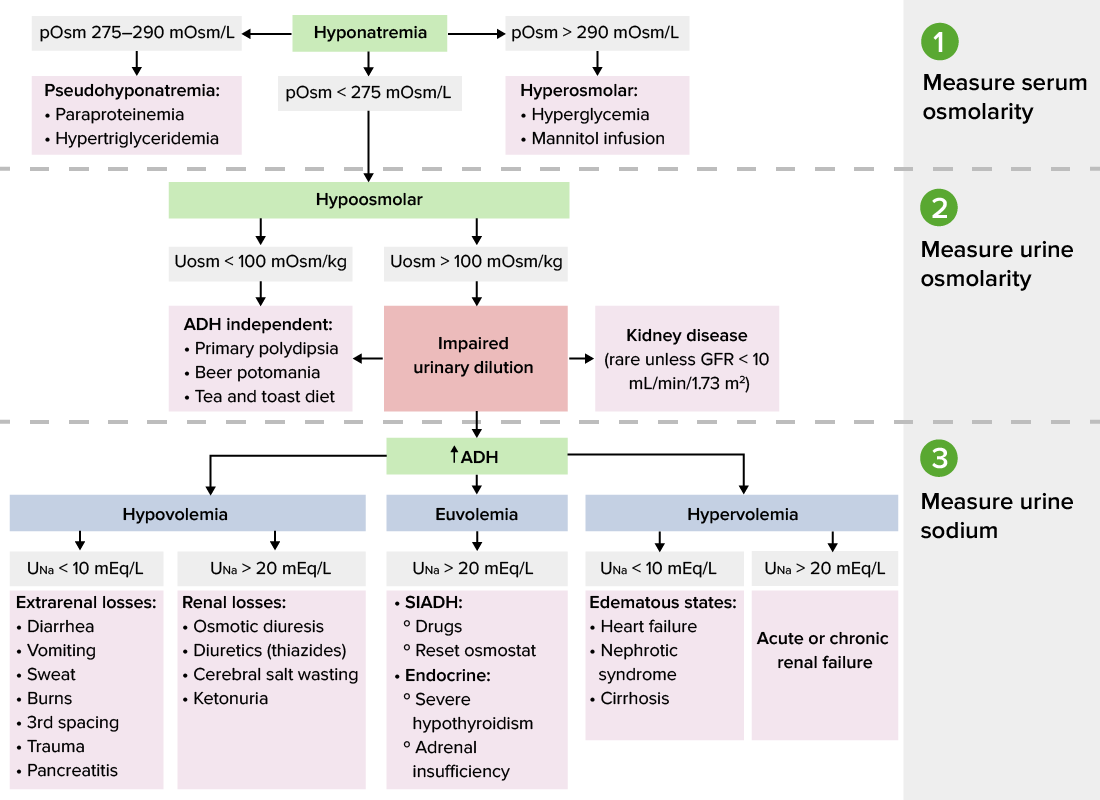
Diagnostic algorithm for hyponatremia
Image by Lecturio.Management varies depending on practice location. The following information was compiled from US, European, and UK literature and guidelines.[3,7,8]
Acuity and severity of symptoms are the primary determinants of this, and the aggressiveness and urgency of treatment will vary according to the risk assessment Risk assessment The qualitative or quantitative estimation of the likelihood of adverse effects that may result from exposure to specified health hazards or from the absence of beneficial influences. Preoperative Care.
Acuity:[7,11,18]
Symptom severity:[7,11]
Specific risk factors for ODS:[7]
General considerations:[7,11,12]
Management:[7,11–13,15]