The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). There are many causes of SIADH, including increased pituitary production of ADH (related to trauma, disease, or medications), ectopic production of ADH by a tumor, and hereditary disorders. SIADH is characterized by impaired water excretion, leading to dilutional hyponatremia. This condition is usually asymptomatic but may cause neurologic symptoms. SIADH should be suspected in any patient with hyponatremia, hypo-osmolality, and high urine osmolality.
Last updated: Mar 4, 2024
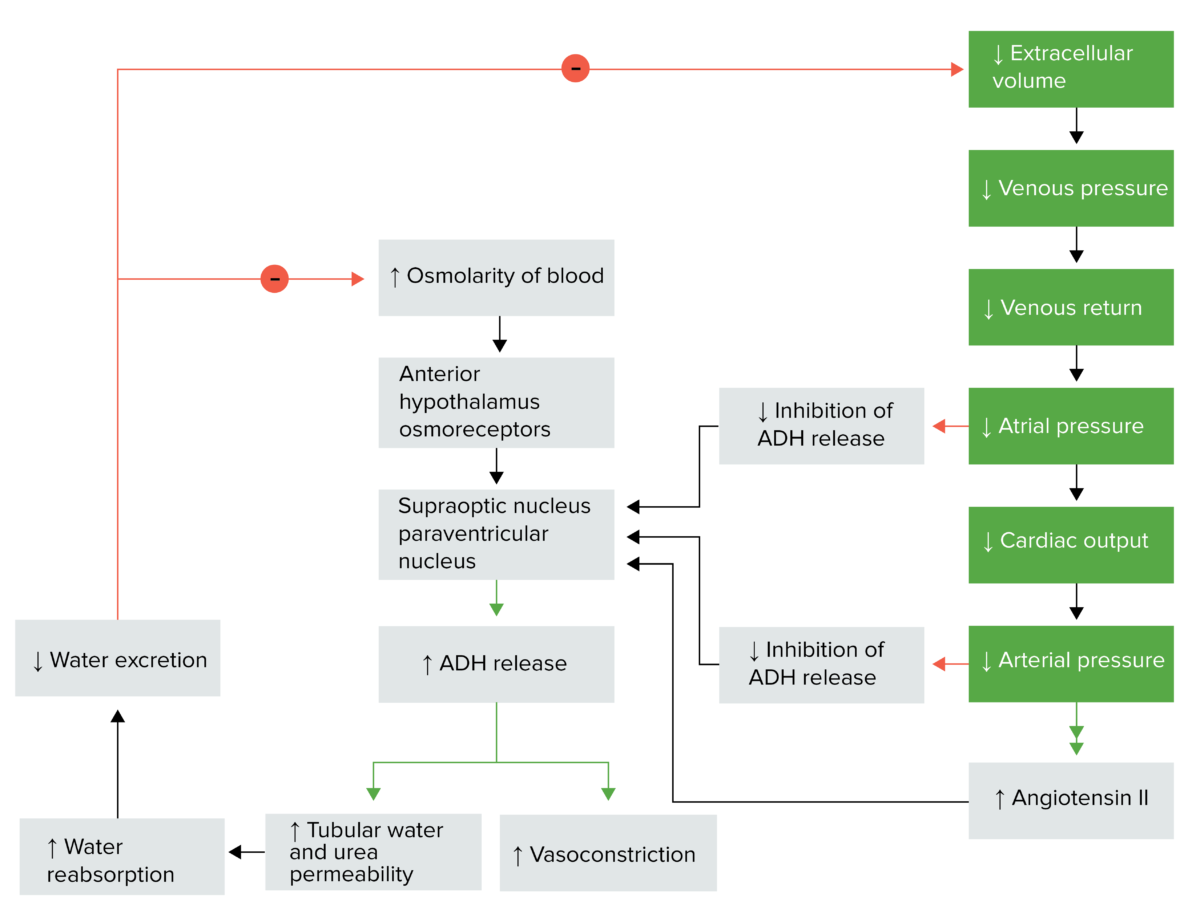
Antidiuretic hormone regulation
Image by Lecturio.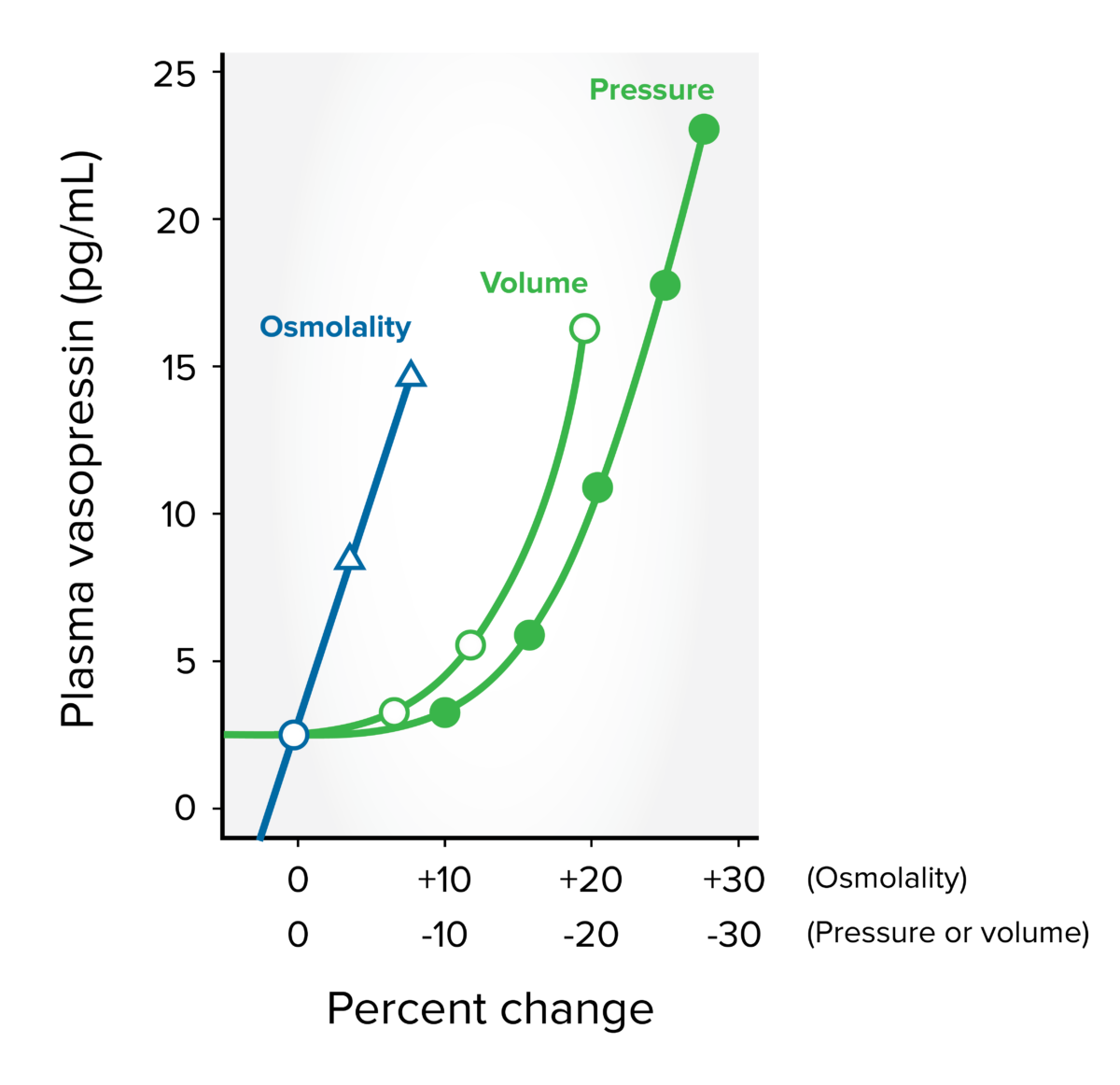
Antidiuretic hormone secretion: directly related to plasma osmolality, blood pressure, and blood volume
Image by Lecturio.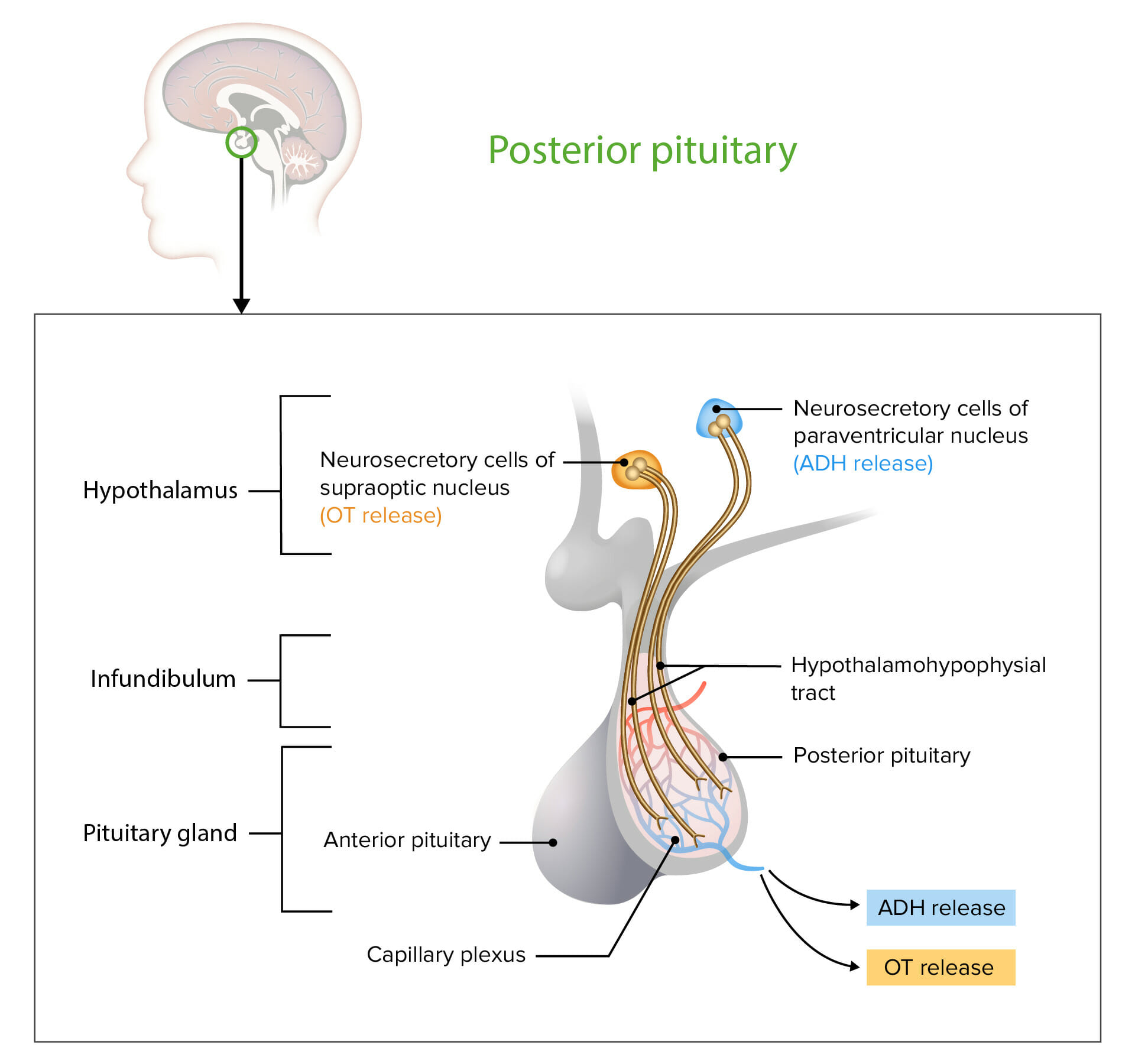
Neurosecretory cells in the hypothalamus release OT or ADH into the posterior lobe of the pituitary gland. The hormones are stored or released into the blood via the capillary plexus.
OT: oxytocin
ADH: antidiuretic hormone
ADH levels normally rise when plasma osmolality Plasma osmolality Volume Depletion and Dehydration exceeds 280 mOsm/kg; this mechanism is impaired with SIADH SIADH Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). SIADH is characterized by impaired water excretion leading to dilutional hyponatremia, which is mainly asymptomatic but may cause neurologic symptoms. S Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH).
The major causes of SIADH SIADH Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). SIADH is characterized by impaired water excretion leading to dilutional hyponatremia, which is mainly asymptomatic but may cause neurologic symptoms. S Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) are medications, malignancies, or infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease affecting the CNS or lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy.
| Major causes | Examples |
|---|---|
| Central nervous system Central nervous system The main information-processing organs of the nervous system, consisting of the brain, spinal cord, and meninges. Nervous System: Anatomy, Structure, and Classification causes |
|
| Neoplasms Neoplasms New abnormal growth of tissue. Malignant neoplasms show a greater degree of anaplasia and have the properties of invasion and metastasis, compared to benign neoplasms. Benign Bone Tumors |
|
| Pulmonary causes |
|
| Medications |
|
| Surgery |
|
Symptoms do not always correlate with the severity or the rapidity of onset of hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia, and some patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with profound hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia may be relatively asymptomatic.[1,7,10]
The following should be evaluated to determine an etiology for SIADH SIADH Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). SIADH is characterized by impaired water excretion leading to dilutional hyponatremia, which is mainly asymptomatic but may cause neurologic symptoms. S Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH):
Laboratory results showing hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia, serum hypo-osmolality, and urine hyperosmolality indicate only that ADH is acting on the kidney, not whether its secretion Secretion Coagulation Studies is “inappropriate.”
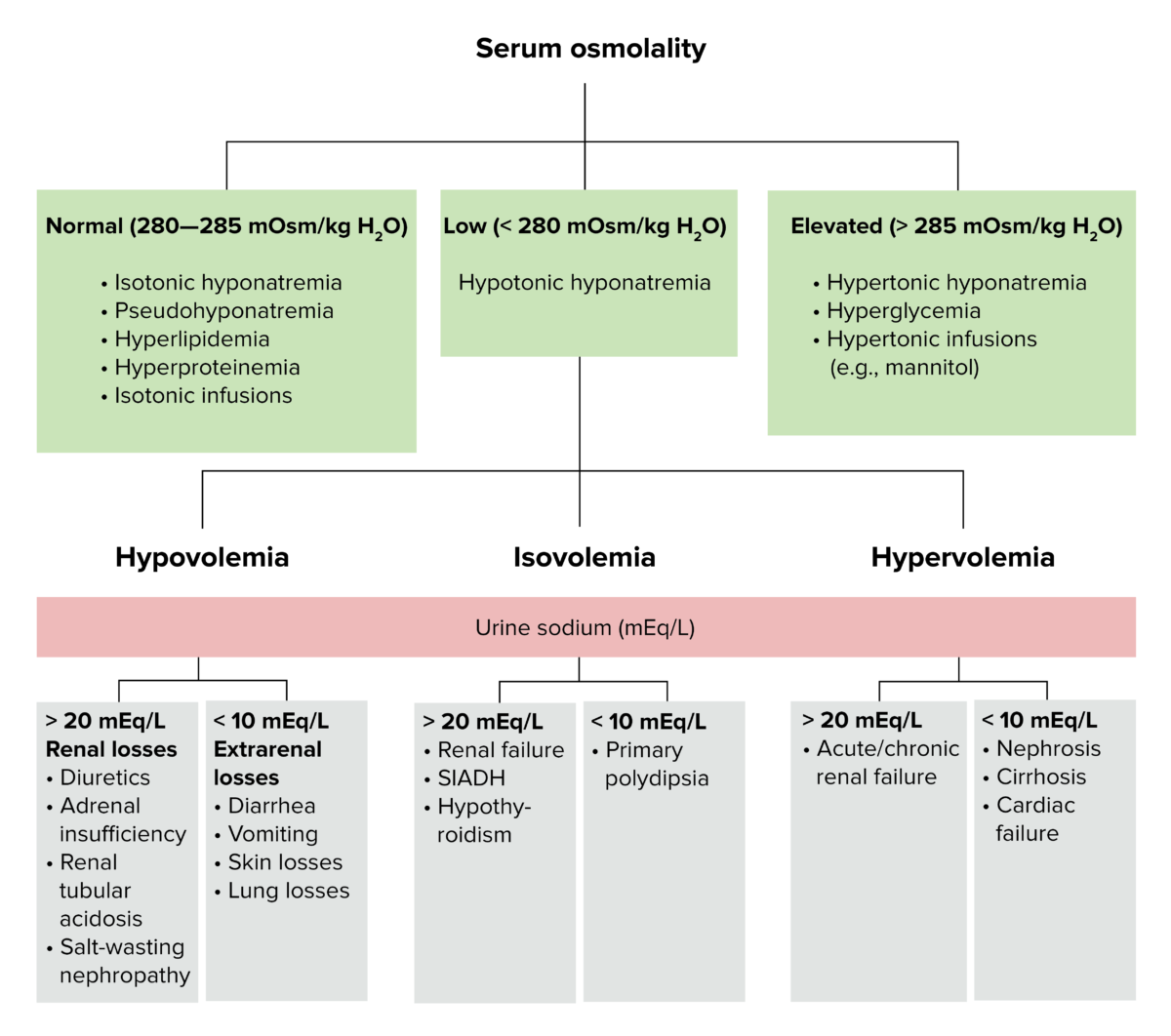
Diagnostic algorithm for volemic and sodium alterations
Image by Lecturio.Management may vary depending on practice location. The following information is derived from US and European literature and guidelines for adults. See local practice guidelines for additional information.
Overall, treatment includes correction of hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia and its underlying cause, if possible. Important note: Isotonic Isotonic Solutions having the same osmotic pressure as blood serum, or another solution with which they are compared. Renal Sodium and Water Regulation saline should be avoided, as it can worsen hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia in SIADH SIADH Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). SIADH is characterized by impaired water excretion leading to dilutional hyponatremia, which is mainly asymptomatic but may cause neurologic symptoms. S Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH).
This is the only definitive treatment for SIADH SIADH Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). SIADH is characterized by impaired water excretion leading to dilutional hyponatremia, which is mainly asymptomatic but may cause neurologic symptoms. S Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH), but it may not always be possible (e.g., incurable malignancy Malignancy Hemothorax, unknown etiology).
General considerations:[1,6,10,13–15]
Acute (< 48 hours) severe hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia (< 130 mOsm/kg):[1,8,10,13–15,17–19]
Chronic hyponatremia Chronic Hyponatremia Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) (> 48 hours or unknown duration):[8,10,14,15,17]
The following medications may be needed to increase serum Na+ and lower urine osmolality Osmolality Plasma osmolality refers to the combined concentration of all solutes in the blood. Renal Sodium and Water Regulation, but they should be started only under the guidance of a specialist.
Loop diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication:[1,13]
Oral solute tablets:[1,14]
Vasopressin receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors antagonists (vaptans):[1,10,13,16]
When overcorrection Overcorrection Volume Depletion and Dehydration occurs, Na+ can be decreased with administration of:
The differential diagnosis of SIADH SIADH Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). SIADH is characterized by impaired water excretion leading to dilutional hyponatremia, which is mainly asymptomatic but may cause neurologic symptoms. S Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) includes other hyponatremic conditions: