Hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy and wrist pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is very common among the general population. Up to 30% of adults will have hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways during their lives, and half of all cases progress to chronic pain Chronic pain Aching sensation that persists for more than a few months. It may or may not be associated with trauma or disease, and may persist after the initial injury has healed. Its localization, character, and timing are more vague than with acute pain. Pain Management. The causes of hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy and wrist pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be classified into mechanical (e.g., fractures, inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, ligament tear), neurologic (e.g., nerve entrapment), and systemic (e.g., autoimmune arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis). Reaching an accurate diagnosis involves following an evidence-based systematic approach. Treatment includes reducing stress on the ligaments, pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways management, and surgery.
Last updated: Nov 21, 2022
Up to 70% of cases of hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy or wrist pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be determined by history alone.
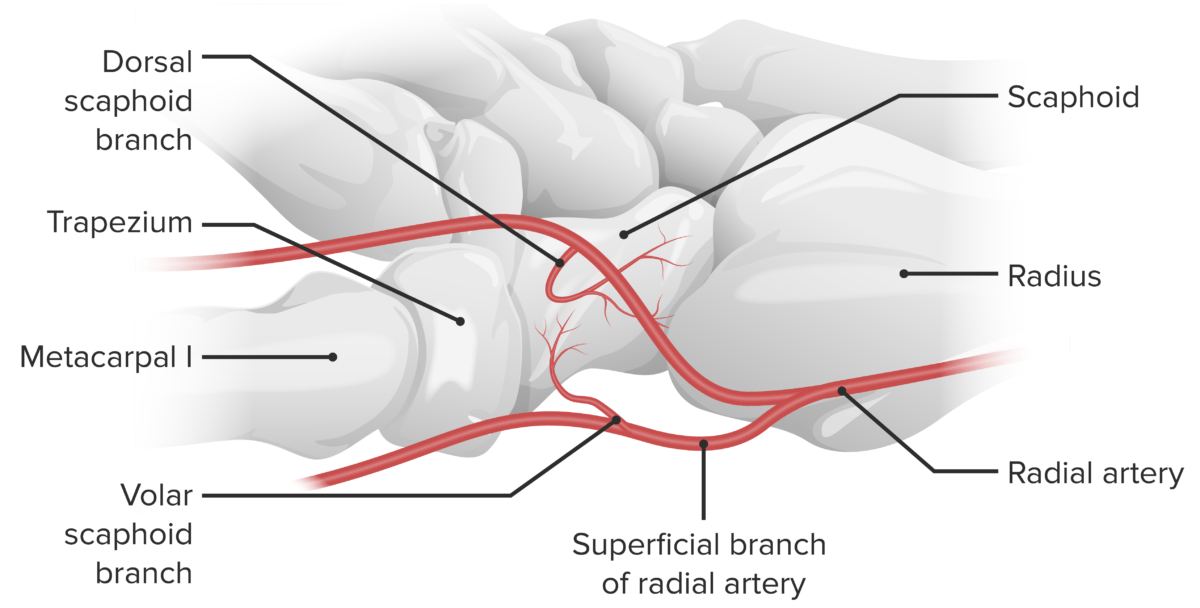
The scaphoid’s blood supply:
The scaphoid’s blood supply is primarily received from the lateral and distal branches of the radial artery via the palmar and dorsal branches. The palmar and dorsal branches provide an “abundant” supply of blood to the middle and distal portions of the bone, while the proximal portion receives the retrograde flow. The dorsal branch supplies the majority of the middle and distal portions, while the palmar branch supplies only the distal ⅓ of the bone.

Magnetic resonance imaging of a waist fracture of the scaphoid
Image: “Magnetic resonance imaging (patient D) of a waist fracture of the scaphoid” by Department of Trauma Surgery, Medical Centre Haaglanden, The Hague, The Netherlands. License: CC BY 2.0
Computed tomography of the wrist indicating hamate hook fracture
Image: “CT of right wrist indicating hamate hook fracture” by Parker College of Chiropractic Research Institute, 2500 Walnut Hill Lane, Dallas, TX 75229, USA. License: CC BY 2.0
a: Anteroposterior skiagram of the wrist with posterior perilunate dislocation showing an avulsion fracture of the tip of the ulnar styloid process
b: Lateral view of the wrist with posterior perilunate dislocation showing an avulsion fracture defect in the posterior horn of lunate: Note the arrowhead points to the fracture fragment.
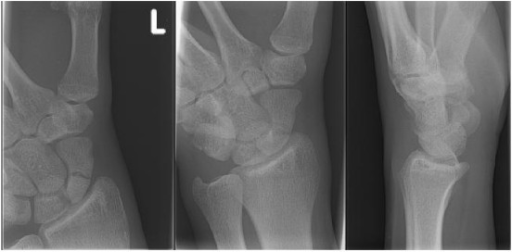
Radiograph of a scaphoid fracture: postero-anterior view, oblique view and lateral view
Image: “Initial radiograph” by Department of Trauma Surgery, Medical Centre Haaglanden, The Hague, The Netherlands. License: CC BY 2.0
Example of Finklestein’s test for De Quervain’s tenosynovitis
Image by LecturioInitially, diagnose and treat the underlying condition. General principles of hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy and wrist pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways management are carried out according to the RICE principle, as follows:
The following are possible etiologies of hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy and wrist pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways: