Fetal presentation describes which part of the fetus will enter through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first, while position is the orientation Orientation Awareness of oneself in relation to time, place and person. Psychiatric Assessment of the fetus compared to the maternal bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 "hip" bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy. Presentations include vertex (the fetal occiput will present through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first), face, brow, shoulder, and breech. If a fetal limb is presenting next to the presenting part (e.g., the hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy is next to the head), this is known as a compound presentation. Malpresentation refers to any presentation other than vertex, with the most common being breech presentations. Vaginal delivery of a breech infant increases the risk for head entrapment and hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage, so, especially in the United States, mothers are generally offered a procedure to help manually rotate the baby to a head-down position instead (known as an external cephalic version) or a planned cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery.
Last updated: Feb 14, 2023
Prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency rates for different malpresentations at term:
Fetal lie is how the long axis of the fetus is oriented in relation to the mother. Possible lies include:
Presentation describes which body part of the fetus will pass through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first. Presentations include:
Cephalic presentations can be categorized as:
Vertex presentation
Image by Lecturio. License: CC BY-NC-SA 4.0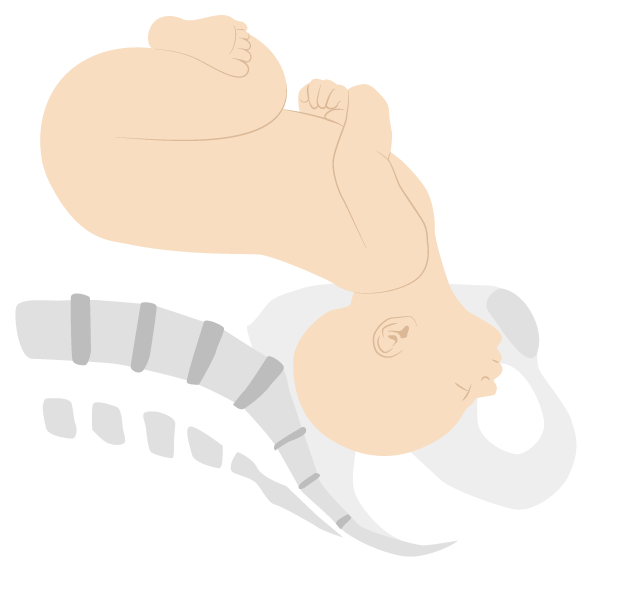
Face presentation (mentum anterior position)
Image by Lecturio. License: CC BY-NC-SA 4.0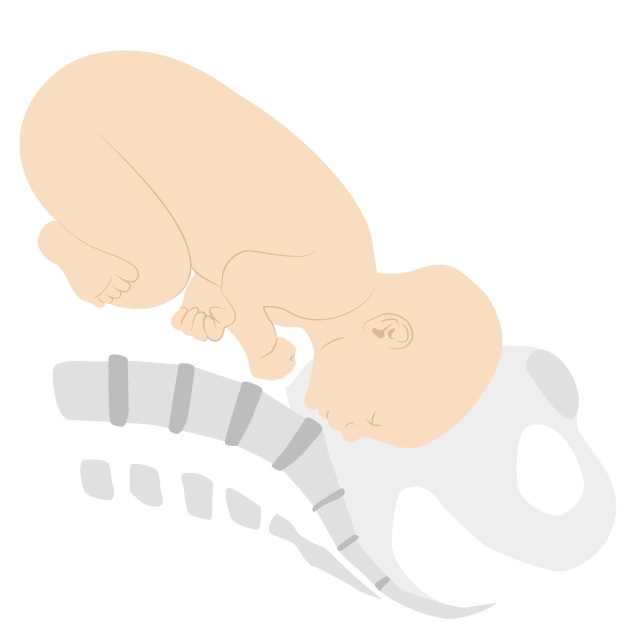
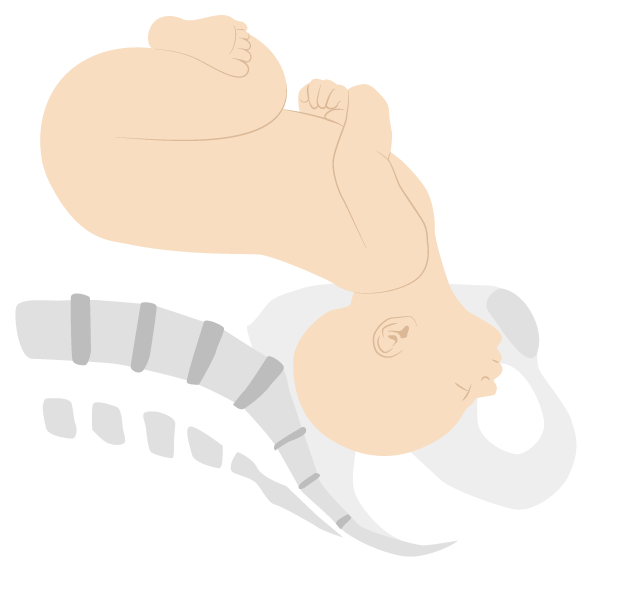
Brow presentation (mentum posterior position)
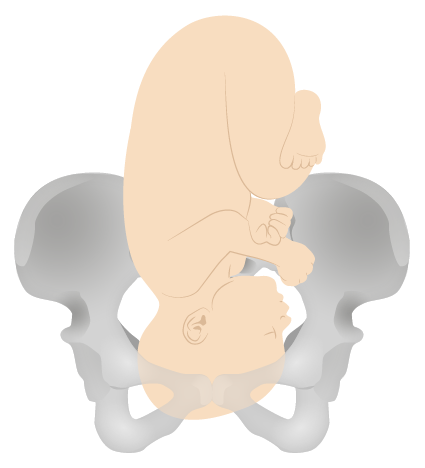
Image by Lecturio. License: CC BY-NC-SA 4.0Breech presentations can be categorized as:
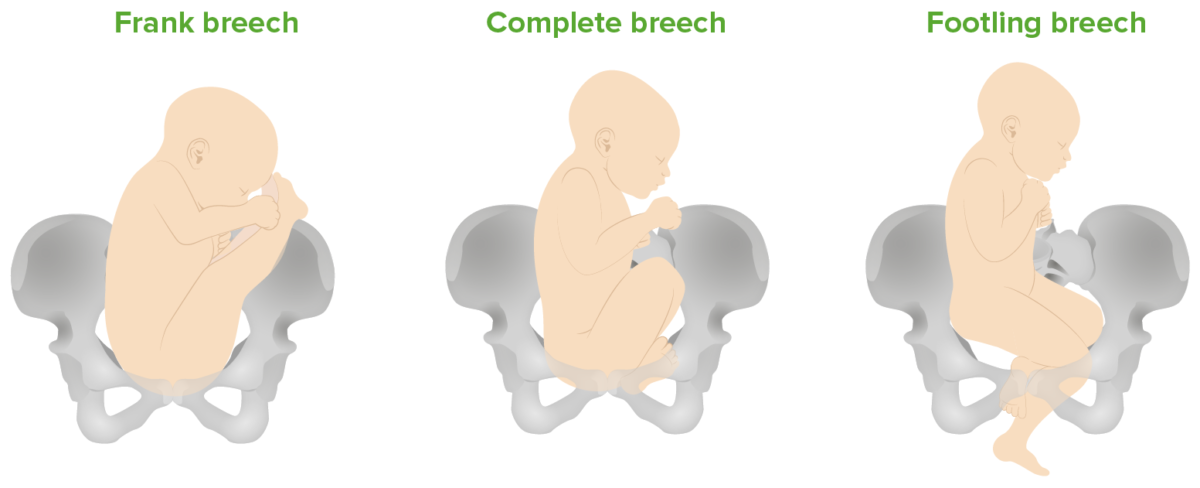
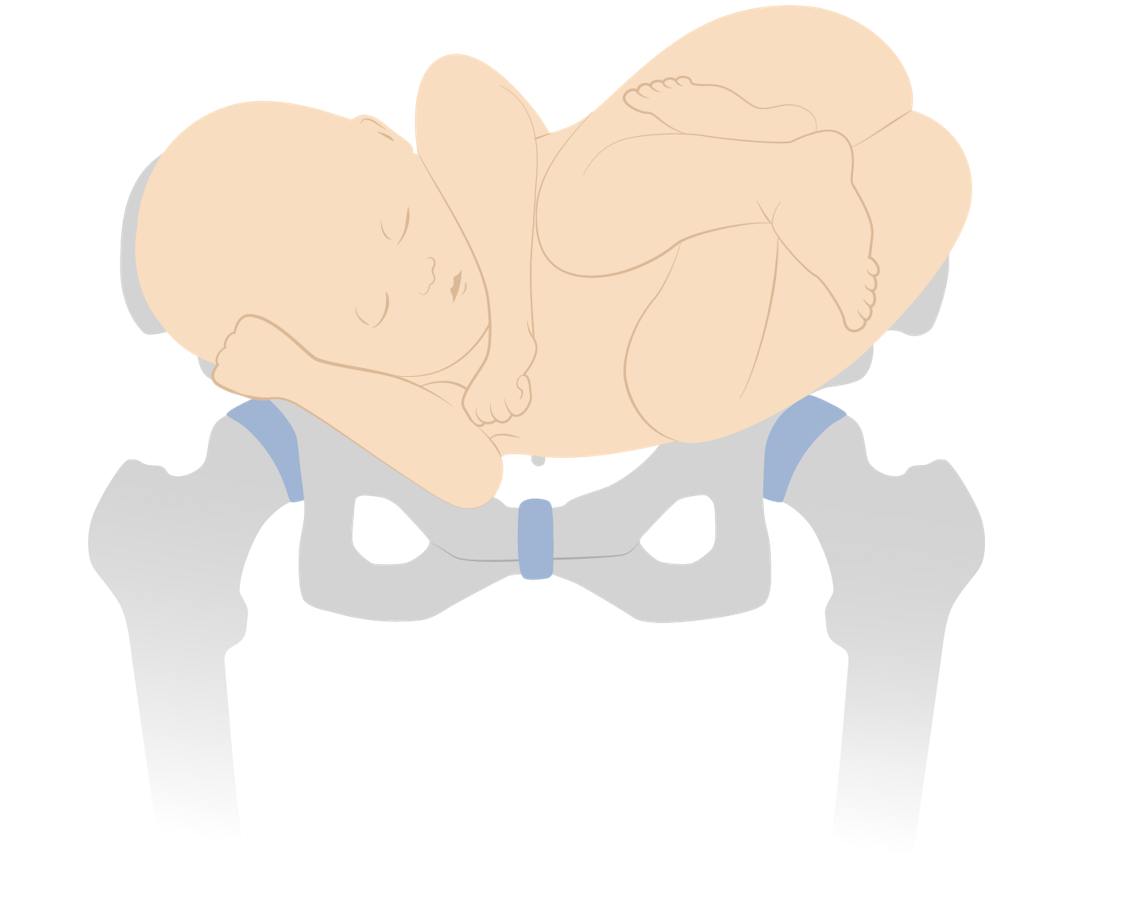
Breech presentations:
Frank (bottom down, legs extended), complete (bottom down, hips and knees both flexed), and footling (feet down) breech presentations
Shoulder presentation (transverse lie)
Image by Lecturio. License: CC BY-NC-SA 4.0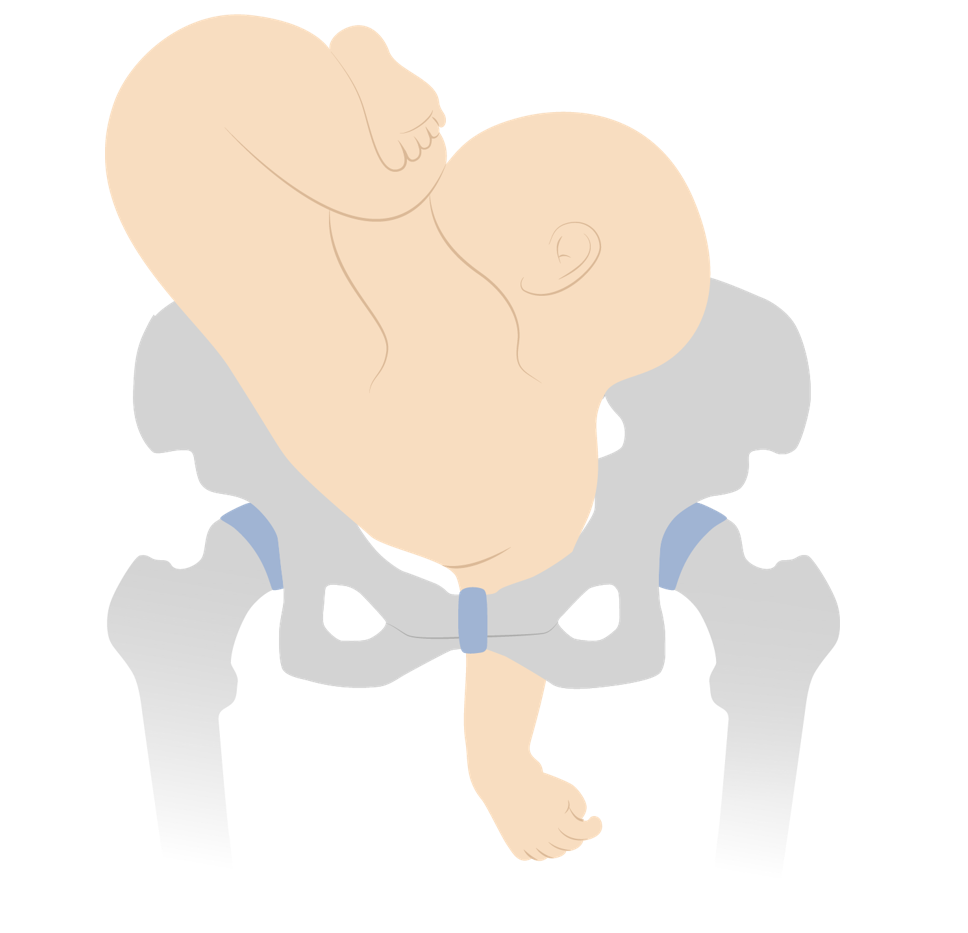
Neglected shoulder presentation resulting in arm prolapse during labor
Image by Lecturio. License: CC BY-NC-SA 4.0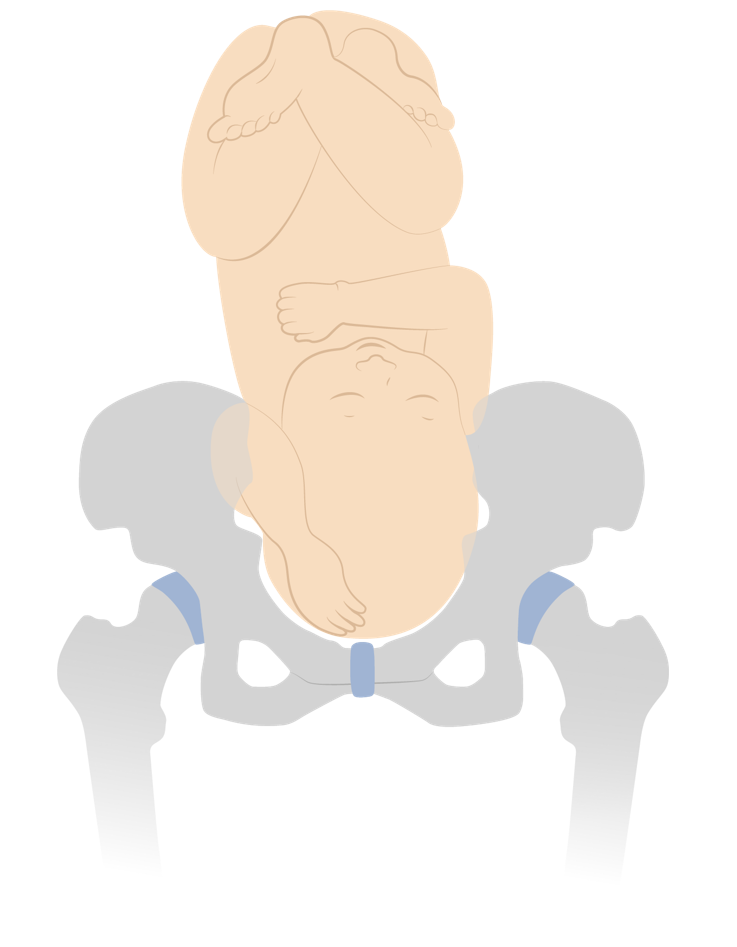
Vertex presentation with a compound hand
Image by Lecturio. License: CC BY-NC-SA 4.0Position describes the relation of the fetal presenting part to the maternal bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy.
Positions for vertex presentations describe the position of the fetal occiput.
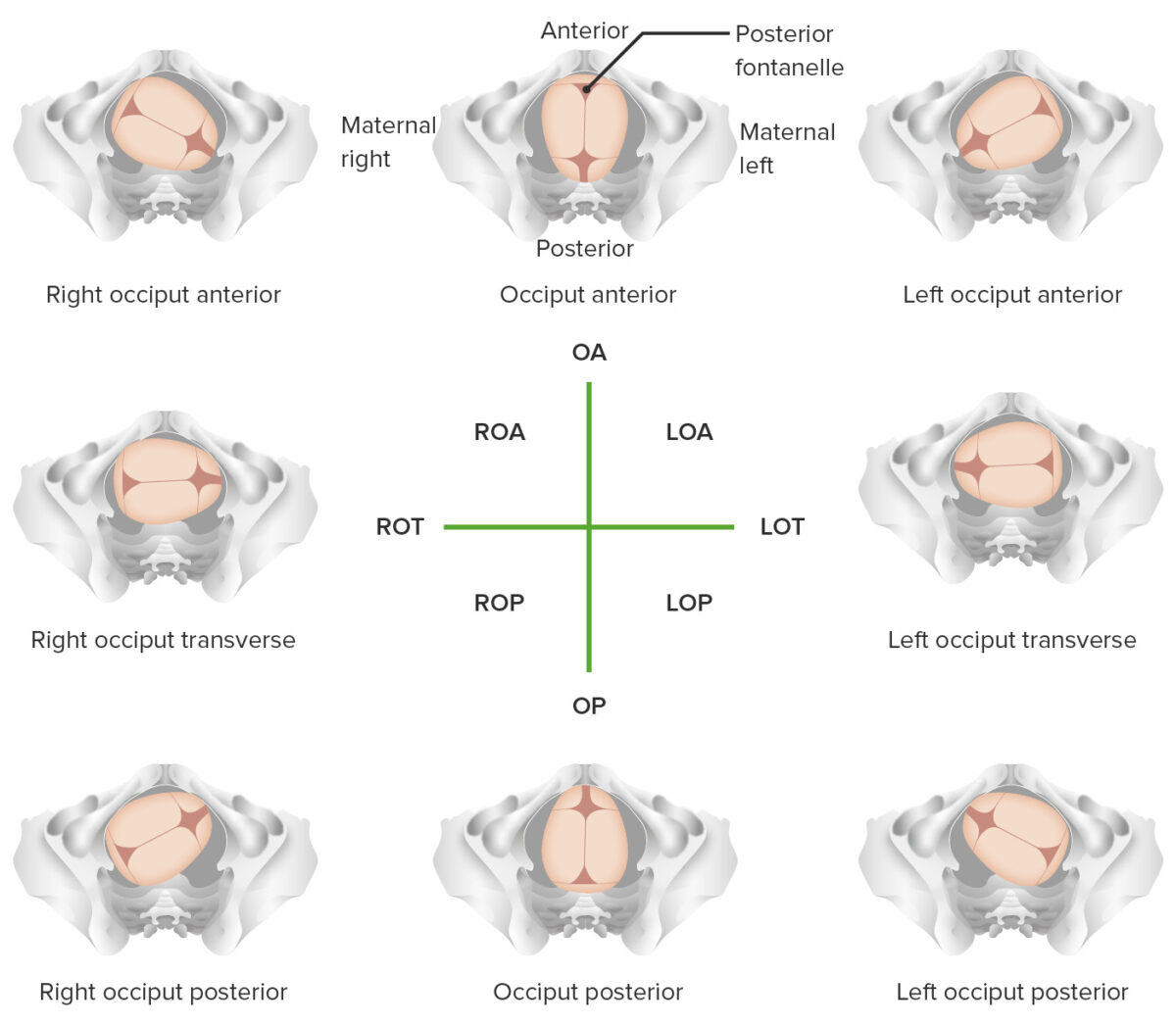
Overview of different vertex positions
LOA: left occiput anterior
LOP: left occiput posterior
LOT: left occiput transverse
OA occiput anterior
OP: occiput posterior
ROA: right occiput anterior
ROP: right occiput posterior
ROT:
right occiput transverse
Positions for face and brow presentations describe the position of the chin Chin The anatomical frontal portion of the mandible, also known as the mentum, that contains the line of fusion of the two separate halves of the mandible (symphysis menti). This line of fusion divides inferiorly to enclose a triangular area called the mental protuberance. On each side, inferior to the second premolar tooth, is the mental foramen for the passage of blood vessels and a nerve. Melasma.
Face presentation (mentum anterior position)
Image by Lecturio. License: CC BY-NC-SA 4.0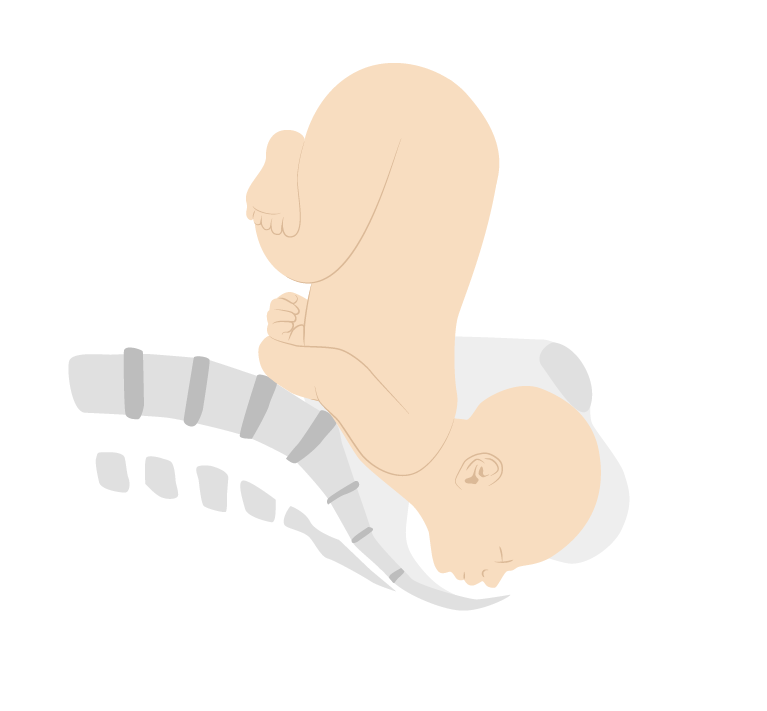
Face presentation (mentum posterior position)
Image by Lecturio. License: CC BY-NC-SA 4.0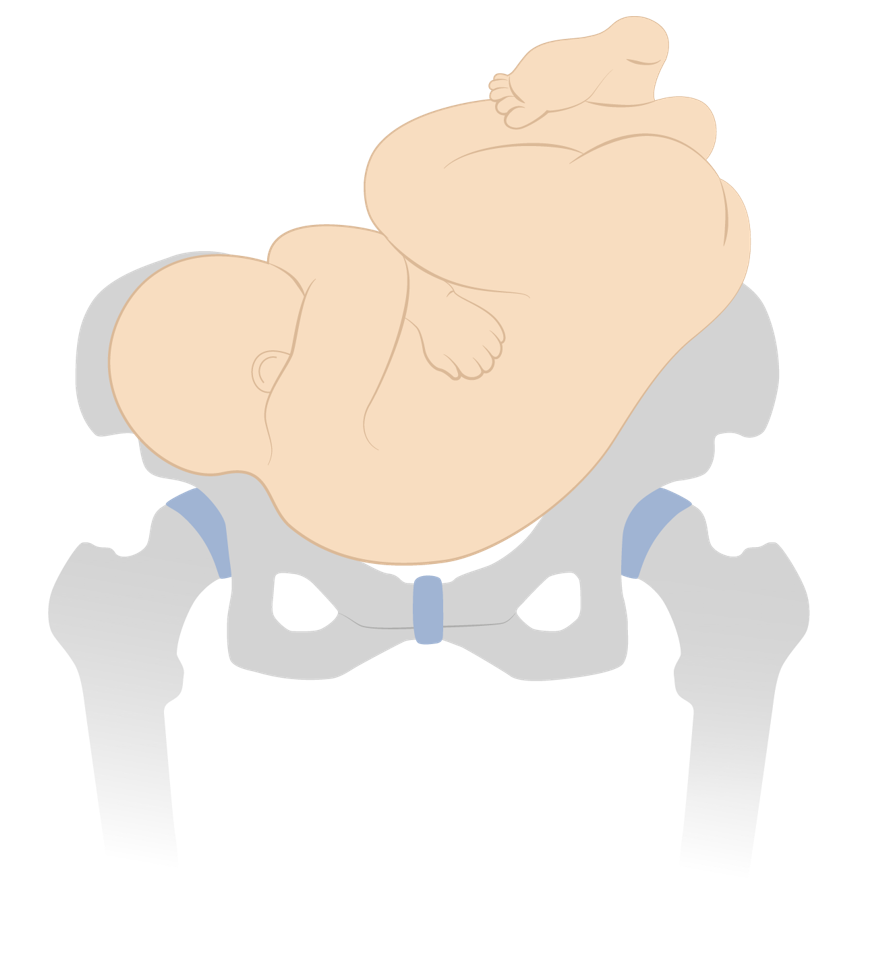
Dorso-inferior shoulder presentation
Image by Lecturio. License: CC BY-NC-SA 4.0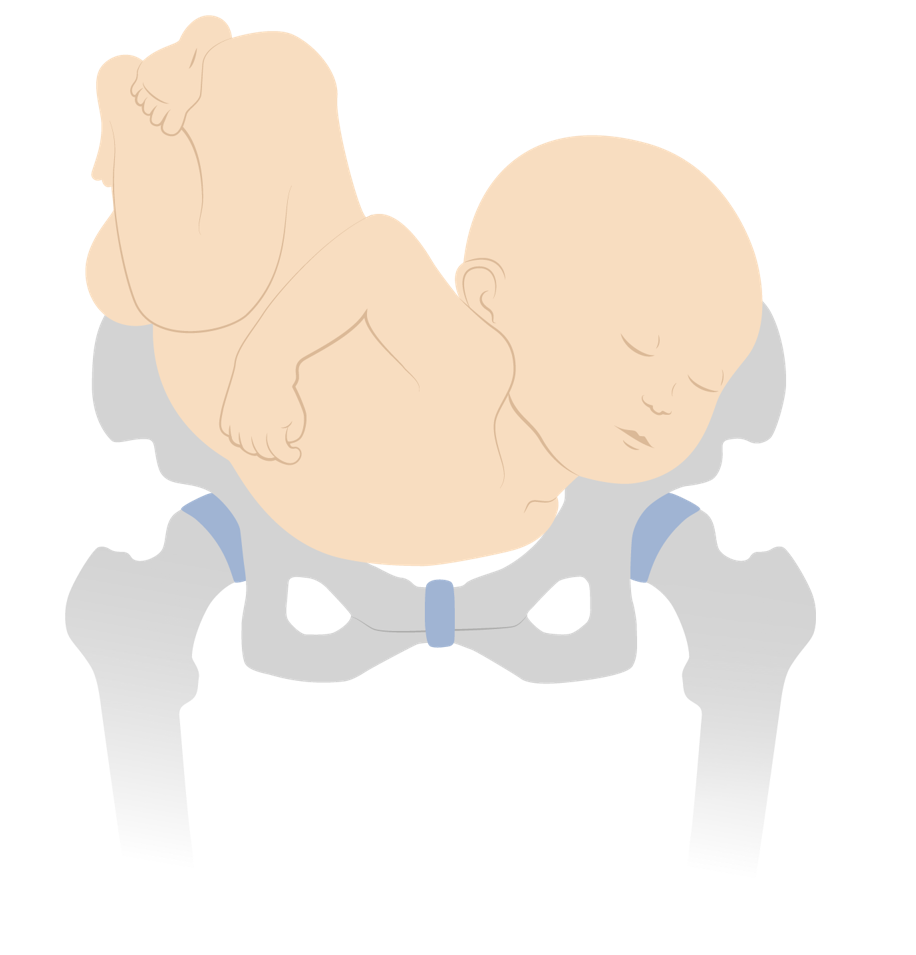
Dorso-superior shoulder presentation
Image by Lecturio. License: CC BY-NC-SA 4.0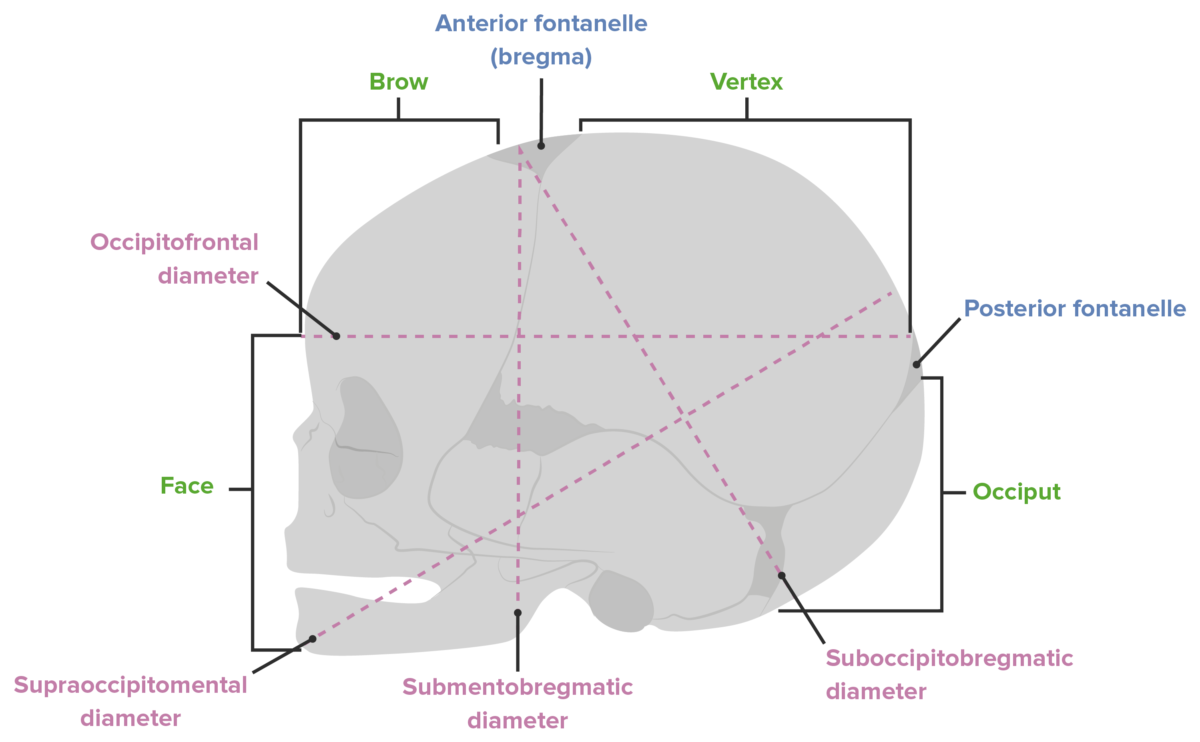
Diameters of the fetal head
Image by Lecturio. License: CC BY-NC-SA 4.0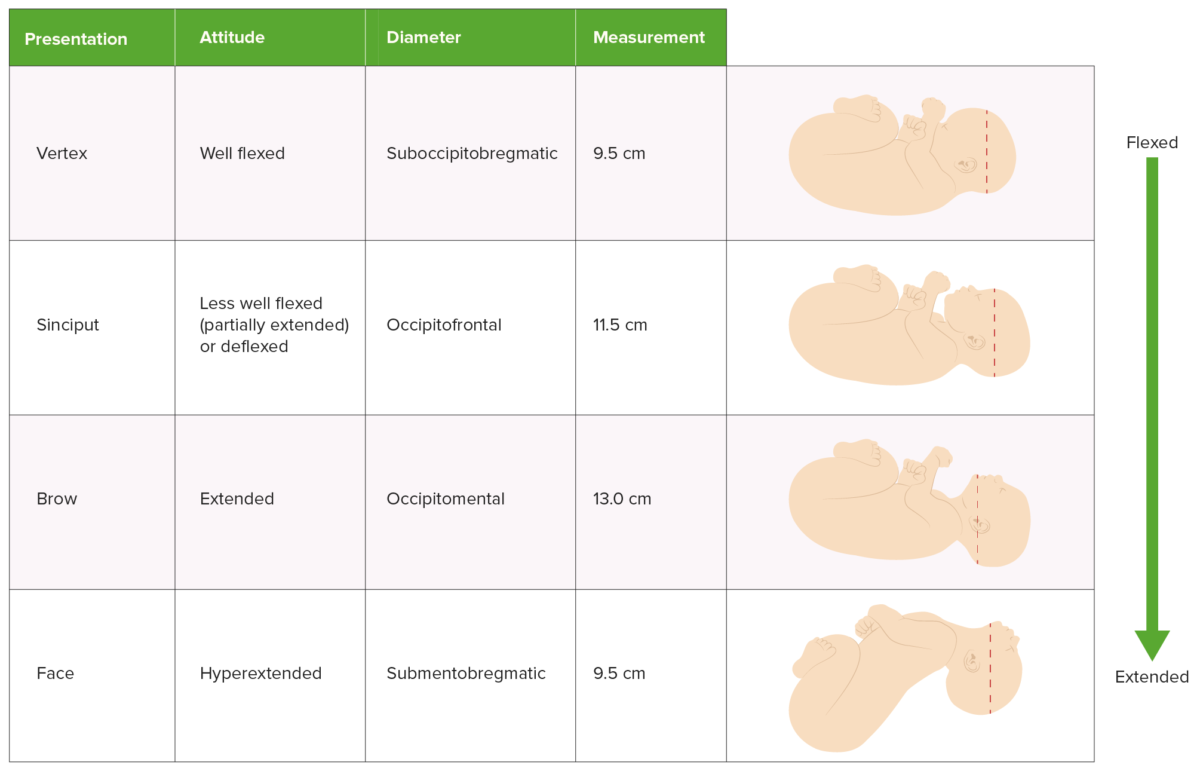
Comparison of presentation, attitude, and presenting diameter
Image by Lecturio. License: CC BY-NC-SA 4.0Delivery is managed differently depending on the presentation and position of the infant. This information can be established in several different ways:
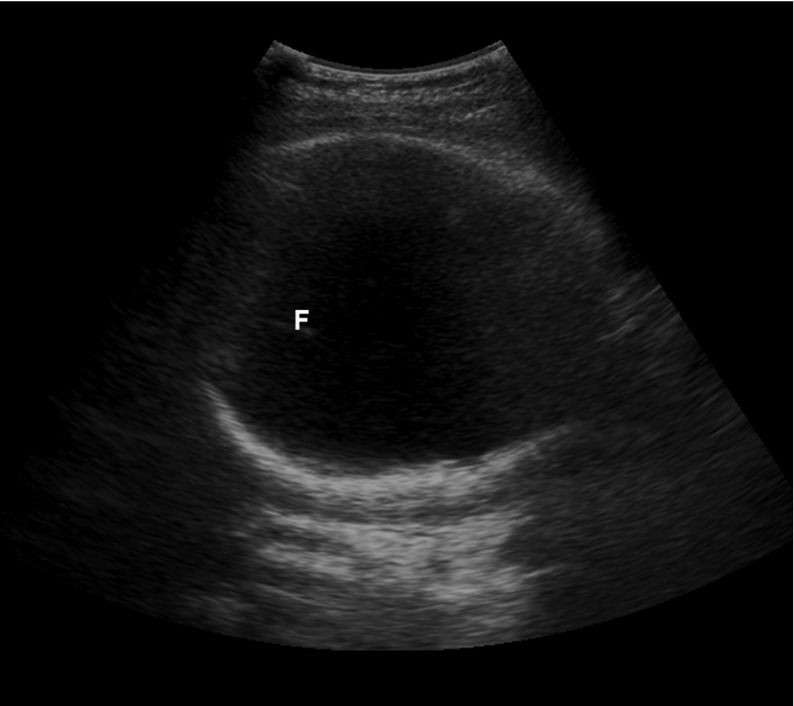
Suprapubic bedside ultrasound showing the large white circle of the fetal skull, confirming a cephalic presentation
F: fetal falx
There are 3 primary options for managing breech presentations: performing CD, attempting an external cephalic version to manually rotate the baby into a vertex presentation for attempted vaginal delivery, or a planned vaginal breech delivery (which is generally not done in the United States).
Most infants will spontaneously rotate to a vertex presentation as the pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care progresses. At different gestational ages, the prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of breech presentations is:
The following risks are associated with breech presentations in utero, regardless of mode of delivery:
The primary risk of a vaginal breech delivery is fetal head entrapment:
Vaginal breech deliveries for singleton gestations may be considered for certain low-risk women if vaginal delivery is strongly desired by the mother. In contrast, vaginal breech deliveries are done frequently for breech 2nd twins; the procedure is known as a breech extraction.
An external cephalic version (ECV) is a procedure in which the physician attempts to manually rotate the fetus from a breech to a cephalic presentation by pushing on the maternal abdomen.