Mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) ( MS MS Multiple sclerosis (MS) is a chronic inflammatory autoimmune disease that leads to demyelination of the nerves in the CNS. Young women are more predominantly affected by this most common demyelinating condition. Multiple Sclerosis) is the narrowing of the mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy (MV) orifice, leading to obstructed blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure from the left atrium (LA) to the left ventricle (LV). Mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) is most commonly due to rheumatic heart disease Rheumatic Heart Disease Cardiac manifestation of systemic rheumatological conditions, such as rheumatic fever. Rheumatic heart disease can involve any part the heart, most often the heart valves and the endocardium. Rheumatic Fever. Mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) leads to impaired LV diastolic filling, increased LA pressure, and LA dilation, which can result in atrial fibrillation Atrial fibrillation Atrial fibrillation (AF or Afib) is a supraventricular tachyarrhythmia and the most common kind of arrhythmia. It is caused by rapid, uncontrolled atrial contractions and uncoordinated ventricular responses. Atrial Fibrillation, pulmonary congestion, pulmonary hypertension Pulmonary Hypertension Pulmonary hypertension (PH) or pulmonary arterial hypertension (PAH) is characterized by elevated pulmonary arterial pressure, which can lead to chronic progressive right heart failure. Pulmonary hypertension is grouped into 5 categories based on etiology, which include primary PAH, and PH due to cardiac disease, lung or hypoxic disease, chronic thromboembolic disease, and multifactorial or unclear etiologies. Pulmonary Hypertension, and right heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR). Symptoms include exertional dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, orthopnea Orthopnea Pulmonary Edema, palpitations Palpitations Ebstein’s Anomaly, fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia, and hoarseness Hoarseness An unnaturally deep or rough quality of voice. Parapharyngeal Abscess. Physical examination will demonstrate an opening snap, followed by a rumbling diastolic murmur. An echocardiogram Echocardiogram Transposition of the Great Arteries is used for diagnosis. Treatment includes sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia restriction, diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication, atrial fibrillation Atrial fibrillation Atrial fibrillation (AF or Afib) is a supraventricular tachyarrhythmia and the most common kind of arrhythmia. It is caused by rapid, uncontrolled atrial contractions and uncoordinated ventricular responses. Atrial Fibrillation management, possible anticoagulation Anticoagulation Pulmonary Hypertension Drugs, and percutaneous commissurotomy or surgery.
Last updated: May 16, 2024
Mitral stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) ( MS MS Multiple sclerosis (MS) is a chronic inflammatory autoimmune disease that leads to demyelination of the nerves in the CNS. Young women are more predominantly affected by this most common demyelinating condition. Multiple Sclerosis) is the narrowing of the mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy (MV) orifice, which impedes blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure from the left atrium (LA) into the left ventricle (LV) during diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle.
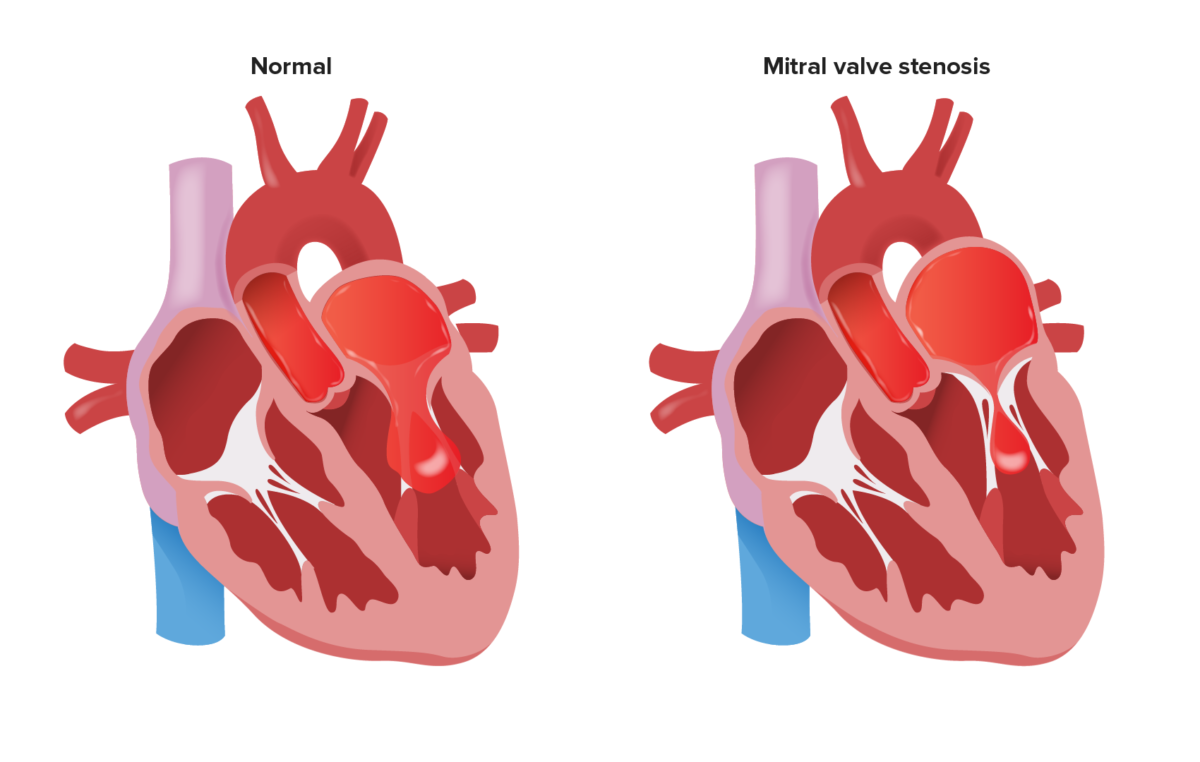
Obstruction of blood flow from the LA to the LV during diastole due to a stenotic MV
Image by Lecturio.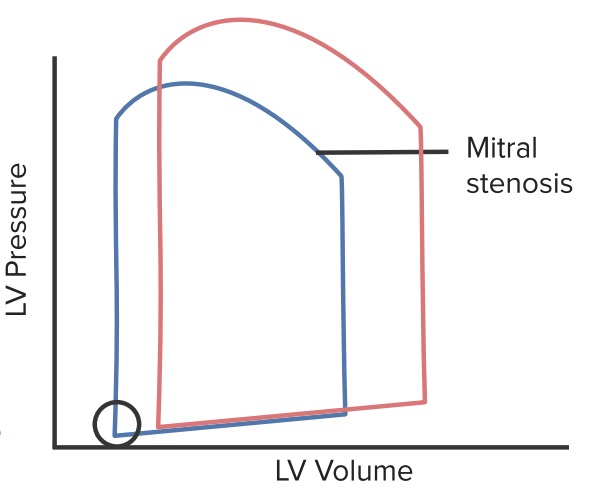
Normal pressure-volume loop (red line) compared to that of MS (blue line): Mitral stenosis impairs LV filling, so there is a decrease in end-diastolic volume. This leads to an overall decrease in cardiac output and stroke volume. The circle represents the opening of the MV, and LV filling pressures that may be slightly decreased in the setting of a stenotic valve.
Image by Lecturio.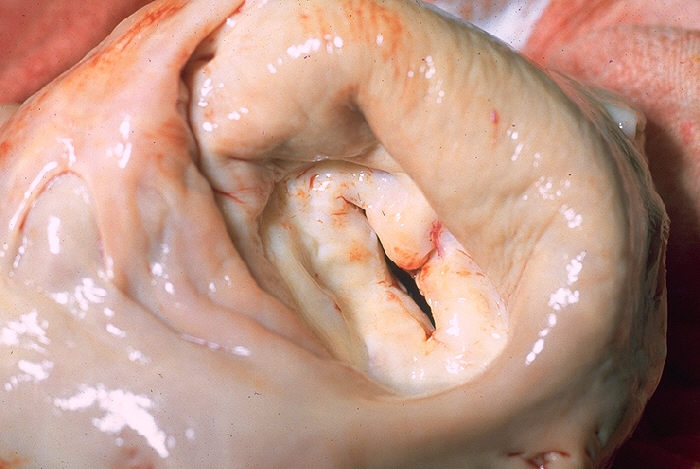
A gross pathology specimen of a stenotic MV: Notice the thickened valve leaflets and narrow valve opening.
Image: “Mitral stenosis, gross pathology” by CDC/Dr. Edwin P. Ewing, Jr. License: Public domain.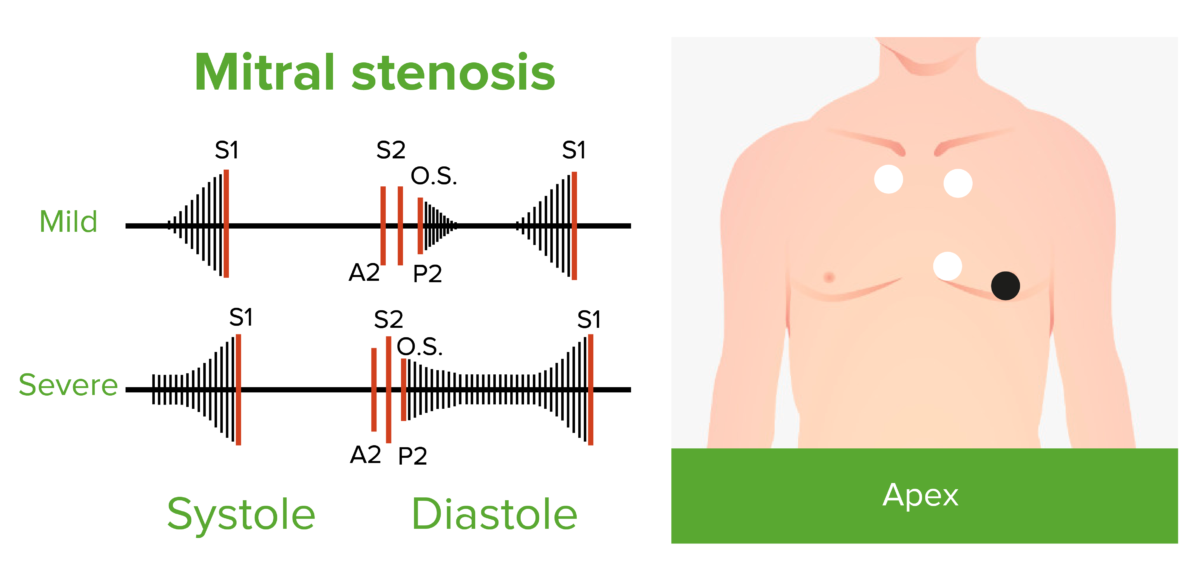
Diastolic filling and rumbling murmur of mild and severe mitral stenosis
The mid-diastolic murmur starts after the opening snap (O.S.). The presystolic murmur is due to atrial contraction (and absent in atrial fibrillation).
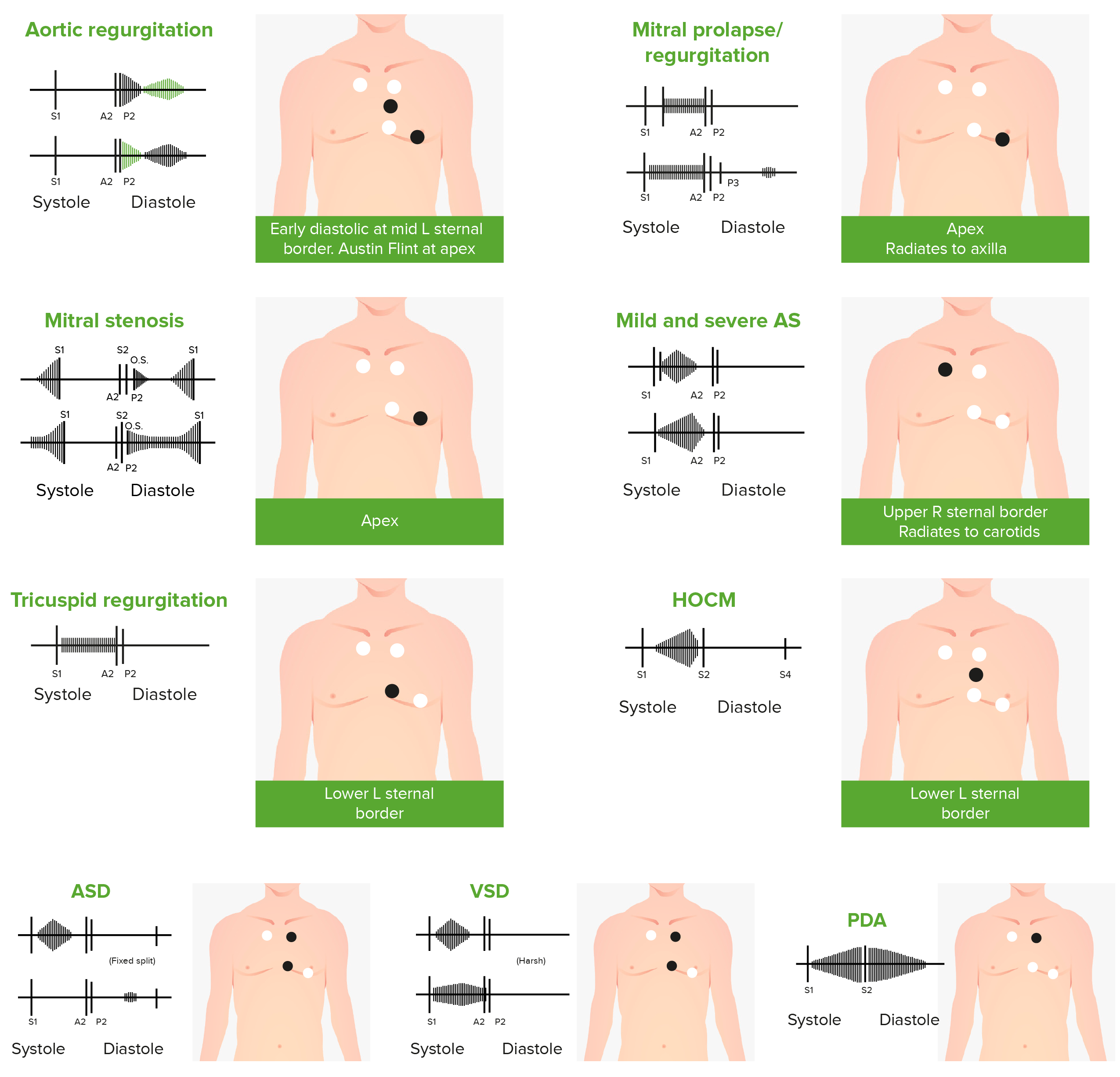
Phonocardiograms of abnormal heart sounds caused by the following cardiac defects:
aortic regurgitation, mitral valve prolapse, mitral stenosis (MS), aortic stenosis (AS), tricuspid regurgitation, hypertrophic obstructive cardiomyopathy (HOCM), atrial septal defect (ASD), ventricular septal defect (VSD), and patent ductus arteriosus (PDA)
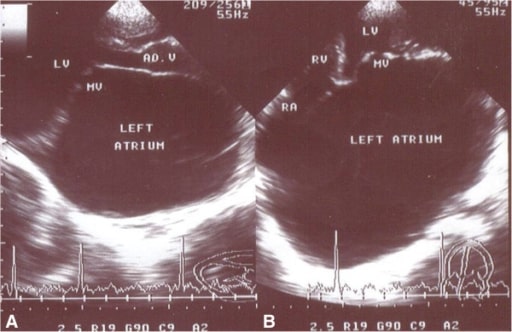
Echocardiography frames in the parasternal long axis (A) and apical 4-chamber (B) views from a patient with severe MS (MVA = 0.84 cm2) and mild regurgitation, showing a giant left atrium (GLA)
MV: mitral valve
LV: left ventricle
RV: right ventricle
RA: right atrium
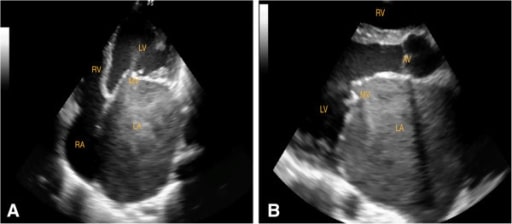
Echocardiographic frames from a patient with rheumatic heart disease and severe MS (MVA 0.51 cm2), showing an enlarged LA and echo contrast in the LA. You can see some movement of the contrast through the narrowed MV.
A: apical 4-chamber view (diastole)
B: parasternal long-axis view (diastole)
LA: left atrium
LV: left ventricle
RV: right ventricle
MV: mitral valve
AV: aortic valve

A cMRI assessing MS. Top: diastolic frame from a LV outflow tract view demonstrating the slice position for subsequent imaging (dashed line);
Bottom: resulting modified short-axis view through the MV in diastole, showing the narrowed mitral orifice (arrow)

Percutaneous mitral valvotomy in a case of situs inversus totalis and juvenile rheumatic critical MS. A: Accura balloon entering into the LV; B: distal inflation of the balloon; C: mitral valve dilation
Image: “Accura balloon” by the Department of Cardiology, LPS Institute of Cardiology, G.S.V.M. Medical College, Kanpur, Uttar Pradesh 208002, India. License: CC BY 2.0.