The elimination Elimination The initial damage and destruction of tumor cells by innate and adaptive immunity. Completion of the phase means no cancer growth. Cancer Immunotherapy disorders that most commonly occur in childhood are enuresis ( urinary incontinence Urinary incontinence Urinary incontinence (UI) is involuntary loss of bladder control or unintentional voiding, which represents a hygienic or social problem to the patient. Urinary incontinence is a symptom, a sign, and a disorder. The 5 types of UI include stress, urge, mixed, overflow, and functional. Urinary Incontinence) and encopresis ( fecal incontinence Fecal incontinence Failure of voluntary control of the anal sphincters, with involuntary passage of feces and flatus. Pediatric Constipation in inappropriate situations). Enuresis is usually diagnosed when children > 5 years of age continue to wet the bed. Enuresis can occur both in the daytime (diurnal) and at night (nocturnal). The incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency of nocturnal enuresis spontaneously resolves at a rate of approximately 15% per year. Management of nocturnal enuresis primarily consists of behavior and lifestyle modifications but can include desmopressin Desmopressin Hemophilia. Encopresis is most often secondary to underlying constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation, although emotional stressors may also be involved. Management is primarily through treating constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation.
Last updated: Mar 6, 2023
The primary goal of assessment is to determine if an underlying medical condition is present that could explain the incontinence (e.g., constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus insipidus).
The diagnosis of enuresis is primarily through history, physical examination, and urinalysis Urinalysis Examination of urine by chemical, physical, or microscopic means. Routine urinalysis usually includes performing chemical screening tests, determining specific gravity, observing any unusual color or odor, screening for bacteriuria, and examining the sediment microscopically. Urinary Tract Infections (UTIs) in Children.
Encopresis is the involuntary or unintentional passage of feces in inappropriate situations in children older than 4 years of age in the absence of neuromuscular disease.
| Type | Explanation |
|---|---|
| Retentive | With constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation and secondary overflow and leakage around obstruction; more common |
| Non-retentive | Without constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation |
| Primary | Seen in boys from infancy; often associated with global developmental delay and enuresis |
| Secondary | Seen in children after successful toilet training; often functional in nature, marked by a higher level of stressors and psychological disorders |
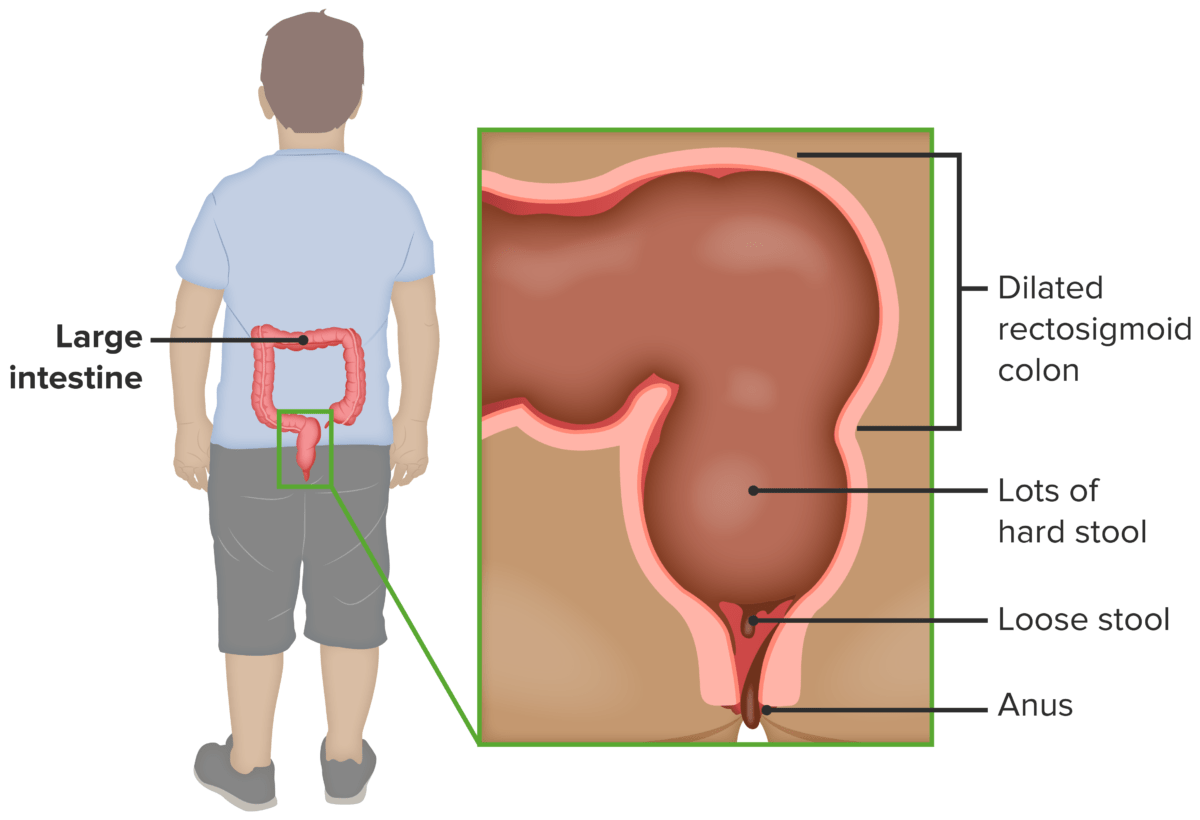
In retentive encopresis, underlying constipation can lead to overflow incontinence.
Image by Lecturio.A careful history is important to determine if there is an underlying condition or if there are any recent stressors in the child’s life.
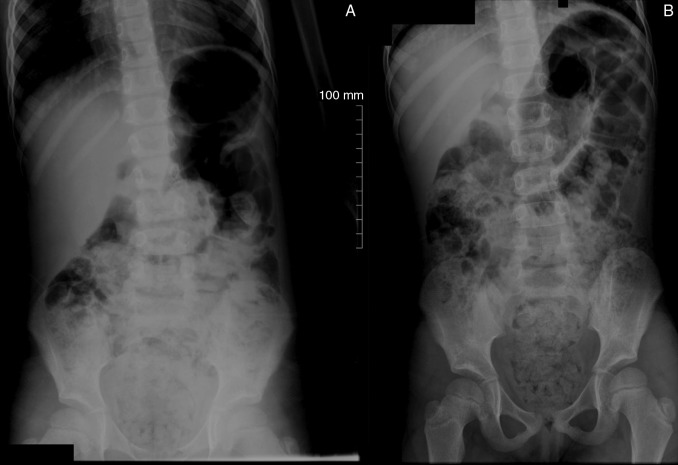
Abdominal X-rays in the standing (A) and supine (B) position, showing a large amount of stool in the ascending and descending colon, sigmoid, and rectum. Dilation in the rectosigmoid segment, secondary to the presence of stool, can also be observed.
Image: “Radiografias de abdome em posição ortostática” by Traslaviña, G. A., Del Ciampo, L. A., & Ferraz, I. S. License: CC BY 4.0Urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infection ( UTI UTI Urinary tract infections (UTIs) represent a wide spectrum of diseases, from self-limiting simple cystitis to severe pyelonephritis that can result in sepsis and death. Urinary tract infections are most commonly caused by Escherichia coli, but may also be caused by other bacteria and fungi. Urinary Tract Infections (UTIs)): infection of the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy by a pathogen, usually fecal Escherichia coli. In children, UTI UTI Urinary tract infections (UTIs) represent a wide spectrum of diseases, from self-limiting simple cystitis to severe pyelonephritis that can result in sepsis and death. Urinary tract infections are most commonly caused by Escherichia coli, but may also be caused by other bacteria and fungi. Urinary Tract Infections (UTIs) may present as cystitis Cystitis Inflammation of the urinary bladder, either from bacterial or non-bacterial causes. Cystitis is usually associated with painful urination (dysuria), increased frequency, urgency, and suprapubic pain. Urinary Tract Infections (UTIs), pyelonephritis Pyelonephritis Pyelonephritis is infection affecting the renal pelvis and the renal parenchyma. This condition arises mostly as a complication of bladder infection that ascends to the upper urinary tract. Pyelonephritis can be acute or chronic (which results from persistent or chronic infections). Typical acute symptoms are flank pain, fever, and nausea with vomiting. T Pyelonephritis and Perinephric Abscess, or asymptomatic bacteriuria Asymptomatic Bacteriuria Urinary Tract Infections (UTIs) in Children. Dysfunctional voiding (neurogenic bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess) and bowel dysfunction ( pediatric constipation Pediatric constipation Constipation is a common complaint in children that is relatively defined for individual age groups based on the frequency and difficulty of defecation and stool consistency. The majority of constipation cases are functional or non-organic. Clinical presentation may vary, from insufficient evacuation noted by the parents, to complaints of abdominal pain, to secondary incontinence. Pediatric Constipation) are among the most common causes.