Intestinal malrotation Malrotation Pediatric Gastrointestinal Abnormalities is a congenital anomaly that results from failure of the GI tract to undergo normal rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays around the mesenteric vessels during embryologic development. This condition can result in several anatomic patterns characterized by abnormal location and attachments of the abdominal cavity's intestines. These anomalies can be clinically silent or present with a number of complications, the most catastrophic of which is midgut Midgut Development of the Abdominal Organs volvulus Volvulus A volvulus is the twisting or axial rotation of a portion of the bowel around its mesentery. The most common site of volvulus in adults is the colon; most frequently the sigmoid volvulus. Patients typically present with symptoms of bowel obstruction such as abdominal pain, distension, vomiting, and constipation/obstipation. Volvulus. Intestinal malrotation Malrotation Pediatric Gastrointestinal Abnormalities usually presents in infancy as an acute onset of bilious vomiting Bilious Vomiting Congenital Duodenal Obstruction. Definitive diagnosis is established with the upper GI series Upper Gi Series Imaging of the Intestines and the treatment is emergent surgery.
Last updated: Mar 27, 2025
Intestinal malrotation Malrotation Pediatric Gastrointestinal Abnormalities is a failure of the GI tract to undergo normal rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays around mesenteric vessels during embryogenesis.
Malrotation Malrotation Pediatric Gastrointestinal Abnormalities represents a spectrum of rotational abnormalities. The 2 most common abnormalities are complete nonrotation and incomplete rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays.
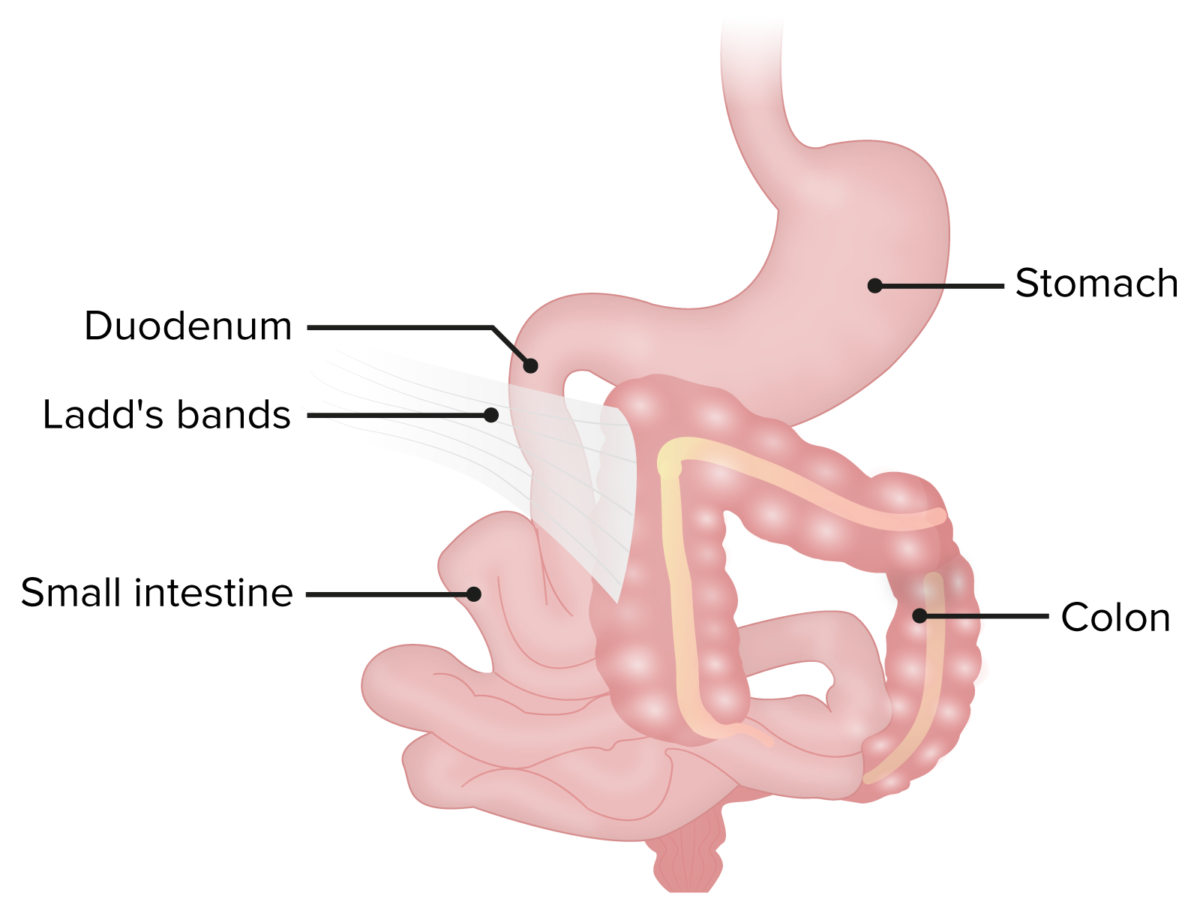
Ladd bands in a patient with malrotation.
The bands of fibrous peritoneal tissue can put pressure on and obstruct the duodenum.
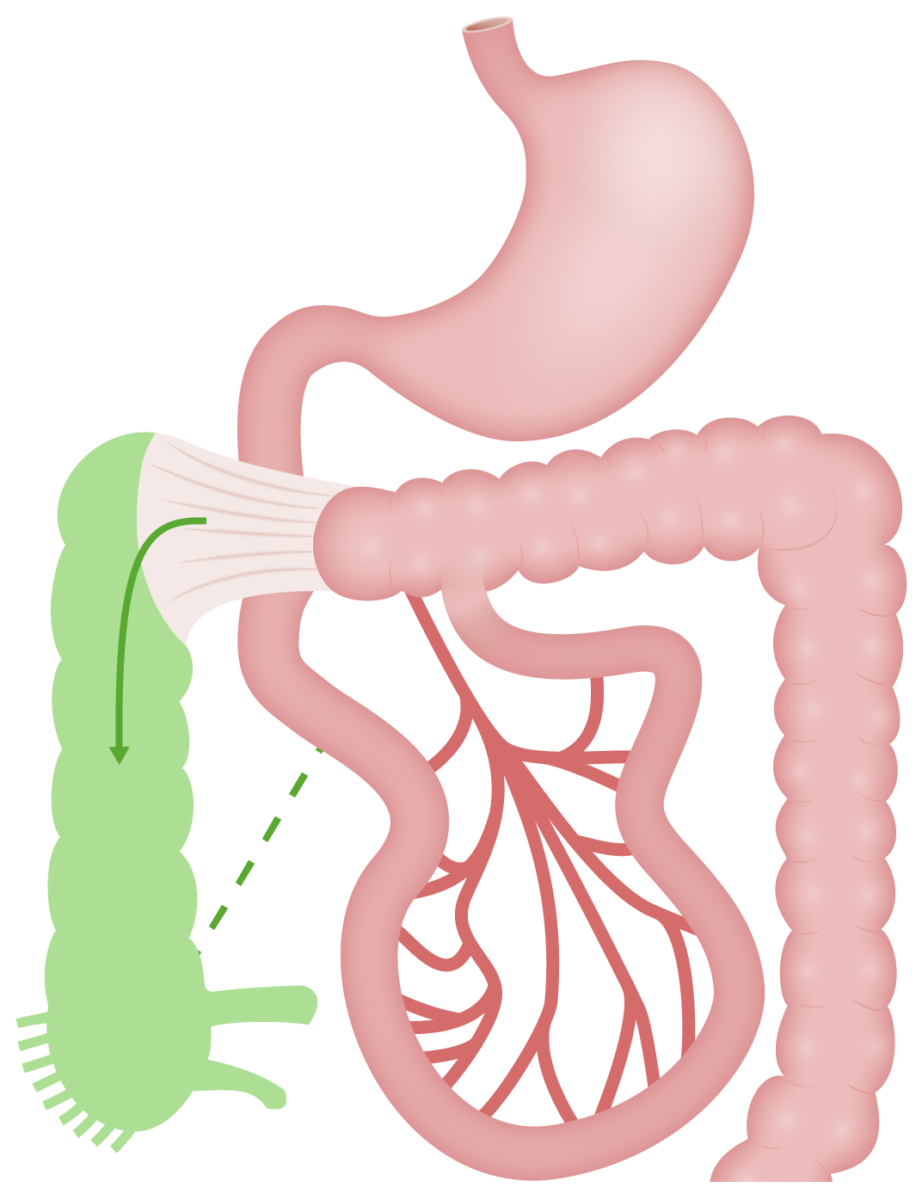
Malrotation:
Caecum remains high (RUQ) and fixed to posterior abdominal wall. Ladd bands are obstructing duodenum.
Normal anatomy is shown in green.
Should only be performed in stable patients Stable Patients Blunt Chest Trauma. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with hemodynamic instability/ sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock/ peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury should proceed to emergent surgery.
Abdominal X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests:
Upper GI series Upper Gi Series Imaging of the Intestines (UGI):
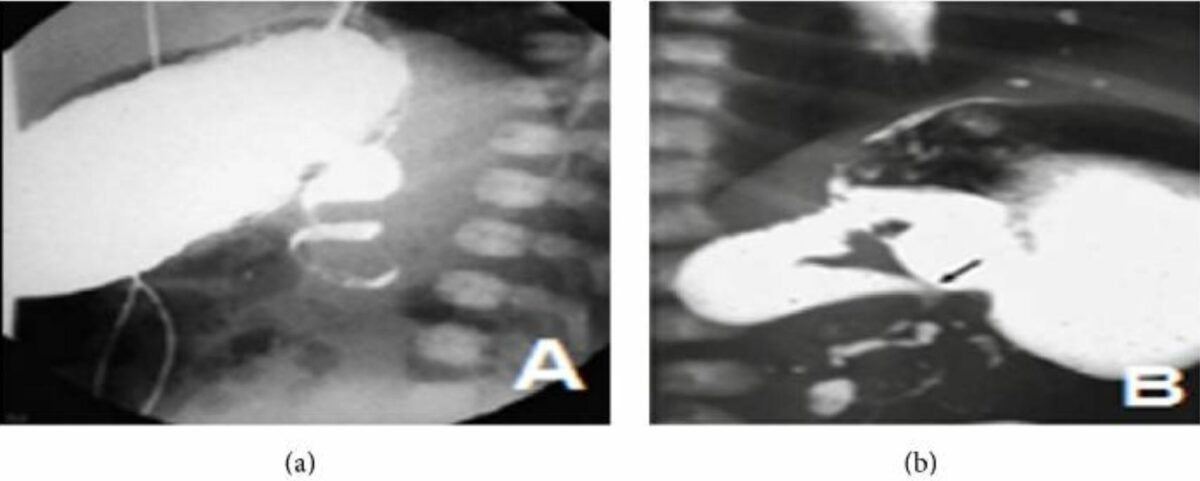
Upper GI series demonstrating malrotation:
(a) Upper GI series shows the “corkscrew sign” in a frontal view.
(b) Upper GI series shows malrotation with midgut volvulus. An incomplete duodenal obstruction and dilation of the first and second portions are seen, as is the “corkscrew sign.”

Ultrasound showing midgut volvulus:
Transverse section of abdominal ultrasound with Doppler showing a whirl sign image around the mesenteric vessels
Ultrasound:
Emergent laparotomy Laparotomy Incision into the side of the abdomen between the ribs and pelvis. Laparotomy and Laparoscopy:
Elective/prophylactic Ladd procedure:
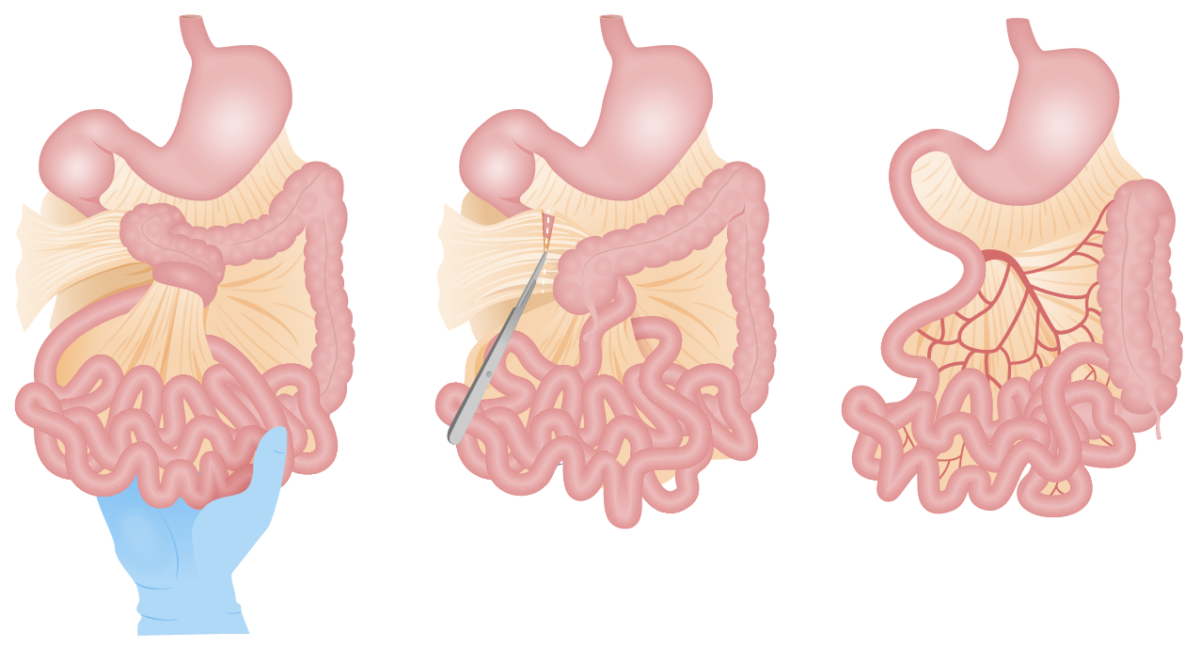
Ladd procedure:
Untwisting of the bowel and division of Ladd bands. Small bowel is placed on the right, and colon on the left side of the abdomen.