Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with enlarged uterine size for gestational age, dyspnea, extremity swelling, or uterine contractions. Diagnosis is made based on ultrasound findings showing excessive amniotic fluid index ≥24 cm or single deepest pocket ≥8 cm. It is associated with significant neonatal and maternal morbidity and mortality. Mild cases can resolve spontaneously. Management of moderate-to-severe cases can include fetal monitoring, amnioreduction, administration of medications such as NSAIDs (e.g., indomethacin), and labor induction.
Last updated: Mar 4, 2024
Polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios is an abnormally high level of amniotic fluid Amniotic fluid A clear, yellowish liquid that envelopes the fetus inside the sac of amnion. In the first trimester, it is likely a transudate of maternal or fetal plasma. In the second trimester, amniotic fluid derives primarily from fetal lung and kidney. Cells or substances in this fluid can be removed for prenatal diagnostic tests (amniocentesis). Placenta, Umbilical Cord, and Amniotic Cavity in the amniotic sac.
Two major causes of polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios:
Diagnostic criteria can vary based on location. The following information is based on US medical society recommendations.
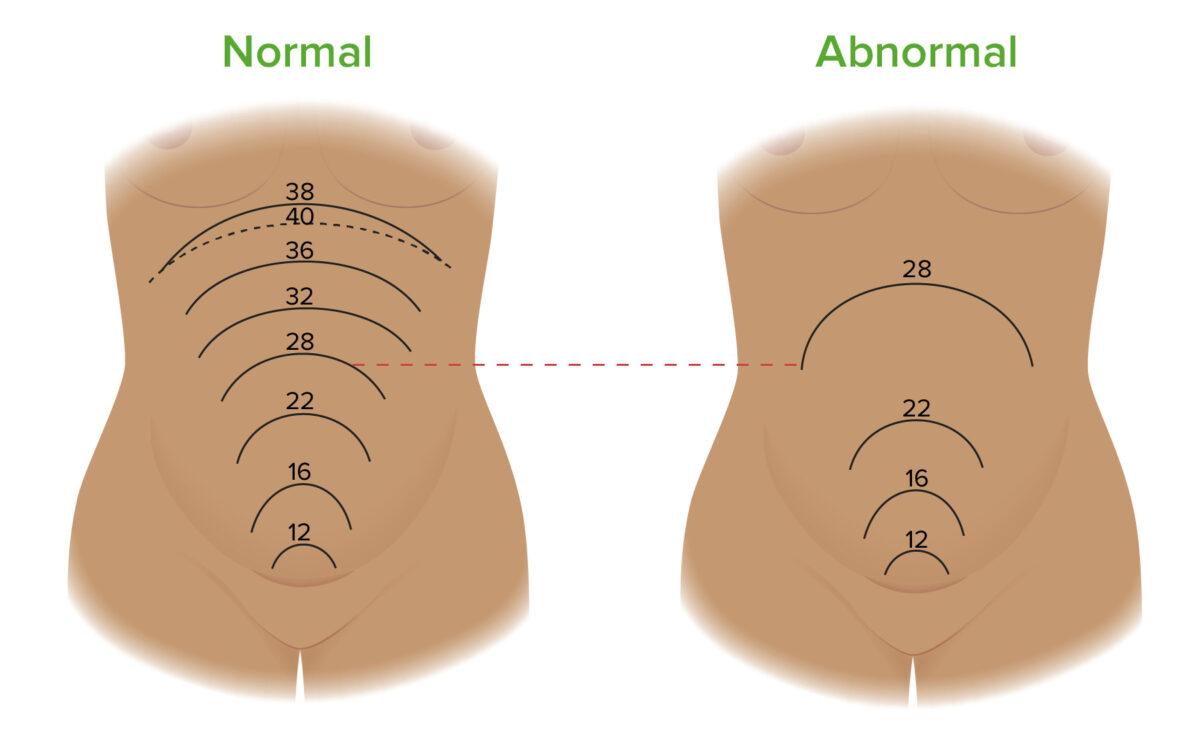
Fundal heights throughout pregnancy in normal cases (left) and pregnancies complicated by polyhydramnios (right). The fundal height (FH) is the length between the pubic symphysis and the top of the fundus. The FH measured in centimeters should be approximately equal to the fetus’ gestational age in weeks. For example, at 28 weeks, the FH should be ~ 28 cm. A discrepancy of > 3 cm is suspicious for polyhydramnios. The image on the left shows where the fundus is located at different gestational ages throughout a normal pregnancy. The image on the right shows a potential progression of fundal growth in a pregnancy complicated by polyhydramnios. Notice how the FH at 28 weeks is significantly higher in the pregnancy complicated by polyhydramnios compared to a normal pregnancy.
Image by Lecturio.| Classification of polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios | Amniotic fluid Amniotic fluid A clear, yellowish liquid that envelopes the fetus inside the sac of amnion. In the first trimester, it is likely a transudate of maternal or fetal plasma. In the second trimester, amniotic fluid derives primarily from fetal lung and kidney. Cells or substances in this fluid can be removed for prenatal diagnostic tests (amniocentesis). Placenta, Umbilical Cord, and Amniotic Cavity index (AFI) | Single deep pocket (SDP) |
|---|---|---|
| Mild | 24–29.9 cm | 8–11.9 cm |
| Moderate | 30–34.9 cm | 12–15.9 cm |
| Severe | ≥ 35 cm | ≥ 16 cm |
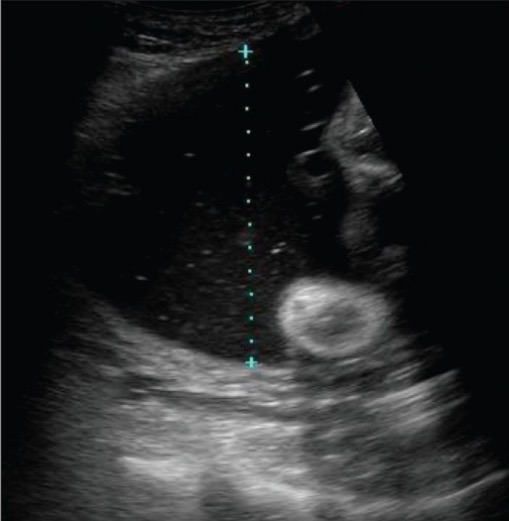
The photo demonstrates the measurement of a vertical pocket of amniotic fluid, which is used in the assessment of amniotic fluid volume. If this was the deepest fluid pocket present, it would be known as the single deepest pocket (SDP); values ≥ 8 cm are classified as polyhydramnios.
Image: “Demonstration of the technique to measure a single vertical pocket of liquor” by Kinare A. License: CC BY 2.0Although idiopathic Idiopathic Dermatomyositis is the most common type of polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios, it is a diagnosis of exclusion. Workup to identify potential causative etiologies can include the following (those indicated with an asterisk (*) are typically already part of routine antenatal care):
Note: Symptomatic polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios (e.g., dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, preterm labor Preterm labor Preterm labor refers to regular uterine contractions leading to cervical change prior to 37 weeks of gestation; preterm birth refers to birth prior to 37 weeks of gestation. Preterm birth may be spontaneous due to preterm labor, preterm prelabor rupture of membranes (PPROM), or cervical insufficiency. Preterm Labor and Birth) often has an underlying etiology.[9]
Management may vary depending on location. The following information is based on US medical society recommendations.