Asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation causing symptoms and structural changes. The classification and phenotypes are heterogeneous but mainly divided into T2-high (inflammatory with eosinophils Eosinophils Granular leukocytes with a nucleus that usually has two lobes connected by a slender thread of chromatin, and cytoplasm containing coarse, round granules that are uniform in size and stainable by eosin. Innate Immunity: Phagocytes and Antigen Presentation) and T2-low (noninflammatory) asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with wheezing Wheezing Wheezing is an abnormal breath sound characterized by a whistling noise that can be relatively high-pitched and shrill (more common) or coarse. Wheezing is produced by the movement of air through narrowed or compressed small (intrathoracic) airways. Wheezing, cough, and dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea. Diagnosis is confirmed with pulmonary function testing Pulmonary Function Testing Pulmonary Function Tests showing a reversible obstructive pattern. Treatment, based on symptom severity, includes bronchodilators Bronchodilators Asthma Drugs and inhaled corticosteroids Corticosteroids Chorioretinitis for control of inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation. Biologic agents Biologic Agents Immunosuppressants targeting inflammatory mediators have been developed for severe persistent asthma Persistent Asthma Asthma in Children.
Last updated: Aug 8, 2024
Asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma is a chronic inflammatory disorder of the airways:
In established asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma, different triggers (precipitants) may exacerbate the symptoms. These include the following:
Asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma can be classified based on its severity, level of control, and clinical phenotypes.
Severity:
Status of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma control:[8,9]
Clinical phenotypes:[1–4,7,12]
The traditional division into only 2 types (allergic and nonallergic) has shown to be an oversimplification, as multiple pathophysiologic mechanisms can lead to asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma. Type 2 (T2) includes allergic asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma but is not always synonymous with either “allergic” or “nonallergic” eosinophilic asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma.
The pathophysiology of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma is heterogeneous, but division into T2-high and T2-low phenotypes is important for diagnosis and treatment. No single histopathologic feature is seen; common inflammatory cell airway Airway ABCDE Assessment infiltration is seen with eosinophils Eosinophils Granular leukocytes with a nucleus that usually has two lobes connected by a slender thread of chromatin, and cytoplasm containing coarse, round granules that are uniform in size and stainable by eosin. Innate Immunity: Phagocytes and Antigen Presentation, neutrophils Neutrophils Granular leukocytes having a nucleus with three to five lobes connected by slender threads of chromatin, and cytoplasm containing fine inconspicuous granules and stainable by neutral dyes. Innate Immunity: Phagocytes and Antigen Presentation, and lymphocytes Lymphocytes Lymphocytes are heterogeneous WBCs involved in immune response. Lymphocytes develop from the bone marrow, starting from hematopoietic stem cells (HSCs) and progressing to common lymphoid progenitors (CLPs). B and T lymphocytes and natural killer (NK) cells arise from the lineage. Lymphocytes: Histology (particularly T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions).[1–4]
Characterized by inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation with airway Airway ABCDE Assessment edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema, mast cell Mast cell Granulated cells that are found in almost all tissues, most abundantly in the skin and the gastrointestinal tract. Like the basophils, mast cells contain large amounts of histamine and heparin. Unlike basophils, mast cells normally remain in the tissues and do not circulate in the blood. Mast cells, derived from the bone marrow stem cells, are regulated by the stem cell factor. Angioedema activation, and cytokine release, then remodeling:
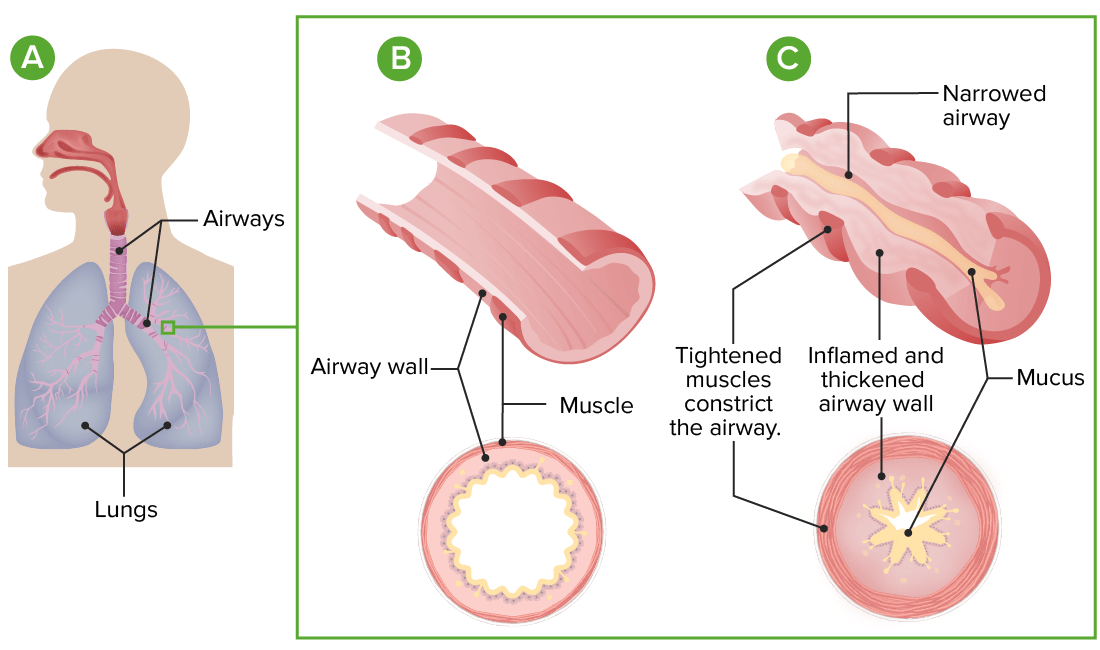
Pathophysiology of asthma:
A: Lung and airway anatomy
B: Cross-section of a normal airway
C: In asthma, exaggerated airway constriction, inflammation, and increased mucus production lead to restriction of airflow.
An acute asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma attack presents with cough, wheezing Wheezing Wheezing is an abnormal breath sound characterized by a whistling noise that can be relatively high-pitched and shrill (more common) or coarse. Wheezing is produced by the movement of air through narrowed or compressed small (intrathoracic) airways. Wheezing, anxiety Anxiety Feelings or emotions of dread, apprehension, and impending disaster but not disabling as with anxiety disorders. Generalized Anxiety Disorder, and dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea. Symptoms may appear after exposure to an allergen, as with extrinsic asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma, or for no identifiable reason, as with intrinsic asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma.
The diagnosis of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma should be suspected in individuals with intermittent wheezing Wheezing Wheezing is an abnormal breath sound characterized by a whistling noise that can be relatively high-pitched and shrill (more common) or coarse. Wheezing is produced by the movement of air through narrowed or compressed small (intrathoracic) airways. Wheezing. History-based diagnosis of “probable asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma” is appropriate in clinical settings where peak flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure measurement and spirometry Spirometry Measurement of volume of air inhaled or exhaled by the lung. Pulmonary Function Tests are not available and the patient has typical symptoms that respond promptly to therapy. Tests that confirm asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma are those demonstrating variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables expiratory airflow limitation (e.g., spirometry Spirometry Measurement of volume of air inhaled or exhaled by the lung. Pulmonary Function Tests) and exclusion of other diagnoses.
It is essential to ask questions to help identify asthma triggers Asthma Triggers Asthma in Children and episodic, recurring symptoms.
Assessing lung function is an important part of the diagnosis of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma. Usually, these tests are performed before initiating therapy with an inhaled corticosteroid. However, to confirm the diagnosis of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma in a patient already receiving inhaled corticosteroid therapy, refer to the Global Initiative for Asthma (GINA) guidelines.
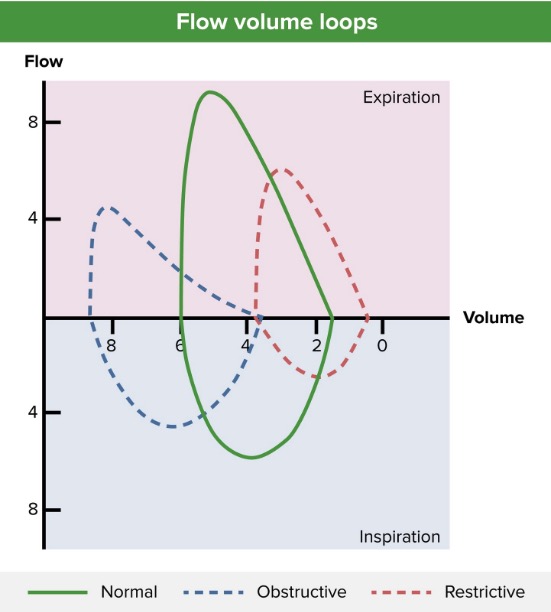
Flow-volume loop (blue line) showing an obstructive pattern of expiration, reduced peak expiratory flow (approximately 4 L/sec), and lung hyperinflation (approximately 4 L at residual volume and > 8 L after full inspiration). A normal pattern (green line) and restrictive pattern (red line) are shown for comparison.
Image by Lecturio.Asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma classifications systems address the severity of the disease and are used to guide therapy. There is some overlap between classifications.
| Intermittent/ step 1 | Mild persistent/ step 2 | Moderate persistent/ step 3 | Severe persistent/ steps 4–6 | |
|---|---|---|---|---|
| Symptoms | ≤ 2 days/week | > 2 but < 7 days/week | Daily | Throughout the day |
| Short-acting bronchodilator use | ≤ 2 days/week | > 2 days/week | Daily | Several times/day |
| Nighttime awakenings | ≤ 2/month | 3–4/month | ≥ 1/week | Nightly |
| Activity limitation | None | Minor | Some | Extreme |
| Lung function | FEV1 > 80% | FEV1 > 80% | FEV1 60%–80% | FEV1 < 60% |
| Exacerbations requiring systemic corticosteroids Corticosteroids Chorioretinitis | 0–1/year | ≥ 2/year | ||
Management may vary depending on practice location. The following information is mostly based on international and US literature and guidelines for adult patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Please refer to the National Institute of Health and Care Excellence (NICE) guidelines and the Scottish Intercollegiate Guidelines Network (SIGN) guidelines if you are practicing in the UK.
The following are recommended for all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma:
Treatment options are guided by asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma severity and should be personalized to the patient.
Types of medications:[1,2,8,9]
What to prescribe:[8,9,13]
Prescribing considerations:[9,14]
| Drug class | Medication options* | |
|---|---|---|
| SABAs |
|
|
| ICS |
|
|
| Combination therapy | SABA/ICS | Albuterol Albuterol A short-acting beta-2 adrenergic agonist that is primarily used as a bronchodilator agent to treat asthma. Sympathomimetic Drugs and budesonide Budesonide A glucocorticoid used in the management of asthma, the treatment of various skin disorders, and allergic rhinitis. Asthma Drugs |
| ICS/LABA |
|
|
| Triple therapy (ICS/ LABA/LAMA) | Fluticasone Fluticasone A steroid with glucocorticoid receptor activity that is used to manage the symptoms of asthma; allergic rhinitis, and atopic dermatitis. Glucocorticoids furoate, umeclidinium, and vilanterol Vilanterol Asthma Drugs | |
| LTRAs |
|
|
| Medication | Type | Low dose | Medium dose | High dose |
|---|---|---|---|---|
| Beclomethasone Beclomethasone An anti-inflammatory, synthetic glucocorticoid. It is used topically as an anti-inflammatory agent and in aerosol form for the treatment of asthma. Asthma Drugs dipropionate |
|
200–500 µg | 500–1,000 µg | > 1,000 µg |
| Budesonide Budesonide A glucocorticoid used in the management of asthma, the treatment of various skin disorders, and allergic rhinitis. Asthma Drugs |
|
200–400 µg | 400–800 µg | > 800 µg |
| Fluticasone Fluticasone A steroid with glucocorticoid receptor activity that is used to manage the symptoms of asthma; allergic rhinitis, and atopic dermatitis. Glucocorticoids furoate |
|
100 µg | 100 µg | 200 µg |
| Fluticasone Fluticasone A steroid with glucocorticoid receptor activity that is used to manage the symptoms of asthma; allergic rhinitis, and atopic dermatitis. Glucocorticoids propionate |
|
100–250 µg | 250–500 µg | > 500 µg |
| Mometasone Mometasone Asthma Drugs furoate |
|
200–400 µg | 200–400 µg | > 400 µg |
The following information is based on preferred, stepwise therapy:[8]
People with severe asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma may have what is called type 2 inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation (characterized by production of IL-4, IL-5, and IL-13 by the adaptive immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs in response to an allergen).
Regular Regular Insulin assessment of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma (at least annually) for symptom control and risk of exacerbations is essential.
Assess symptom control:
Review risk for adverse outcomes:
Plan:
Management options will be based on severity. Frequent reassessment should be performed to determine response to therapy, augmentation of therapy, and need for hospitalization Hospitalization The confinement of a patient in a hospital. Delirium.
Medications:
Respiratory management:
Reassess frequently:
| Severity | Clinical features | Initial treatment options |
|---|---|---|
| Mild to moderate |
|
|
| Severe |
|
|
|
Above plus:
|
Administration of inhaled medications through a nebulizer may be needed for emergent symptom relief.
Image: “Administering inhaled medication” by British Columbia Institute of Technology (BCIT). License: CC BY 4.0