Acute shoulder injuries are a common reason for visits to primary care physicians Physicians Individuals licensed to practice medicine. Clinician–Patient Relationship and EDs EDS Ehlers-danlos syndrome (EDS) is a heterogeneous group of inherited connective tissue disorders that are characterized by hyperextensible skin, hypermobile joints, and fragility of the skin and connective tissue. Ehlers-Danlos Syndrome. Common injuries include clavicle Clavicle A bone on the ventral side of the shoulder girdle, which in humans is commonly called the collar bone. Clavicle Fracture fractures, sternoclavicular sprains and dislocations, rotator cuff tears, proximal humerus Humerus Bone in humans and primates extending from the shoulder joint to the elbow joint. Arm: Anatomy fractures, scapular fractures, glenohumeral dislocations, and acromioclavicular joint Acromioclavicular joint The gliding joint formed by the outer extremity of the clavicle and the inner margin of the acromion process of the scapula. Examination of the Upper Limbs injuries. Evaluation of acute shoulder pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways requires an understanding of the mechanism of injury, as well as the appropriate physical examination and radiologic studies needed in the acute setting. A focused history and physical examination is essential and should include inspection Inspection Dermatologic Examination, palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination, and a thorough neurovascular exam. Imaging begins with plain radiographs and is occasionally supplemented by MRI or CT imaging. Management includes pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways control and varies based on diagnosis.
Last updated: Nov 21, 2022
Remember the rotator cuff muscles with SITS:
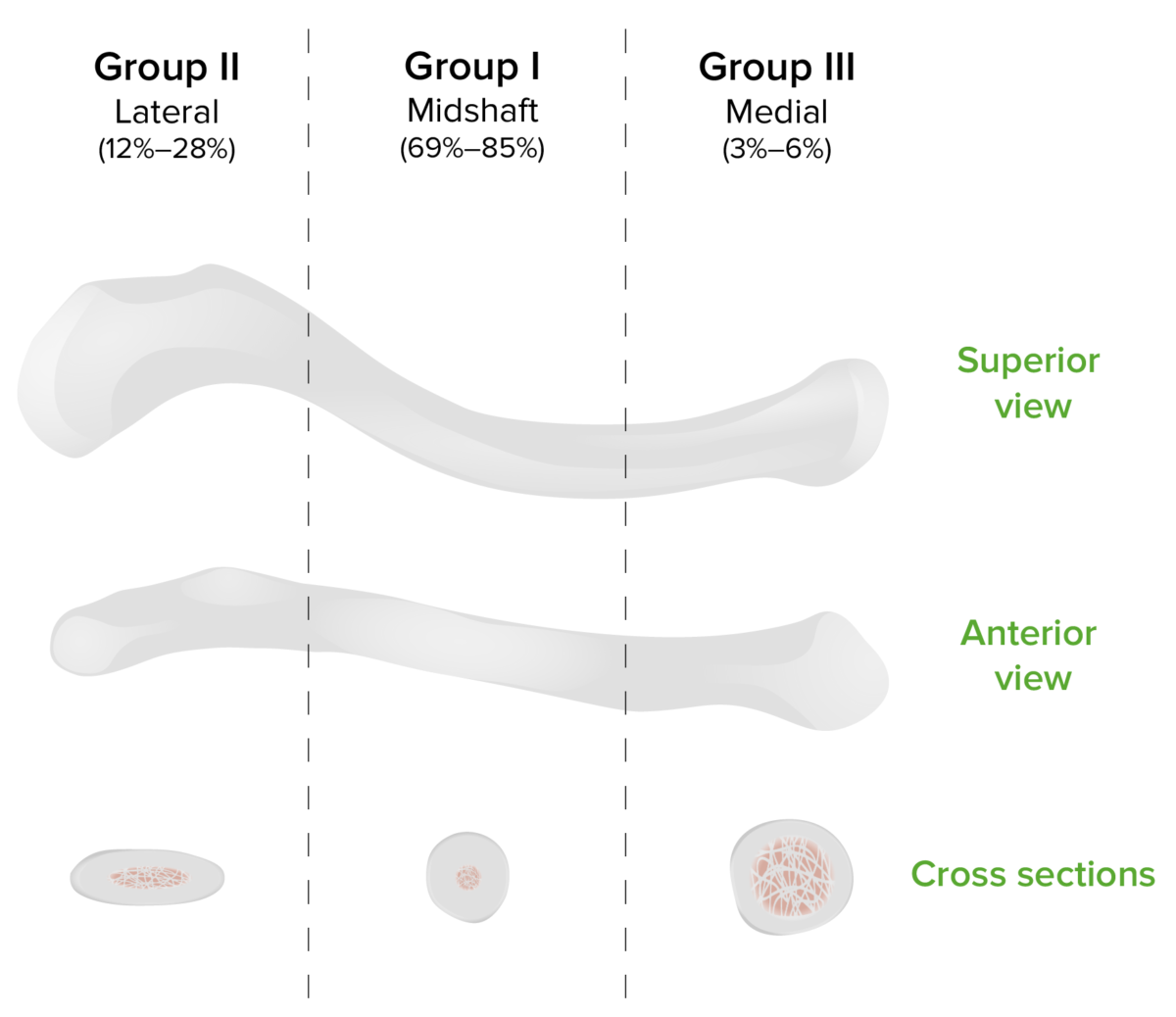
Allman classification of clavicular fracture
Image by Lecturio.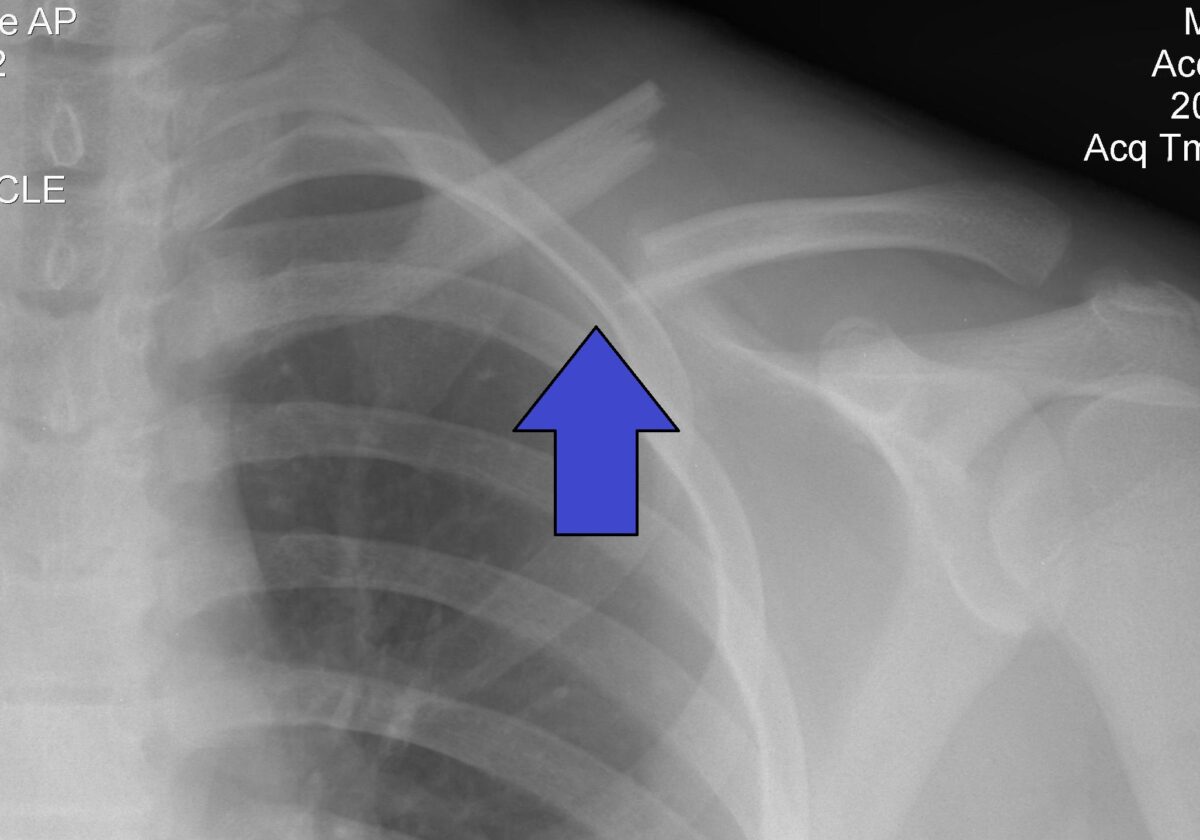
Group 1 clavicle fracture indicated by the arrow
Image: “Clavicle Fracture Left” by Majorkev. License: CC BY 3.0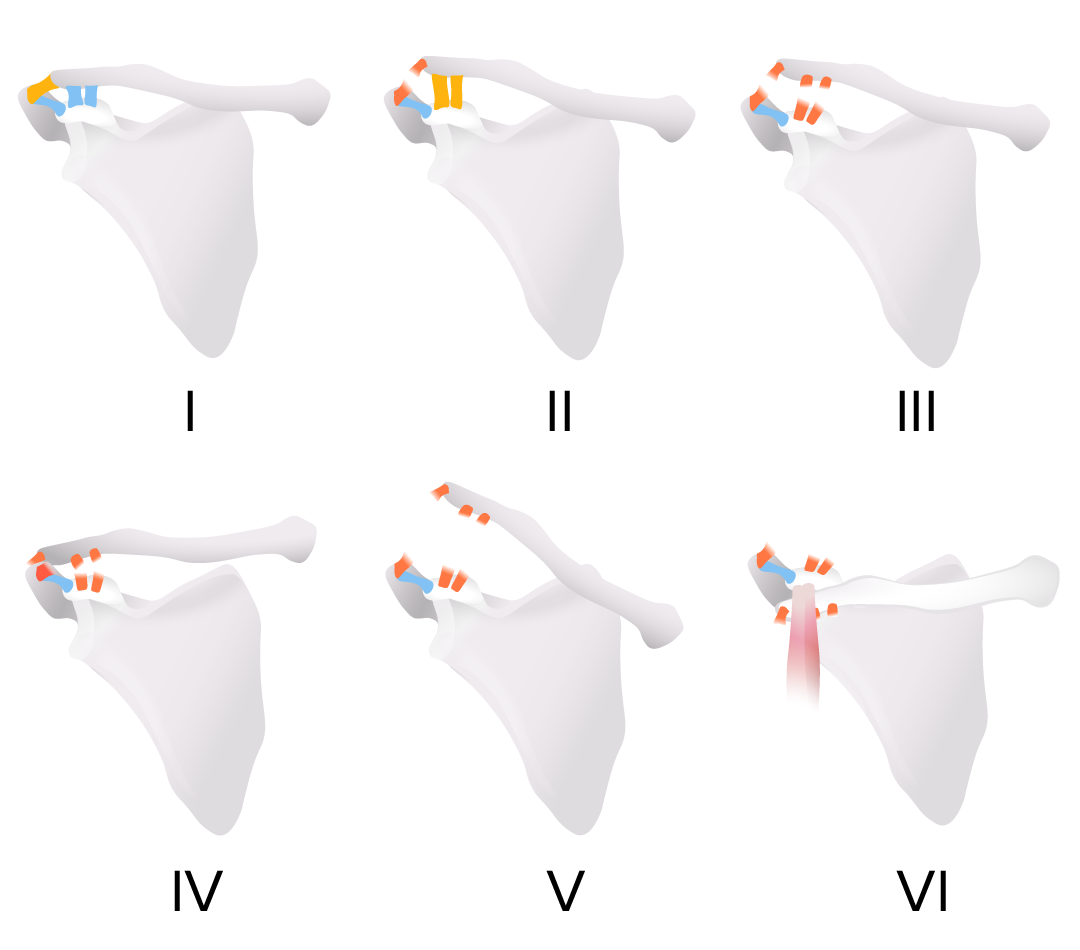
Rockwood classification of acromioclavicular joint injury
Image by Lecturio.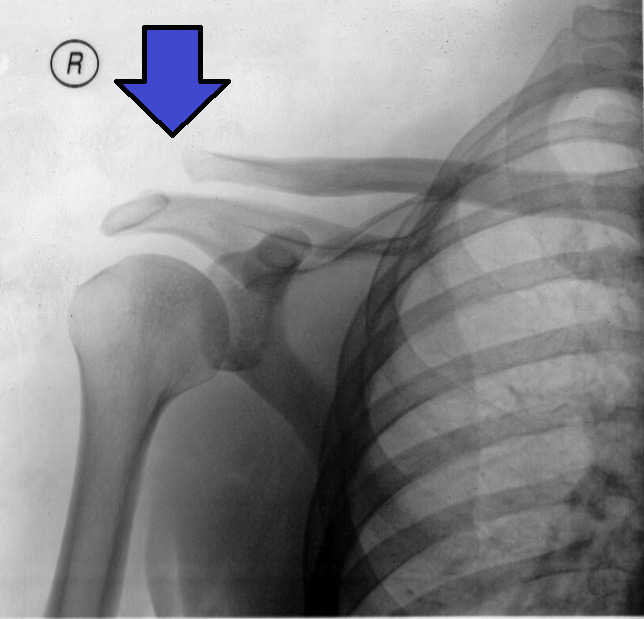
Type III acromioclavicular joint injury on x-ray:
The arrow shows the clavicle above the level of the acromion, but not more than twice the normal distance.
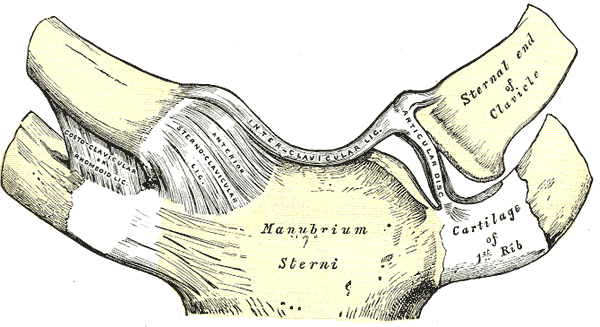
Normal anterior view of the sternoclavicular joint
Image: “Gray325” by Henry Gray, Warren H. Lewis. License: Public Domain
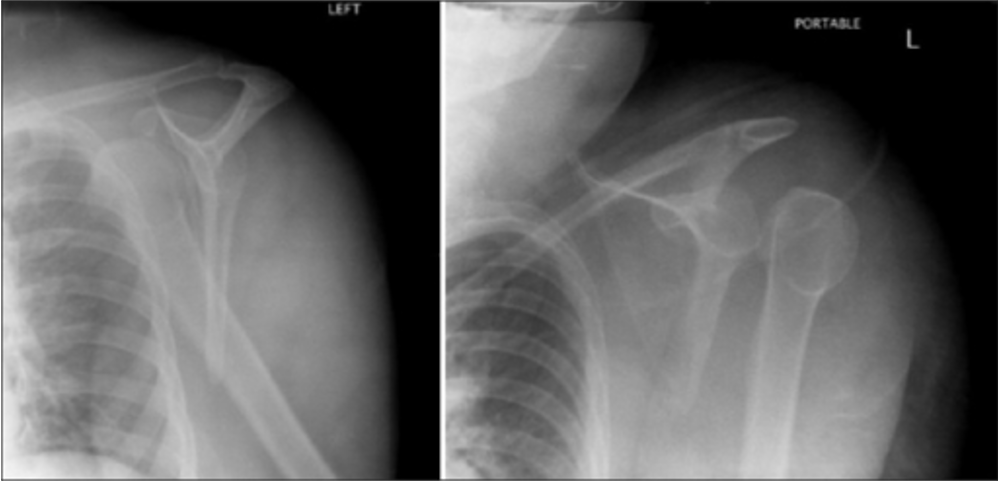
Scapular Y views of anterior (left) and posterior (right) dislocation of the left shoulder
Image: “Scapular Y views of (a) anterior and (b) posterior dislocation of the left shoulder” by Day MS, Epstein DM, Young BH, Jazrawi LM. License: CC BY 2.0
Normal Y-view X-ray
Image: “Y-projection X-ray of a normal shoulder” by Mikael Häggström. License: CC0 1.0
X-ray of a proximal humerus fracture
Image: “X-Ray images showing the progression from injury (a) to 7 days after (b) a non-operative approach” by Woojin Chae, Akib Khan, Sarah Abbott, Angelos Assiotis. License: CC BY 4.0
Full-thickness rotator cuff tear (arrow) shown on a coronal-oblique T2-weighted MRI: The high signal intensity of fluid replacing the insertion of the supraspinatus tendon at the greater tuberosity indicates a tear.
Image: “F0003: Coronal-oblique T2-weighted magnetic resonance image showing full-thickness rotator cuff tear (arrow), indicated by high signal intensity fluid replacing the insertion of the supraspinatus tendon at the greater tuberosity” by Gohar Abbas Naqvi, Mutaz Jadaan, and Paul Harrington. License: CC BY 2.0