Trigeminal neuralgia (TN) is an often chronic and recurring pain syndrome involving the sensory distribution of the trigeminal nerve (cranial nerve (CN) V). The pain is typically unilateral and described as an acute, sharp, electric shock-like pain involving the maxillary or mandibular areas and often associated with spasm of facial muscles. Trigeminal neuralgia occurs in multiple, short-acting episodes. Most cases are usually due to vascular compression of the trigeminal nerve, although secondary causes can be due to aneurysms, neuromas, or other neurologic disorders. A detailed history is the hallmark for diagnosis. Neuroimaging with MRI is useful to determine the exact pathology involving the trigeminal nerve root. The 1st line of therapy is pharmacologic (carbamazepine). Other treatment options include botulinum toxin injections or surgical procedures in refractory cases.
Last updated: Mar 4, 2024
Trigeminal neuralgia Trigeminal neuralgia Trigeminal neuralgia (TN) is an often chronic and recurring pain syndrome involving the sensory distribution of the trigeminal nerve (cranial nerve (CN) V). The pain is typically unilateral and described as an acute, sharp, electric-shock-like pain involving the maxillary or mandibular areas and often associated with spasm of facial muscles. Trigeminal Neuralgia (TN) is a disorder presenting with recurrent, sharp pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in the distribution of the trigeminal nerve Trigeminal nerve The 5th and largest cranial nerve. The trigeminal nerve is a mixed motor and sensory nerve. The larger sensory part forms the ophthalmic, mandibular, and maxillary nerves which carry afferents sensitive to external or internal stimuli from the skin, muscles, and joints of the face and mouth and from the teeth. Most of these fibers originate from cells of the trigeminal ganglion and project to the trigeminal nucleus of the brain stem. The smaller motor part arises from the brain stem trigeminal motor nucleus and innervates the muscles of mastication. The 12 Cranial Nerves: Overview and Functions.
Trigeminal nerve Trigeminal nerve The 5th and largest cranial nerve. The trigeminal nerve is a mixed motor and sensory nerve. The larger sensory part forms the ophthalmic, mandibular, and maxillary nerves which carry afferents sensitive to external or internal stimuli from the skin, muscles, and joints of the face and mouth and from the teeth. Most of these fibers originate from cells of the trigeminal ganglion and project to the trigeminal nucleus of the brain stem. The smaller motor part arises from the brain stem trigeminal motor nucleus and innervates the muscles of mastication. The 12 Cranial Nerves: Overview and Functions (cranial nerve (CN) V):
3 major divisions of CN V:
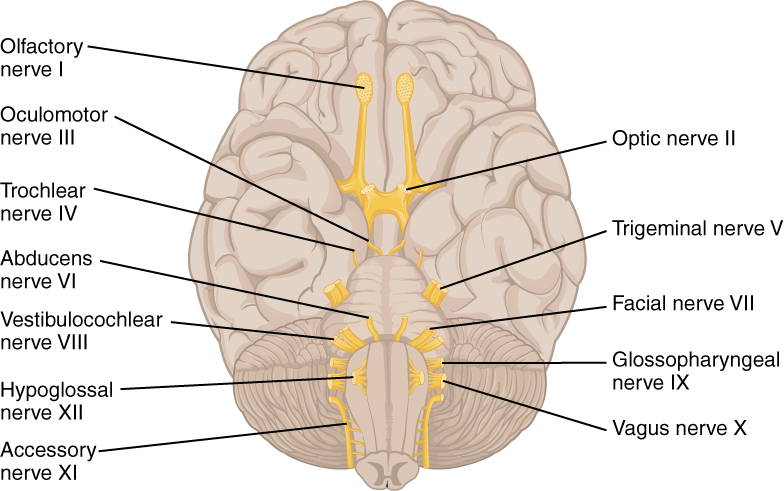
The 12 cranial nerves exiting the brain
Image: “The Cranial Nerves” by Phil Schatz. License: CC BY 4.0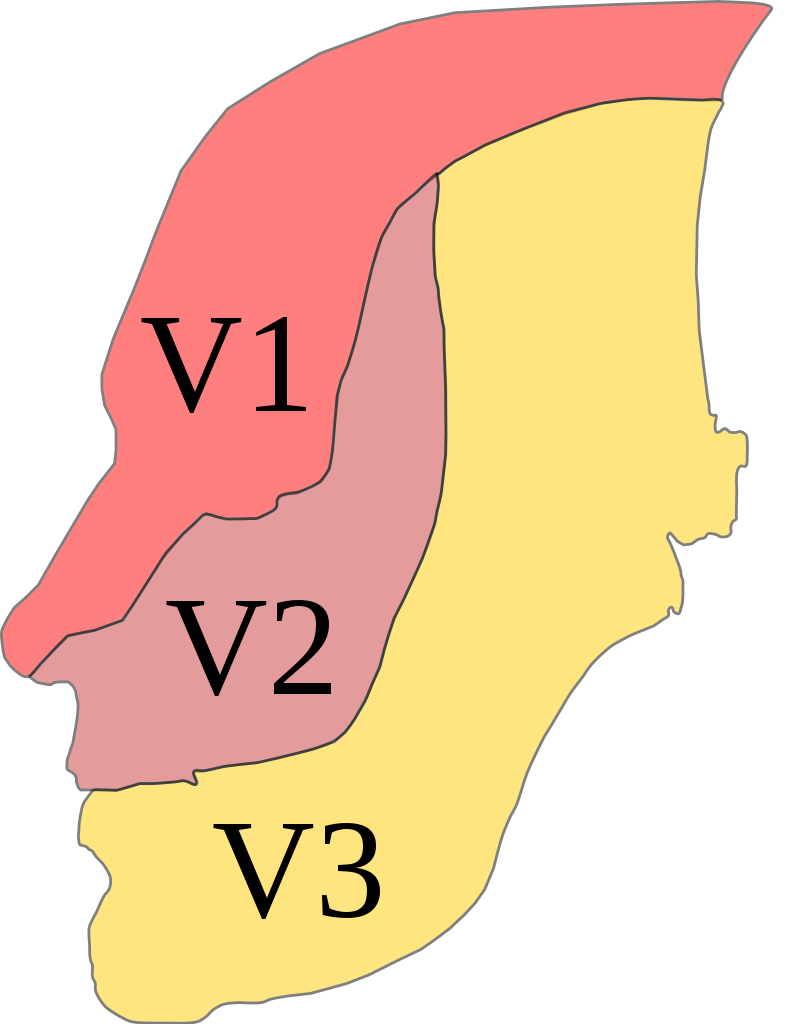
Trigeminal distribution
Image: “Trig innervation” by Madhero88. License: CC BY 3.0, edited by Lecturio.When other neurologic conditions (e.g., multiple sclerosis Sclerosis A pathological process consisting of hardening or fibrosis of an anatomical structure, often a vessel or a nerve. Wilms Tumor or aneurysms) are present, additional symptoms may include:
Diagnosis of TN is clinical, with a thorough history and physical. Further workup with imaging or laboratory studies may be required if red-flag symptoms are present.
Management may vary based on practice location. The following information is based on US and UK guidelines.