Shoulder pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is considered chronic when present for > 6 months. Common conditions resulting in chronic shoulder pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways include rotator cuff disorders, adhesive capsulitis, shoulder instability, and joint arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis. Shoulder pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be intrinsic or extrinsic to the joint. The potential of serious causes of referred pain Referred Pain Spinal Disk Herniation to the shoulder such as cardiovascular and abdominal etiologies should be considered. A focused history and physical examination is essential and should include inspection Inspection Dermatologic Examination, palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination, range of motion Range of motion The distance and direction to which a bone joint can be extended. Range of motion is a function of the condition of the joints, muscles, and connective tissues involved. Joint flexibility can be improved through appropriate muscle strength exercises. Examination of the Upper Limbs (ROM), and provocative testing. Imaging often includes plain radiographs occasionally supplemented with MRI. Management varies related to specific disorders and frequently requires physical therapy Physical Therapy Becker Muscular Dystrophy.
Last updated: Jun 9, 2025
Mnemonic:
SITS: Supraspinatus, Infraspinatus, Teres minor, Subscapularis
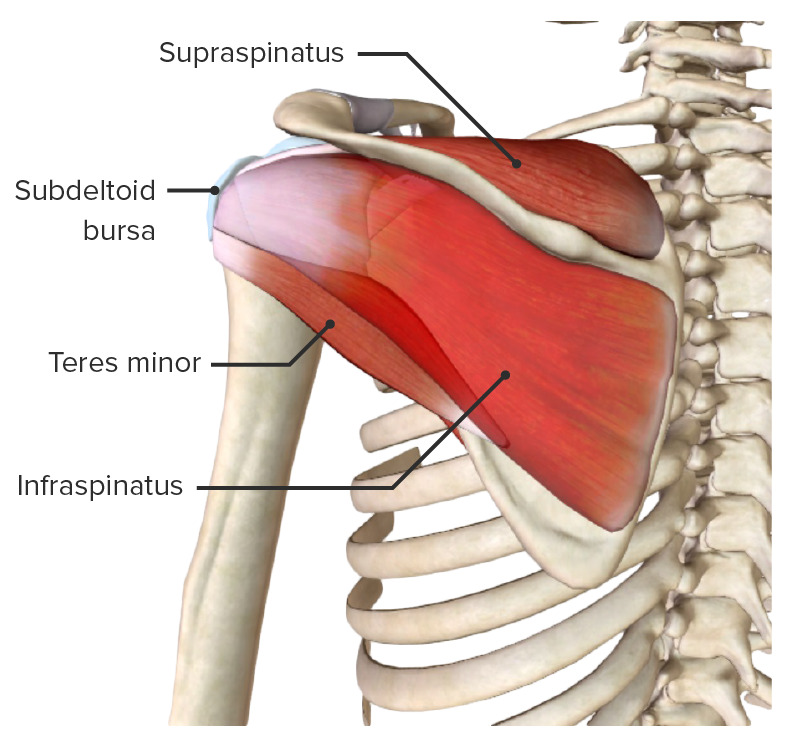
Posterior view of the scapular region and rotator cuff muscles (missing subscapularis)
Image by BioDigital, edited by Lecturio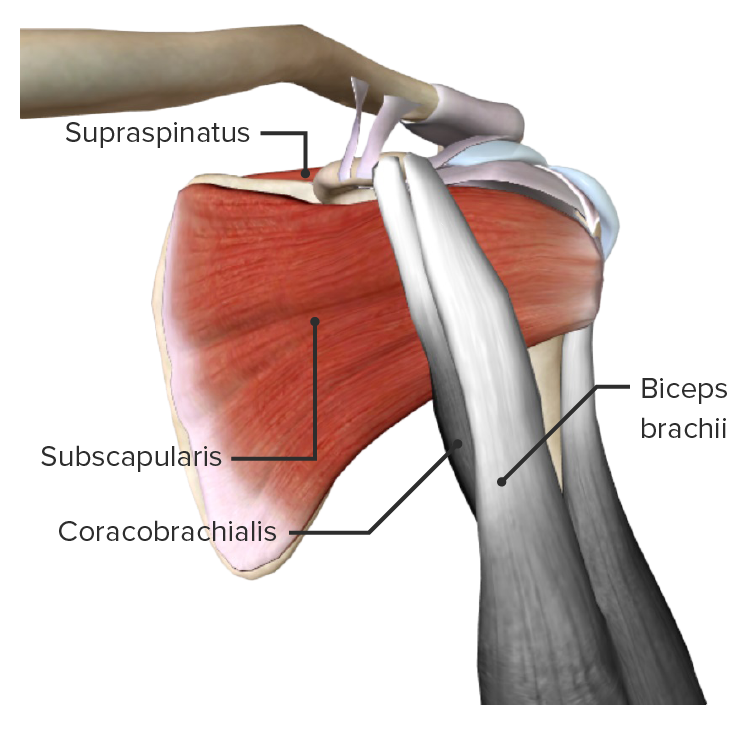
Anterior view of the scapular region featuring the subscapularis muscle (part of the rotator cuff muscles)
Image by BioDigital, edited by Lecturio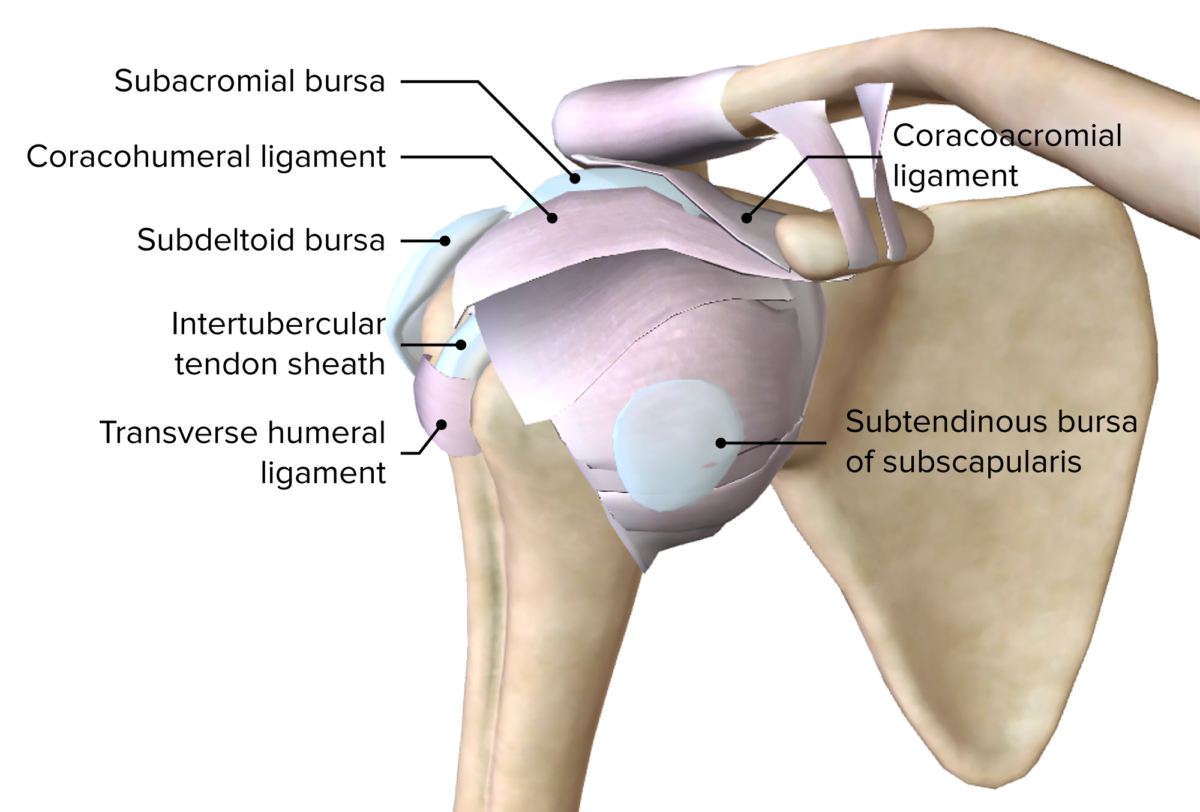
Anterior view of the superficial layer of ligaments and bursa of the right glenohumeral joint
Image by BioDigital, edited by Lecturio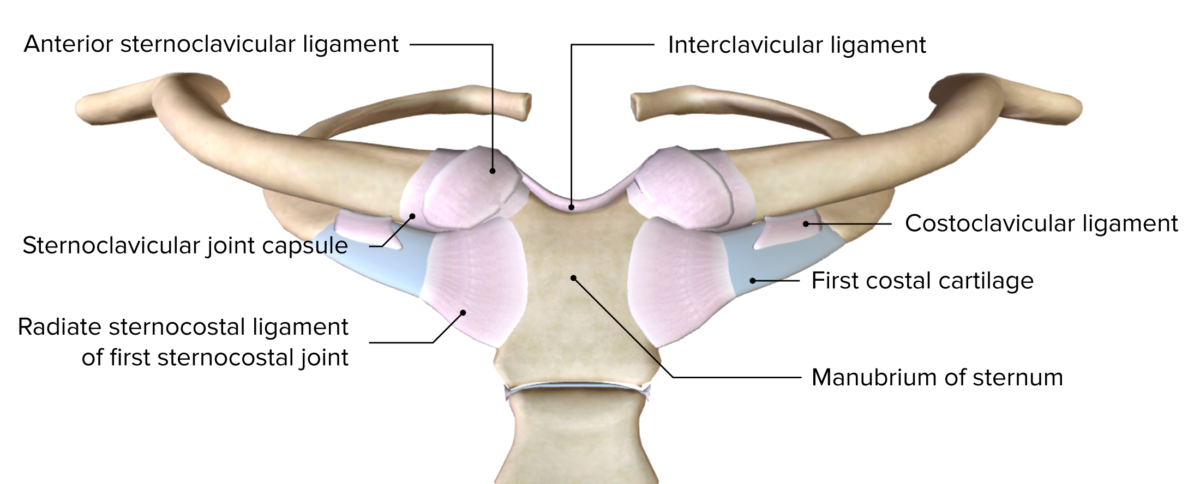
Anterior view of the sternoclavicular joint and the 1st sternocostal joint
Image by BioDigital, edited by LecturioImaging studies might be helpful to support or confirm the diagnosis:
Function of the supraspinatus muscle
Image: “Shoulder motion with rotator cuff” by Young Lae, Moon M.D. Chair of 3D Based Medical Application Working group. Chairman and Professor of Orthopaedics, Chosun University Hospital, Korea. License: CC BY 3.0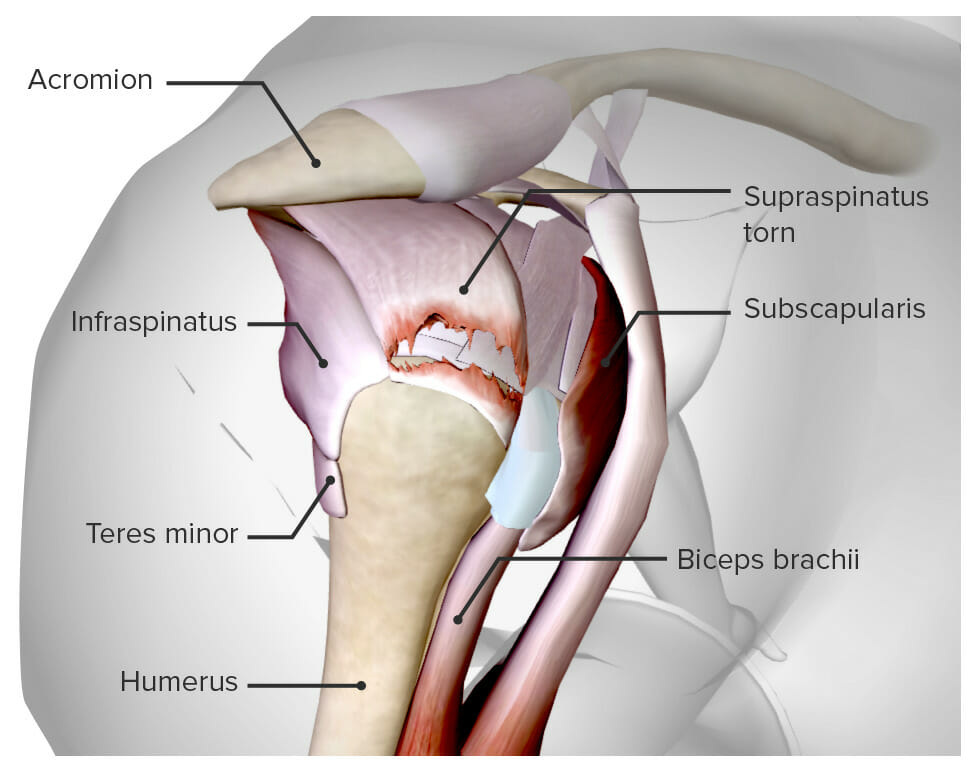
Diagram depicting a torn supraspinatus tendon
Image by BioDigital, edited by Lecturio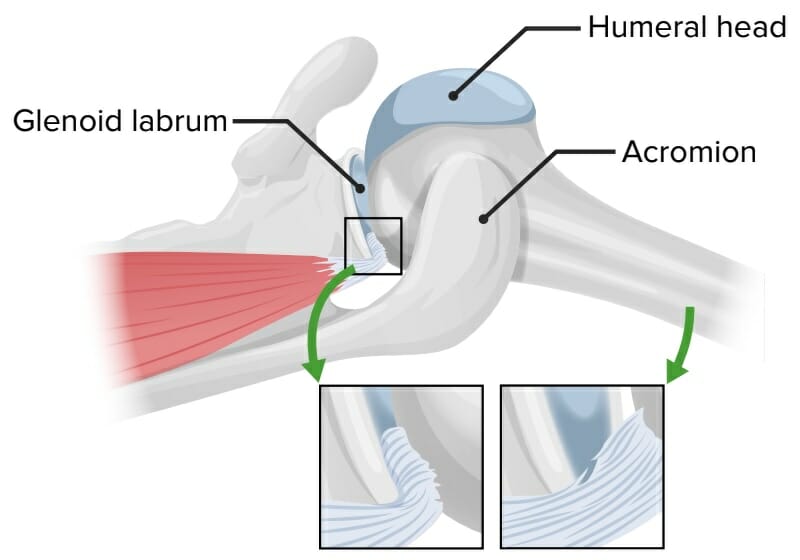
Mechanism of internal impingement:
Abduction and extreme external rotation associated with overhead throwing compress the supraspinatus and infraspinatus muscles and tendons between the posterosuperior glenoid rim, the posterior humeral head, and the
greater tuberosity, which cause the deep layers of the infraspinatus to fray.
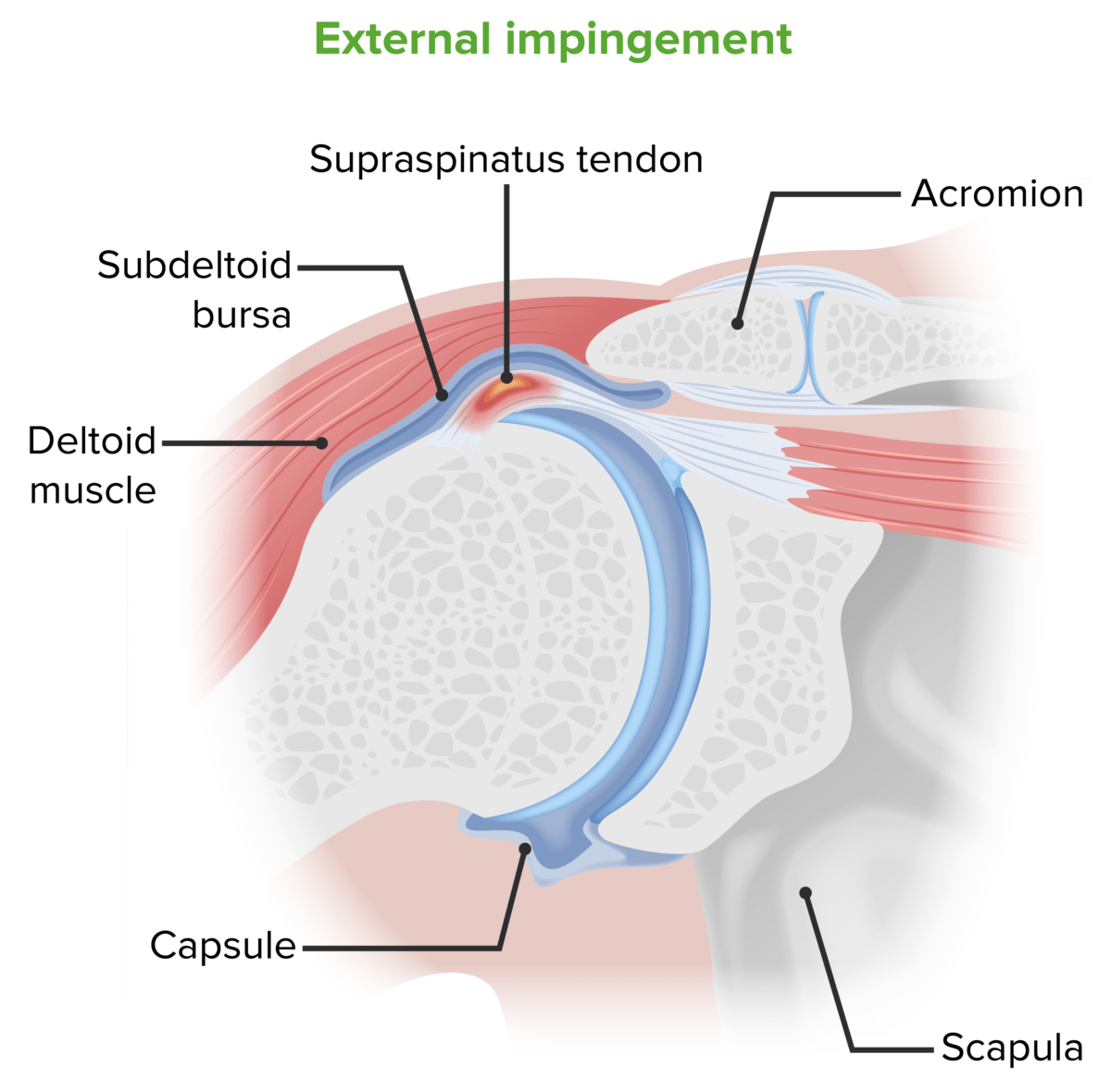
Mechanism of external impingement:
Repeated abduction of the arm causes impingement of the greater tuberosity of the humerus on the acromion, which causes degeneration and inflammation of the supraspinatus tendon.

Coronal oblique T2-weighted magnetic resonance image (MRI) showing a full-thickness rotator cuff tear (arrow). The high signal intensity fluid replacing the insertion of the supraspinatus tendon at the greater tuberosity indicates the tear.
Image: “Coronal oblique T2-weighted magnetic resonance image showing full-thickness rotator cuff tear” by Naqvi GA, Jadaan M, Harrington P. License: CC BY 2.0Biceps Biceps Arm: Anatomy tendinopathy or rupture:
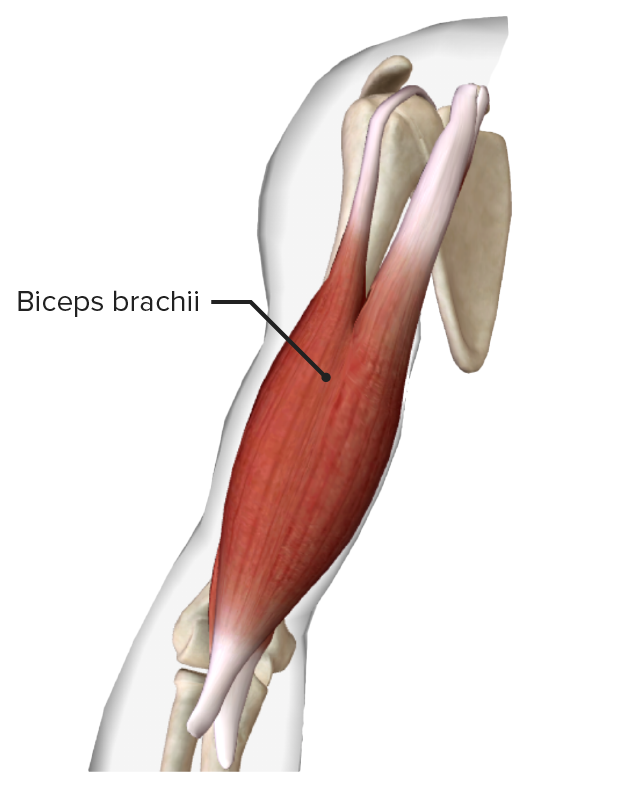
Biceps brachii muscle
Image by BioDigital, edited by Lecturio
“Popeye sign”: pathognomonic of distal biceps tendon rupture
Image: ““Popeye sign” by Ennaciri B, Beaudouin E, Mahfoud M, Berrada MS, Montbarbon E. License: CC BY 2.0Acromioclavicular joint Acromioclavicular joint The gliding joint formed by the outer extremity of the clavicle and the inner margin of the acromion process of the scapula. Examination of the Upper Limbs pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways:
Sternoclavicular joint Sternoclavicular Joint Examination of the Upper Limbs pathology:
Adhesive capsulitis (frozen shoulder):
Glenohumeral OA OA Osteoarthritis (OA) is the most common form of arthritis, and is due to cartilage destruction and changes of the subchondral bone. The risk of developing this disorder increases with age, obesity, and repetitive joint use or trauma. Patients develop gradual joint pain, stiffness lasting < 30 minutes, and decreased range of motion. Osteoarthritis:
Chronic instability of the shoulder:
Superior Labral tear from Anterior to Posterior (SLAP) lesion: