Substance use disorders are a significant cause of morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and mortality Mortality All deaths reported in a given population. Measures of Health Status, especially among adolescents and young adults. A substance-related (addictive disorder) is the continued use of a substance despite harmful consequences; these include significant impairment to one’s health or relationships or failure to fulfill major responsibilities at work, school, or home because of substance use. There are several individual substance use disorders, and they are linked by their chronicity and the significant impairment they cause. Most substance use disorders have associated intoxication and withdrawal symptoms. Treatment options include pharmacotherapy and behavioral interventions; however, individuals with substance use disorders have frequent relapse Relapse Relapsing Fever/ remission Remission A spontaneous diminution or abatement of a disease over time, without formal treatment. Cluster Headaches as well as low compliance Compliance Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure. Veins: Histology with treatment.
Last updated: Feb 28, 2025
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) Work Group revisions combined abuse and dependence criteria from previous classifications into a single substance use disorder.
A substance-related (addictive disorder) is the continued use of a substance despite harmful consequences, including significant impairment to one’s health or relationships or failure to fulfill major responsibilities at work, school, or home due to substance use.
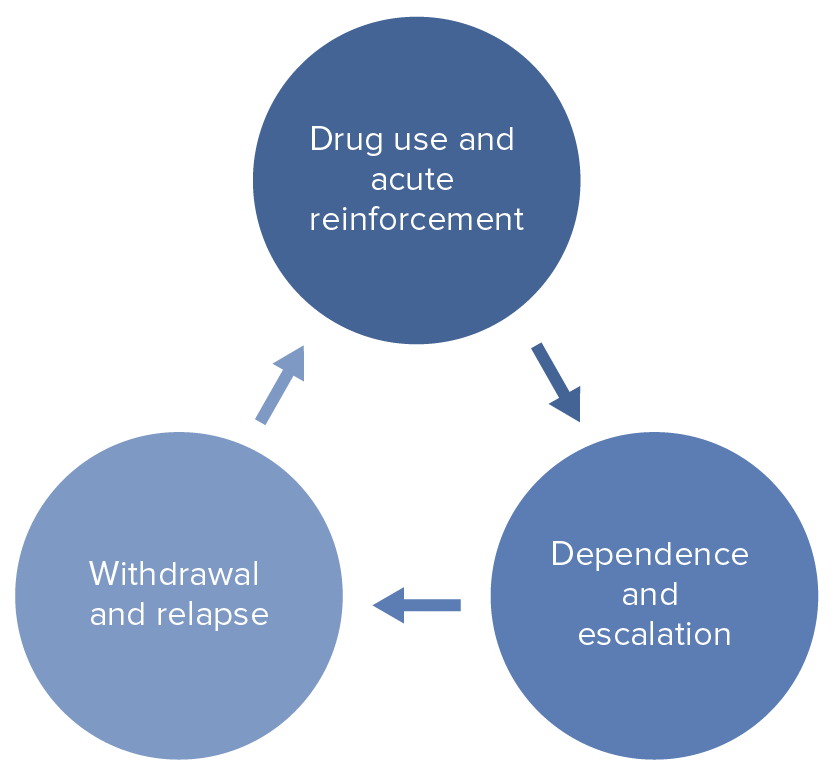
Cycle of substance-related and addictive disorders
Image by Lecturio.Substance use disorder assessments should establish the type of substance(s) used as well as the frequency, amount, and whether other mental health disorders (mood disorders, schizophrenia Schizophrenia Schizophrenia is a chronic mental health disorder characterized by the presence of psychotic symptoms such as delusions or hallucinations. The signs and symptoms of schizophrenia are traditionally separated into 2 groups: positive (delusions, hallucinations, and disorganized speech or behavior) and negative (flat affect, avolition, anhedonia, poor attention, and alogia). Schizophrenia, personality disorders Personality Disorders A major deviation from normal patterns of behavior. Cluster A Personality Disorders) or past history of substance use disorder are present.
Substances causing pupil Pupil The pupil is the space within the eye that permits light to project onto the retina. Anatomically located in front of the lens, the pupil’s size is controlled by the surrounding iris. The pupil provides insight into the function of the central and autonomic nervous systems. Pupil: Physiology and Abnormalities dilation:
Substances causing pupil Pupil The pupil is the space within the eye that permits light to project onto the retina. Anatomically located in front of the lens, the pupil’s size is controlled by the surrounding iris. The pupil provides insight into the function of the central and autonomic nervous systems. Pupil: Physiology and Abnormalities constriction:
| Substance | Intoxication findings | Management |
|---|---|---|
| Nicotine Nicotine Nicotine is highly toxic alkaloid. It is the prototypical agonist at nicotinic cholinergic receptors where it dramatically stimulates neurons and ultimately blocks synaptic transmission. Nicotine is also important medically because of its presence in tobacco smoke. Stimulants/tobacco |
|
Supportive treatment |
| Cocaine Cocaine An alkaloid ester extracted from the leaves of plants including coca. It is a local anesthetic and vasoconstrictor and is clinically used for that purpose, particularly in the eye, ear, nose, and throat. It also has powerful central nervous system effects similar to the amphetamines and is a drug of abuse. Cocaine, like amphetamines, acts by multiple mechanisms on brain catecholaminergic neurons; the mechanism of its reinforcing effects is thought to involve inhibition of dopamine uptake. Local Anesthetics |
|
|
| Amphetamines Amphetamines Analogs or derivatives of amphetamine. Many are sympathomimetics and central nervous system stimulators causing excitation, vasopressin, bronchodilation, and to varying degrees, anorexia, analepsis, nasal decongestion, and some smooth muscle relaxation. Stimulants |
|
|
| Synthetic canthinones (“bath salts”): a stimulant found naturally in the khat plant |
|
| Substance | Intoxication findings | Management |
|---|---|---|
| Alcohol |
|
|
| Opioids Opioids Opiates are drugs that are derived from the sap of the opium poppy. Opiates have been used since antiquity for the relief of acute severe pain. Opioids are synthetic opiates with properties that are substantially similar to those of opiates. Opioid Analgesics |
|
|
| Sedatives and hypnotics ( benzodiazepines Benzodiazepines Benzodiazepines work on the gamma-aminobutyric acid type A (GABAA) receptor to produce inhibitory effects on the CNS. Benzodiazepines do not mimic GABA, the main inhibitory neurotransmitter in humans, but instead potentiate GABA activity. Benzodiazepines, barbiturates Barbiturates A class of chemicals derived from barbituric acid or thiobarbituric acid. Many of these are gaba modulators used as hypnotics and sedatives, as anesthetics, or as anticonvulsants. Intravenous Anesthetics) |
|
|
| Substance | Intoxication findings | Management |
|---|---|---|
| Cannabis |
|
|
| Hallucinogens (e.g., phencyclidine ( PCP PCP Pneumocystis jiroveci is a yeast-like fungus causing pneumocystis pneumonia (PCP) in immunocompromised patients. Pneumocystis pneumonia is spread through airborne transmission and classically affects patients with AIDS, functioning as an AIDS-defining illness. Patients may present with insidious onset of fever, chills, dry cough, chest pain, and shortness of breath. Pneumocystis jirovecii/Pneumocystis Pneumonia (PCP))) |
|
|
| Hallucinogens (e.g., LSD) |
|
|
| Ecstasy Ecstasy An n-substituted amphetamine analog. It is a widely abused drug classified as a hallucinogen and causes marked, long-lasting changes in brain serotonergic systems. It is commonly referred to as mdma or ecstasy. Stimulants ( methylenedioxymethamphetamine Methylenedioxymethamphetamine An n-substituted amphetamine analog. It is a widely abused drug classified as a hallucinogen and causes marked, long-lasting changes in brain serotonergic systems. It is commonly referred to as mdma or ecstasy. Stimulants ( MDMA MDMA An n-substituted amphetamine analog. It is a widely abused drug classified as a hallucinogen and causes marked, long-lasting changes in brain serotonergic systems. It is commonly referred to as mdma or ecstasy. Stimulants)) |
|
|
| Inhalants |
|
|
| Substance | Withdrawal findings | Management |
|---|---|---|
| Nicotine Nicotine Nicotine is highly toxic alkaloid. It is the prototypical agonist at nicotinic cholinergic receptors where it dramatically stimulates neurons and ultimately blocks synaptic transmission. Nicotine is also important medically because of its presence in tobacco smoke. Stimulants/tobacco |
|
|
| Cocaine Cocaine An alkaloid ester extracted from the leaves of plants including coca. It is a local anesthetic and vasoconstrictor and is clinically used for that purpose, particularly in the eye, ear, nose, and throat. It also has powerful central nervous system effects similar to the amphetamines and is a drug of abuse. Cocaine, like amphetamines, acts by multiple mechanisms on brain catecholaminergic neurons; the mechanism of its reinforcing effects is thought to involve inhibition of dopamine uptake. Local Anesthetics |
|
|
| Amphetamines Amphetamines Analogs or derivatives of amphetamine. Many are sympathomimetics and central nervous system stimulators causing excitation, vasopressin, bronchodilation, and to varying degrees, anorexia, analepsis, nasal decongestion, and some smooth muscle relaxation. Stimulants, synthetic canthinones (“bath salts”) |
|
|
| Substance | Withdrawal findings | Management |
|---|---|---|
| Alcohol |
|
|
| Opioids Opioids Opiates are drugs that are derived from the sap of the opium poppy. Opiates have been used since antiquity for the relief of acute severe pain. Opioids are synthetic opiates with properties that are substantially similar to those of opiates. Opioid Analgesics |
|
|
| Sedatives and hypnotics ( benzodiazepines Benzodiazepines Benzodiazepines work on the gamma-aminobutyric acid type A (GABAA) receptor to produce inhibitory effects on the CNS. Benzodiazepines do not mimic GABA, the main inhibitory neurotransmitter in humans, but instead potentiate GABA activity. Benzodiazepines, barbiturates Barbiturates A class of chemicals derived from barbituric acid or thiobarbituric acid. Many of these are gaba modulators used as hypnotics and sedatives, as anesthetics, or as anticonvulsants. Intravenous Anesthetics) |
|
|
| Substance | Withdrawal findings | Management |
|---|---|---|
| Cannabis |
|
|
| Inhalants |
|
|
| Ecstasy Ecstasy An n-substituted amphetamine analog. It is a widely abused drug classified as a hallucinogen and causes marked, long-lasting changes in brain serotonergic systems. It is commonly referred to as mdma or ecstasy. Stimulants |
|
|
The DSM-5 uses 11 criteria (including dependence criteria, abuse criteria, and craving) to classify substance use disorders. There are separate criteria for substance intoxication and withdrawal.
Diagnosis is made by a problematic pattern of use leading to significant impairment or distress manifested by ≥ 2 of the following in a 12-month period:
Impaired control:
Social impairment:
Risky use:
Pharmacologic criteria inherent to the substance:
Other factors relevant to diagnosis:
Substance use disorders often coexist with other medical and psychiatric conditions.