Subdural hemorrhage Subdural Hemorrhage Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral "bridging" veins. Subdural Hemorrhage ( SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral "bridging" veins. Subdural Hemorrhage) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury Closed Head Injury Subdural Hemorrhage) causing a tearing injury to the extracerebral “bridging” veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology, but rupture of small arteries Small arteries Arteries: Histology within this space or intracranial hypotension Intracranial hypotension Reduction of cerebrospinal fluid pressure characterized clinically by orthostatic headache and occasionally by an abducens nerve palsy; hearing loss; nausea; neck stiffness, and other symptoms. This condition may be spontaneous or secondary to cerebrospinal fluid leak; spinal puncture; neurosurgical procedures; dehydration; uremia; trauma; and other processes. Chronic hypotension may be associated with subdural hematomas or hygromas. Subdural Hemorrhage may also be causative. Acute SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral "bridging" veins. Subdural Hemorrhage presents, immediately following head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma, with an altered level of consciousness Altered Level of Consciousness Intracerebral Hemorrhage that may span from a momentary loss of consciousness to coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma, which makes it a potentially life-threatening condition. Chronic SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral "bridging" veins. Subdural Hemorrhage may also occur, presenting with a more gradual neurologic deterioration. Diagnosis is based on clinical suspicion following head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma and confirmed with neuroimaging Neuroimaging Non-invasive methods of visualizing the central nervous system, especially the brain, by various imaging modalities. Febrile Infant (e.g., noncontrast head CT). Management includes stabilization, stopping (possibly reversing) all anticoagulants Anticoagulants Anticoagulants are drugs that retard or interrupt the coagulation cascade. The primary classes of available anticoagulants include heparins, vitamin K-dependent antagonists (e.g., warfarin), direct thrombin inhibitors, and factor Xa inhibitors. Anticoagulants, monitoring in a neurologic ICU ICU Hospital units providing continuous surveillance and care to acutely ill patients. West Nile Virus, and neurosurgical intervention.
Last updated: Mar 4, 2024
Subdural hematoma Hematoma A collection of blood outside the blood vessels. Hematoma can be localized in an organ, space, or tissue. Intussusception ( SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral “bridging” veins. Subdural Hemorrhage) is bleeding, usually caused by head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma, into the space between the dural and arachnoid meningeal layers surrounding the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, creating a space called the subdural space Subdural space Potential cavity which separates the arachnoid mater from the dura mater. Subdural Hemorrhage.[1]
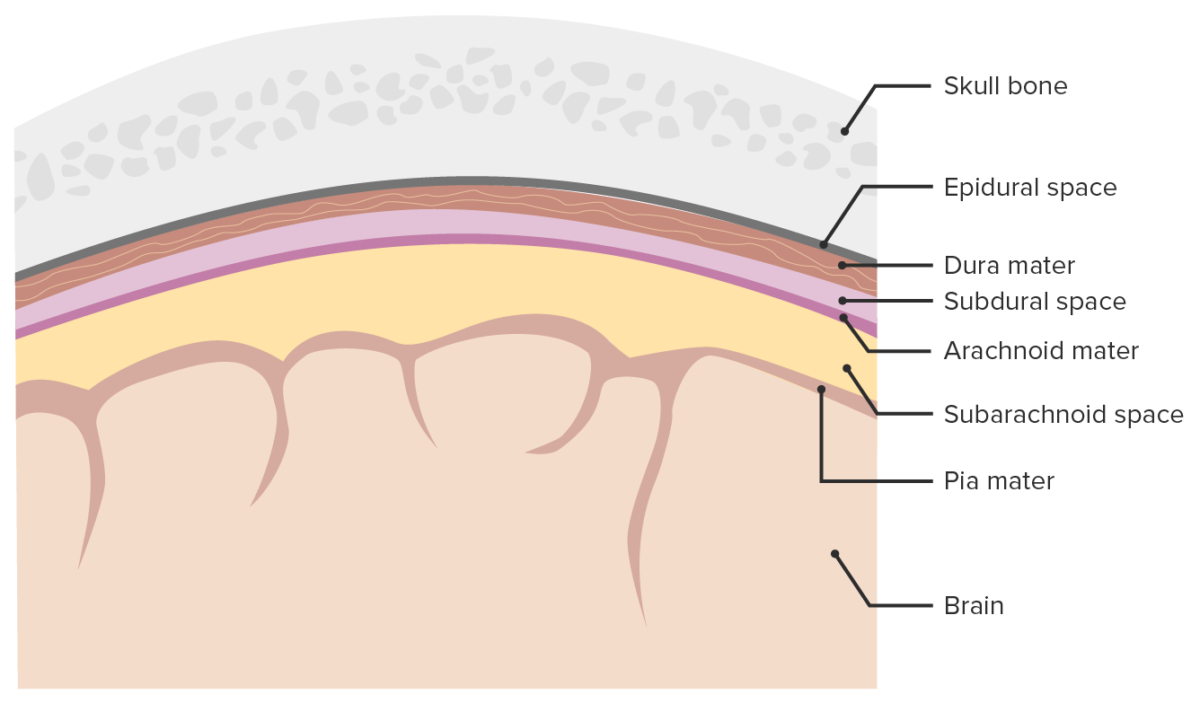
Meninges and meningeal spaces:
The image depicts the 3 layers (dura mater, arachnoid mater, and pia mater) surrounding the brain and spinal cord. The meninges serve as mechanical protection of the CNS. The meninges also support the cerebral and spinal blood vessels and allow for passage of the CSF. The subarachnoid space is filled with CSF. Only the subarachnoid space is a true space present in physiologic conditions, whereas the epidural and subdural spaces form only because of pathologic processes. The subdural space opens if the arachnoid mater separates from the dura mater, most commonly because of trauma and pathologic processes.
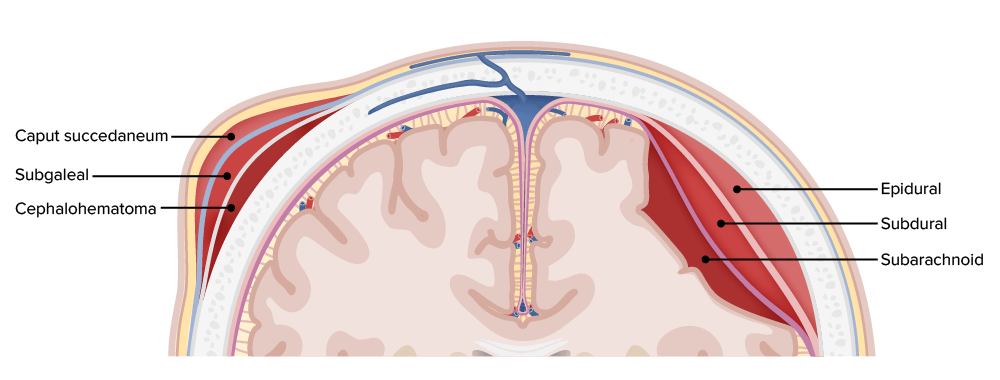
Hemorrhages by location within the different layers of the meninges and scalp
Image by Lecturio.SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral “bridging” veins. Subdural Hemorrhage is caused by rupture of vasculature (typically bridging veins Bridging Veins Subdural Hemorrhage) between the arachnoid and dural meningeal layers. The primary etiology is trauma.
Acute SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral “bridging” veins. Subdural Hemorrhage:
Chronic SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral “bridging” veins. Subdural Hemorrhage:
The 2 main risk factors are cerebral atrophy Cerebral Atrophy Subdural Hemorrhage and antithrombotic therapy.[1,5]
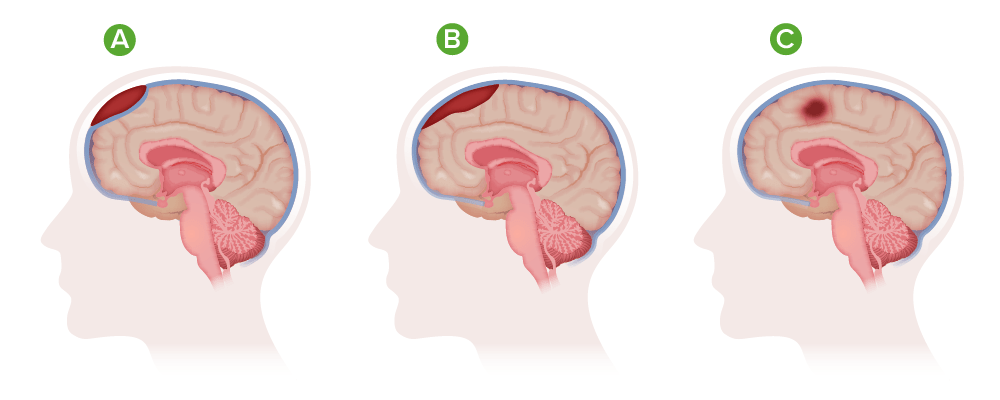
Types of hematoma:
A) Epidural;
B) Subdural;
C) Intracranial
SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral “bridging” veins. Subdural Hemorrhage occurs because of bleeding within the subdural space Subdural space Potential cavity which separates the arachnoid mater from the dura mater. Subdural Hemorrhage. This may resolve by resorption or may become chronic by membranous encapsulation.[1,6]
Acute subdural hematoma Acute Subdural Hematoma Accumulation of blood in the subdural space with acute onset of neurological symptoms. Symptoms may include loss of consciousness, severe headache, and deteriorating mental status. Subdural Hemorrhage:[1]
Chronic subdural hematoma Chronic Subdural Hematoma Accumulation of blood in the subdural space with delayed onset of neurological symptoms. Symptoms may include loss of consciousness, severe headache, and deteriorating mental status. Subdural Hemorrhage:[1]
Acute-on-chronic SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral “bridging” veins. Subdural Hemorrhage:[1,8]
Neurologic presentation depends on the size, location, and rate of growth of the hematoma Hematoma A collection of blood outside the blood vessels. Hematoma can be localized in an organ, space, or tissue. Intussusception, as well as the length of time since the initiating event.[1,6]
Onset of symptoms:[3,6]
Neurologic symptoms and signs:[5]
Suspect SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral “bridging” veins. Subdural Hemorrhage in any elderly person presenting with head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma, altered mental status Altered Mental Status Sepsis in Children, decreased level of consciousness, or neurologic symptoms/signs. Head CT should be performed emergently.[3,6]
Noncontrast head CT:
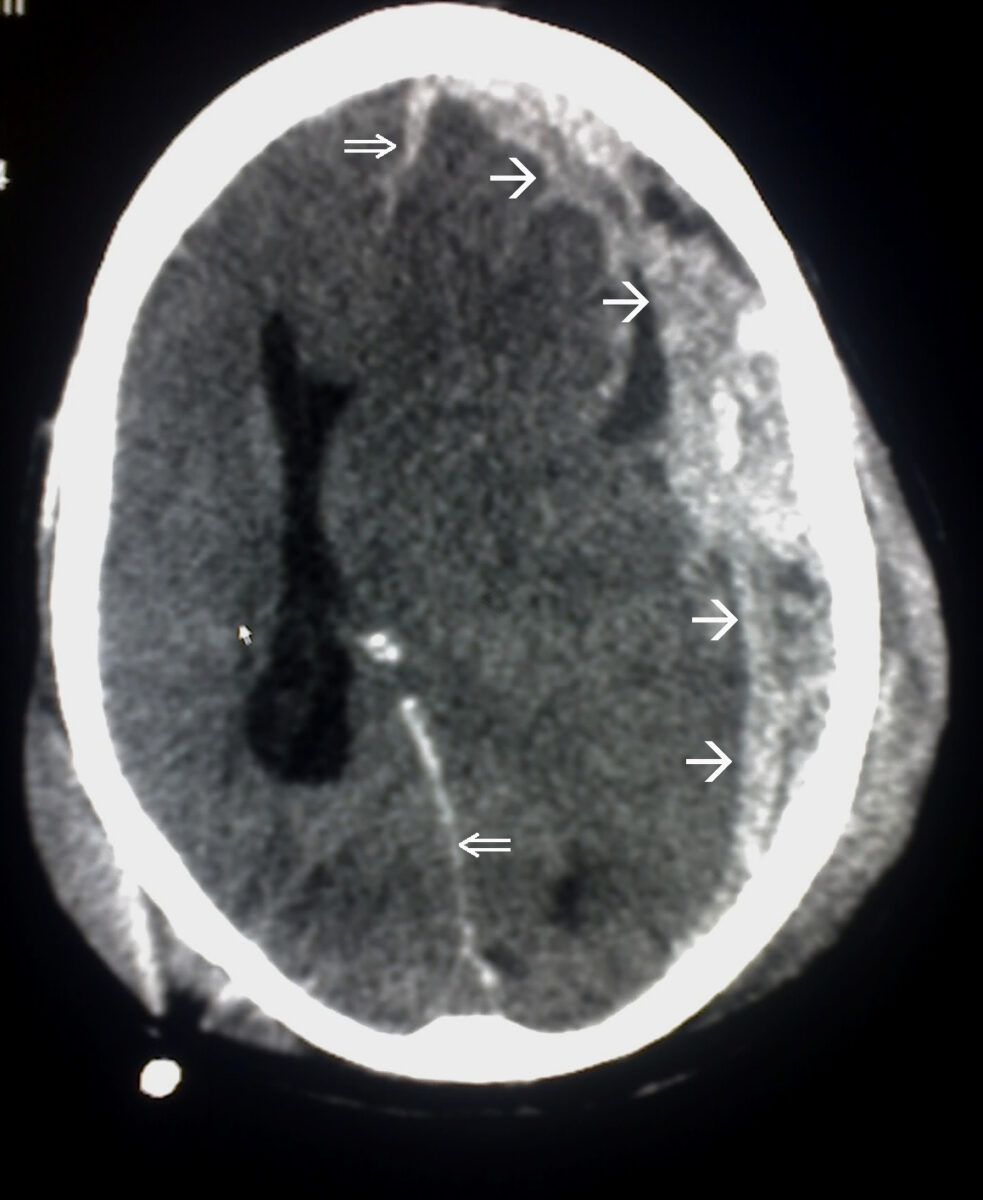
Subdural hemorrhage:
Note the convexity of the hematoma and associated midline shift (with distortion of cerebral anatomy and obliteration of the lateral ventricle).
Head MRI:
Angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery:
Lumbar puncture Lumbar Puncture Febrile Infant:[1]
Acute SDH SDH Subdural hemorrhage (SDH) is bleeding into the space between the dural and arachnoid meningeal layers surrounding the brain. The most common mechanism triggering the bleeding event is trauma (e.g., closed head injury) causing a tearing injury to the extracerebral “bridging” veins. Subdural Hemorrhage, especially that presenting with neurologic compromise or coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma, is an emergent neurologic situation often requiring surgical intervention. Failure to promptly stabilize, diagnose, evaluate, and intervene could result in hemorrhagic expansion, parenchymal brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification injury, elevated ICP ICP Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP), brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification herniation Herniation Omphalocele, and death.[1,3,6,7]
Clinical decision tools used to determine operative or nonoperative management include: