Knee pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is a common presentation to primary care physicians Physicians Individuals licensed to practice medicine. Clinician–Patient Relationship. The diagnosis can be challenging as the pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways may arise from the joint, surrounding tissues, or referred to the joint from distant structures. The differential diagnosis of knee pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is broad and categorizing the various diagnoses related to the timing (acute or chronic) is useful. A thorough understanding of pertinent anatomy, appropriate physical examination, and common problems of the knee joint Knee joint The knee joint is made up of the articulations between the femur, tibia, and patella bones, and is one of the largest and most complex joints of the human body. The knee is classified as a synovial hinge joint, which primarily allows for flexion and extension with a more limited degree of translation and rotation. Knee Joint: Anatomy are essential for diagnosis and proper management of knee pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Exercise-based therapy is often the 1st-line management of many knee disorders, but surgical intervention is warranted for specific diagnoses.
Last updated: Mar 29, 2023
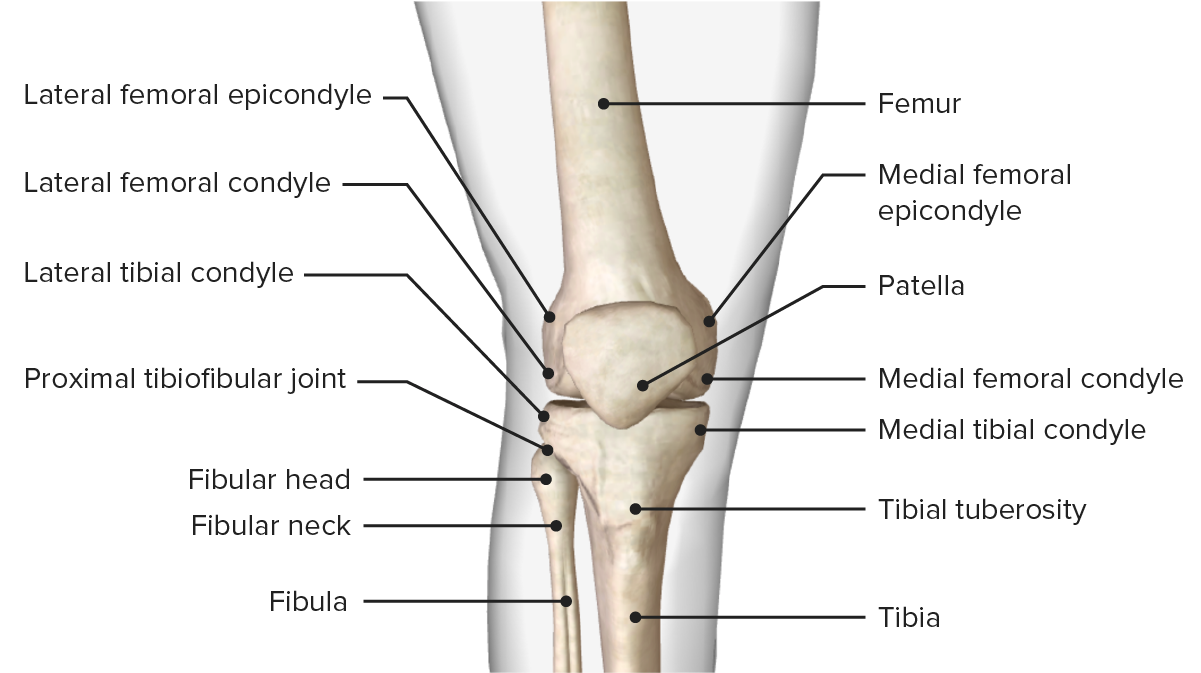
The bony structure of the knee joint
Image by BioDigital, edited by Lecturio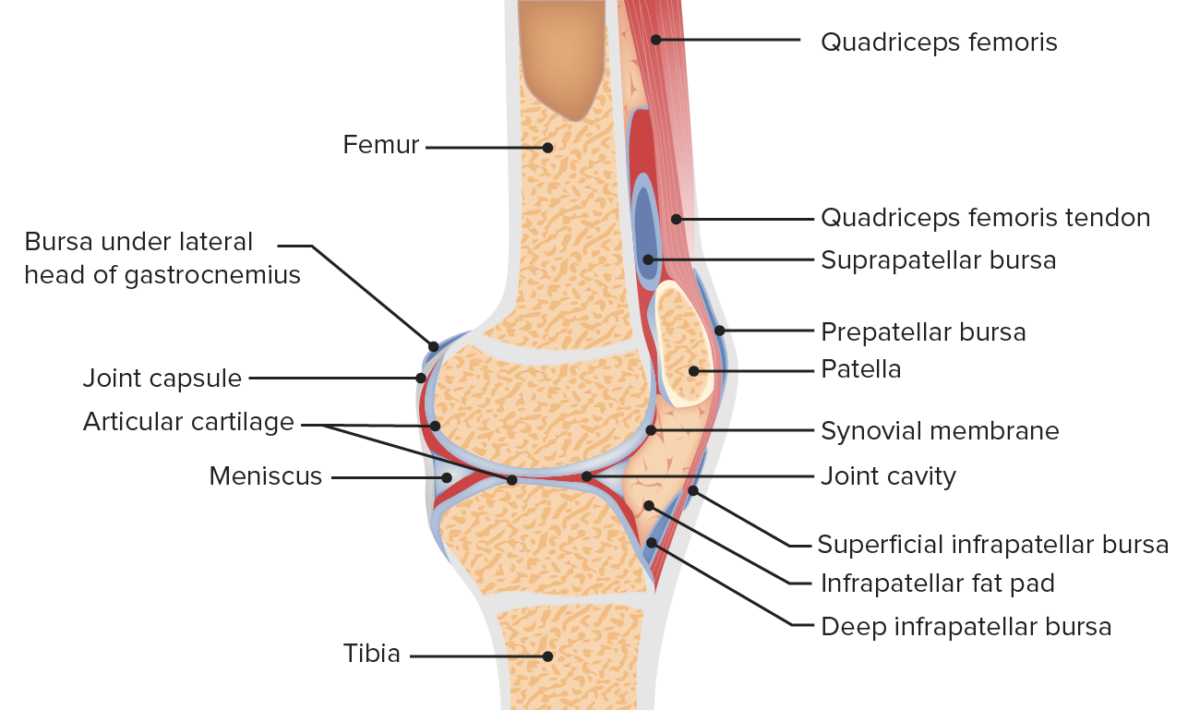
Sagittal view of the anatomy of the patellofemoral joint
Image by Lecturio.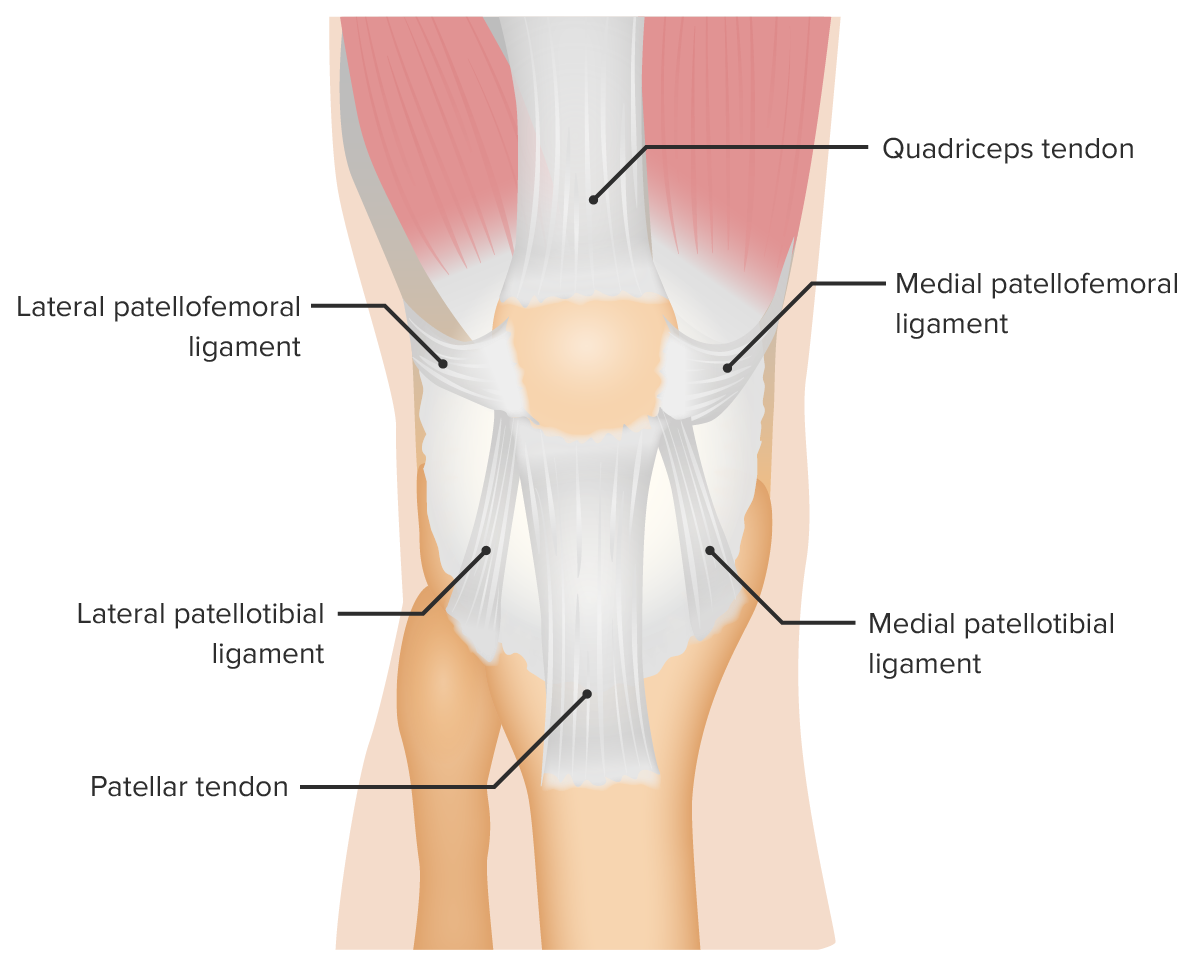
Anterior view of the supporting ligaments of the patellofemoral joint
Image by Lecturio.Obtaining a clear history is essential to making the correct diagnosis and guiding the examination:
The exam is directed by the duration and type of injury (acute or chronic) and the age of the individual. Comparison of the healthy knee is important:

Total knee replacement scar noted on examination of the patient
Image: “Total knee replacement scar” by Dave Haygarth; Geeky Medics. License: CC BY 2.0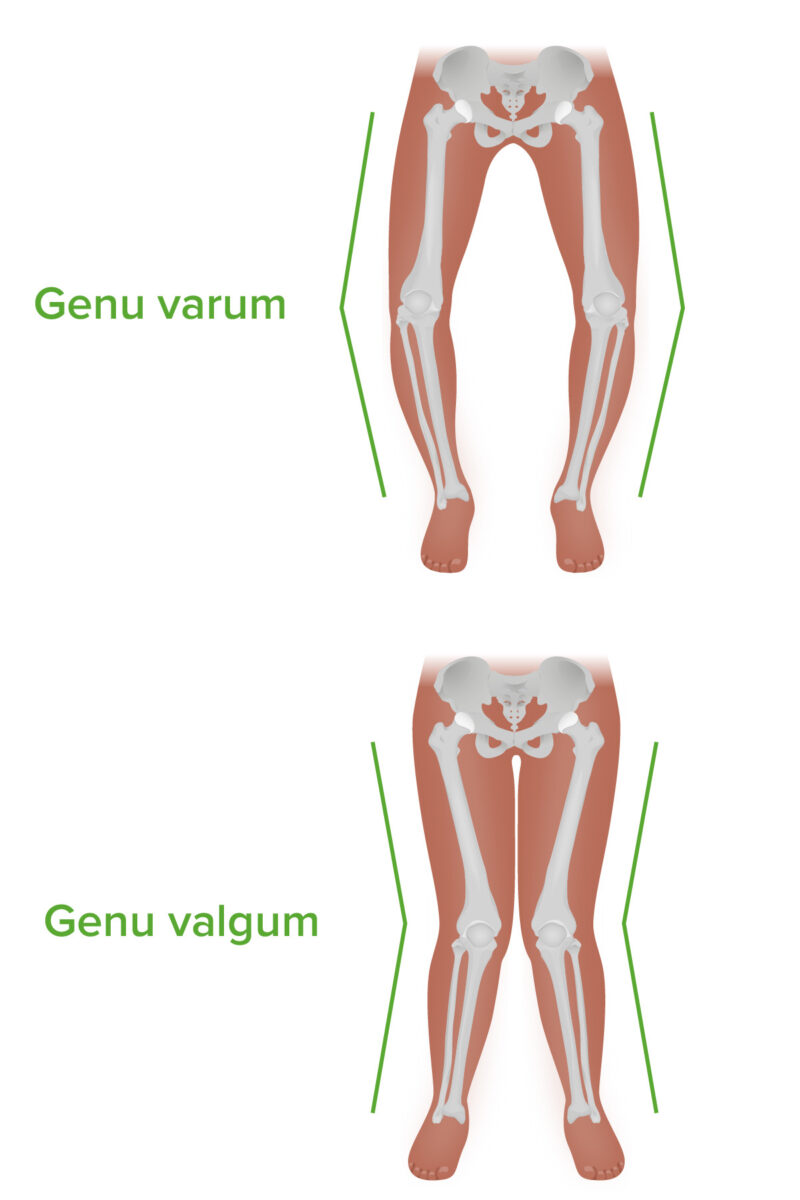
Genu varum and genu valgum: Note the difference in angulation in the coronal plane.
Image by Lecturio. License: CC BY-NC-SA 4.0| Injury | Maneuver |
|---|---|
| ACL ACL A strong ligament of the knee that originates from the posteromedial portion of the lateral condyle of the femur, passes anteriorly and inferiorly between the condyles, and attaches to the depression in front of the intercondylar eminence of the tibia. Knee Joint: Anatomy injury |
|
| PCL PCL A strong ligament of the knee that originates from the anterolateral surface of the medial condyle of the femur, passes posteriorly and inferiorly between the condyles, and attaches to the posterior intercondylar area of the tibia. Knee Joint: Anatomy injury |
|
| MCL MCL Knee Joint: Anatomy injury | Valgus stress test for
MCL
MCL
Knee Joint: Anatomy instability:
|
| LCL injury |
Varus stress test
Varus Stress Test
Knee Ligament Injuries for lateral instability:
|
| Meniscal tear |
|
| ITBS |
|
| PFPS |
|
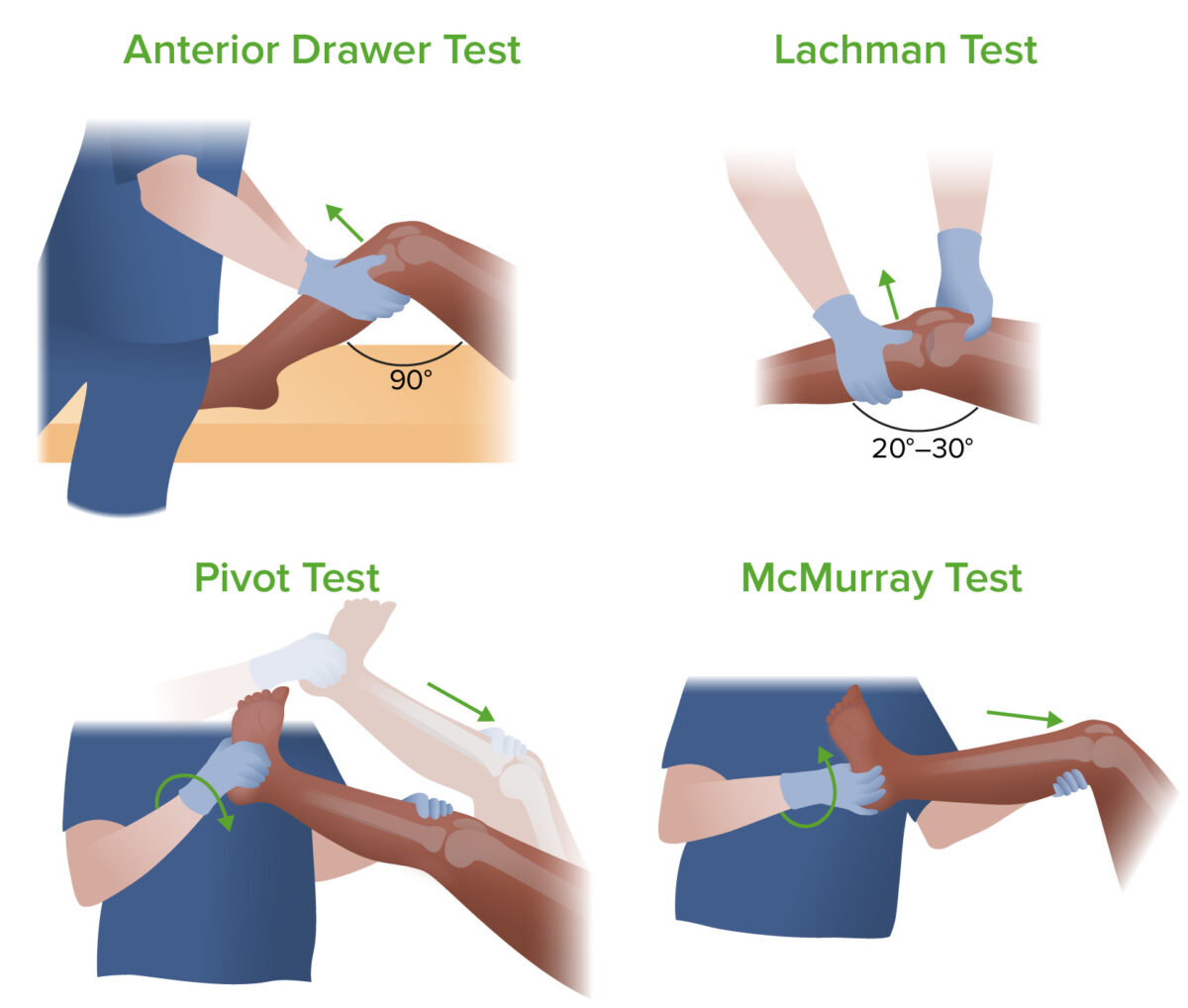
Four exams to determine the cause of knee pain: anterior drawer test, Lachman test, pivot test, and McMurray test
Image by Lecturio.
Valgus and varus stress tests
Image: “Valgus and varus stress tests” by Rossi R, Dettoni F, Bruzzone M, Cottino U, D’Elicio DG, Bonasia DE. License: CC BY 2.0
The Muller test (also known as the quadriceps active test)
Image: “Quadriceps Active Test” by Rossi R, Dettoni F, Bruzzone M, Cottino U, D’Elicio DG, Bonasia DE. License: CC BY 2.0
MRI of the right knee revealing an intra-articular, bucket-handle medial meniscus tear with displaced fragment located in the intercondylar notch
Image: “Coronal MRI of the right knee” by Ahmed Ali R, McKay S. License: CC BY 3.0
X-ray demonstrating medial joint space narrowing in a meniscal tear
Image: “Complete medial femorotibial thinning” by Sylvain Steinmetz et al. License: CC BY 4.0
X-ray and MRI images of valgus deformity:
a severe case of genu valgum of the left knee following bone cancer treatment
The assessment of knee pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is challenging. One approach to the differential diagnosis is to group the various conditions based on the acuteness of the presentation, the presence or absence of effusion, and the precipitating activities.
| Condition | Mechanism | Features | Diagnosis |
|---|---|---|---|
| ACL ACL A strong ligament of the knee that originates from the posteromedial portion of the lateral condyle of the femur, passes anteriorly and inferiorly between the condyles, and attaches to the depression in front of the intercondylar eminence of the tibia. Knee Joint: Anatomy tear |
|
|
|
| PCL PCL A strong ligament of the knee that originates from the anterolateral surface of the medial condyle of the femur, passes posteriorly and inferiorly between the condyles, and attaches to the posterior intercondylar area of the tibia. Knee Joint: Anatomy tear |
|
|
|
| Meniscus tear Meniscus tear The menisci are fibrocartilaginous wedge-shaped structures between the distal femur and proximal tibia that stabilize and dissipate weight-bearing forces at the knee joint. A meniscus tear is an injury to the meniscus caused by rotational or shearing forces across the tibiofemoral joint. Meniscus Tear |
|
|
|
| Patellar dislocation | Pivoting or sudden change in direction |
|
|
| Patellar ligament Patellar ligament A band of fibrous tissue that attaches the apex of the patella to the lower part of the tubercle of the tibia. The ligament is actually the caudal continuation of the common tendon of the quadriceps femoris. The patella is embedded in that tendon. As such, the patellar ligament can be thought of as connecting the quadriceps femoris tendon to the tibia, and therefore it is sometimes called the patellar tendon. Osgood-Schlatter Disease tear |
|
|
|
| Quadriceps tendon Quadriceps tendon Knee Joint: Anatomy tear |
|
|
|
| Intra-articular fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures |
|
|
|
| Condition | Mechanism | Features | Diagnosis |
|---|---|---|---|
| MCL MCL Knee Joint: Anatomy sprain |
|
|
|
| LCL sprain | Varus force to the knee |
|
|
| Condition | Features |
|---|---|
| Knee osteoarthritis Osteoarthritis Osteoarthritis (OA) is the most common form of arthritis, and is due to cartilage destruction and changes of the subchondral bone. The risk of developing this disorder increases with age, obesity, and repetitive joint use or trauma. Patients develop gradual joint pain, stiffness lasting < 30 minutes, and decreased range of motion. Osteoarthritis |
|
| Crystal arthropathy Arthropathy Osteoarthritis |
|
| Septic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis |
|
| Rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis |
|
| Condition | Features |
|---|---|
| Anterior knee pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | |
| Tibial tubercle Tibial Tubercle Osgood-Schlatter Disease apophysitis Apophysitis Osgood-Schlatter Disease (Osgood-Schlatter) |
|
| SCFE SCFE Slipped capital femoral epiphysis (SCFE) is an orthopedic disorder of early adolescence characterized by the pathologic “slipping” or displacement of the femoral head, or epiphysis, on the femoral neck. Slipped Capital Femoral Epiphysis |
|
| Prepatellar bursitis |
|
| Patellofemoral pain syndrome Patellofemoral pain syndrome A syndrome characterized by retropatellar or peripatellar pain resulting from physical and biochemical changes in the patellofemoral joint. The pain is most prominent when ascending or descending stairs, squatting, or sitting with flexed knees. There is a lack of consensus on the etiology and treatment. The syndrome is often confused with (or accompanied by) chondromalacia patellae, the latter describing a pathological condition of the cartilage and not a syndrome. Examination of the Lower Limbs |
|
| Medial knee pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | |
| Pes PES Removal of plasma and replacement with various fluids, e.g., fresh frozen plasma, plasma protein fractions (ppf), albumin preparations, dextran solutions, saline. Used in treatment of autoimmune diseases, immune complex diseases, diseases of excess plasma factors, and other conditions. Thrombotic Thrombocytopenic Purpura anserine bursitis |
|
| Lateral knee pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | |
| ITBS |
|
| Posterior knee pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | |
| Popliteal (Baker) cyst |
|
| Condition | Management |
|---|---|
| ACL ACL A strong ligament of the knee that originates from the posteromedial portion of the lateral condyle of the femur, passes anteriorly and inferiorly between the condyles, and attaches to the depression in front of the intercondylar eminence of the tibia. Knee Joint: Anatomy injury |
|
| PCL PCL A strong ligament of the knee that originates from the anterolateral surface of the medial condyle of the femur, passes posteriorly and inferiorly between the condyles, and attaches to the posterior intercondylar area of the tibia. Knee Joint: Anatomy injuries |
|
| Meniscal injuries |
|
| MCL MCL Knee Joint: Anatomy injury |
|
| Osteoarthritis Osteoarthritis Osteoarthritis (OA) is the most common form of arthritis, and is due to cartilage destruction and changes of the subchondral bone. The risk of developing this disorder increases with age, obesity, and repetitive joint use or trauma. Patients develop gradual joint pain, stiffness lasting < 30 minutes, and decreased range of motion. Osteoarthritis |
|
| Crystal arthropathy Arthropathy Osteoarthritis: gout Gout Gout is a heterogeneous metabolic disease associated with elevated serum uric acid levels (> 6.8 mg/dL) and abnormal deposits of monosodium urate in tissues. The condition is often familial and is initially characterized by painful, recurring, and usually monoarticular acute arthritis, or “gout flare,” followed later by chronic deforming arthritis. Gout and CPPD |
Gout
Gout
Gout is a heterogeneous metabolic disease associated with elevated serum uric acid levels (> 6.8 mg/dL) and abnormal deposits of monosodium urate in tissues. The condition is often familial and is initially characterized by painful, recurring, and usually monoarticular acute arthritis, or “gout flare,” followed later by chronic deforming arthritis.
Gout management:
|
| Septic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis |
|
| PFPS |
|
| Popliteal (Baker) cyst |
|