Insulinotropic diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus medications treat type 2 diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus by increasing insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin secretion Secretion Coagulation Studies, which results in decreased glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance levels. The group of medications includes sulfonylureas Sulfonylureas Sulfonamides and Trimethoprim, meglitinides, glucagon-like peptide-1 ( GLP-1 GLP-1 A peptide of 36 or 37 amino acids that is derived from proglucagon and mainly produced by the intestinal l cells. Glp-1(1-37 or 1-36) is further n-terminally truncated resulting in glp-1(7-37) or glp-1-(7-36) which can be amidated. These glp-1 peptides are known to enhance glucose-dependent insulin release, suppress glucagon release and gastric emptying, lower blood glucose, and reduce food intake. Insulinomas) receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors agonists, and DPP-4 inhibitors. The agents are usually used in combination with other therapies for diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus management. Sulfonylureas Sulfonylureas Sulfonamides and Trimethoprim and meglitinides are associated with weight gain, while GLP-1 GLP-1 A peptide of 36 or 37 amino acids that is derived from proglucagon and mainly produced by the intestinal l cells. Glp-1(1-37 or 1-36) is further n-terminally truncated resulting in glp-1(7-37) or glp-1-(7-36) which can be amidated. These glp-1 peptides are known to enhance glucose-dependent insulin release, suppress glucagon release and gastric emptying, lower blood glucose, and reduce food intake. Insulinomas agonists may provide the added benefit of weight loss Weight loss Decrease in existing body weight. Bariatric Surgery. Other side effects vary between the drug classes. None of the medications should be used in the treatment of type 1 Type 1 Spinal Muscular Atrophy diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus or diabetic ketoacidosis Ketoacidosis A life-threatening complication of diabetes mellitus, primarily of type 1 diabetes mellitus with severe insulin deficiency and extreme hyperglycemia. It is characterized by ketosis; dehydration; and depressed consciousness leading to coma. Metabolic Acidosis.
Last updated: Jul 3, 2024
Hypoglycemic (or antihyperglycemic) medications can be classified based on the mechanism of action:
Insulinotropic drugs (↑ insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin secretion Secretion Coagulation Studies):
Non-insulinotropic drugs (do not affect insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin release):
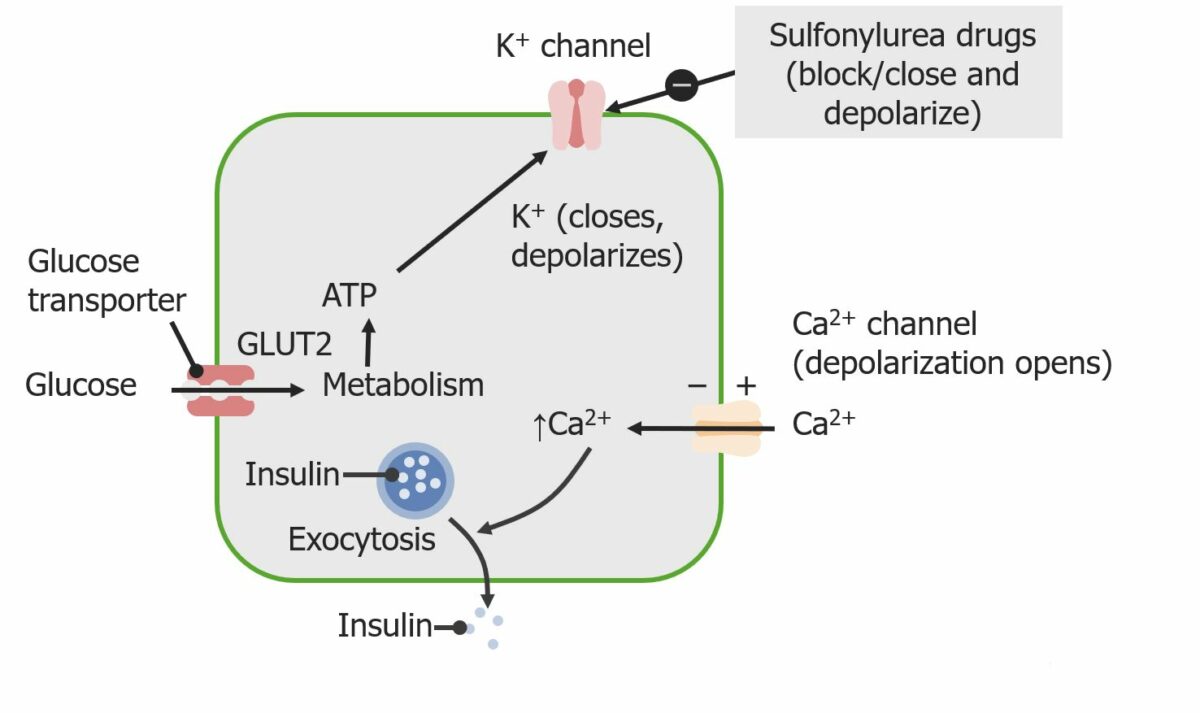
Sulfonylureas stimulate insulin secretion by acting on potassium channels of pancreatic beta cells.
Image by Lecturio.The following describes the pharmacokinetics Pharmacokinetics Pharmacokinetics is the science that analyzes how the human body interacts with a drug. Pharmacokinetics examines how the drug is absorbed, distributed, metabolized, and excreted by the body. Pharmacokinetics and Pharmacodynamics for 2nd-generation sulfonylureas Sulfonylureas Sulfonamides and Trimethoprim:
Sulfonylureas Sulfonylureas Sulfonamides and Trimethoprim are used in the treatment of type 2 diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus:
Meglitinides treat type 2 diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus:
An increased hypoglycemic effect may be seen with:
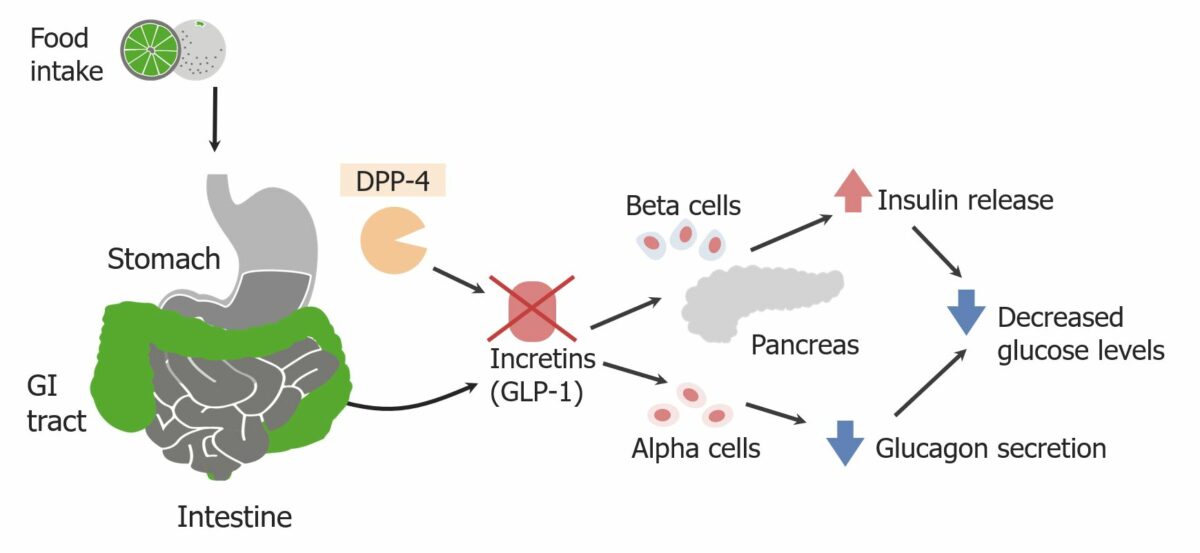
Normal function of DPP-4: Enzyme inhibition prevents the breakdown of glucagon-like peptide-1 (GLP-1), allowing for increased insulin release and decreased glucagon secretion.
Image by Lecturio.DPP-4 inhibitors treat type 2 diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus:
The following table compares type 2 diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus non-insulin medications:
| Drug | Mechanism | Indications | Adverse effects |
|---|---|---|---|
| Sulfonylureas Sulfonylureas Sulfonamides and Trimethoprim |
|
|
|
| Meglitinides |
|
|
|
| Glucagon-like protein-1 ( GLP-1 GLP-1 A peptide of 36 or 37 amino acids that is derived from proglucagon and mainly produced by the intestinal l cells. Glp-1(1-37 or 1-36) is further n-terminally truncated resulting in glp-1(7-37) or glp-1-(7-36) which can be amidated. These glp-1 peptides are known to enhance glucose-dependent insulin release, suppress glucagon release and gastric emptying, lower blood glucose, and reduce food intake. Insulinomas) agonists |
|
|
|
| DPP-4 inhibitors |
|
Adjunctive therapy |
|
| Biguanides Biguanides Derivatives of biguanide (the structure formula HN(C(NH)NH2)2) that are primarily used as oral hypoglycemic agents for the treatment of diabetes mellitus, type 2 and prediabetes. Non-insulinotropic Diabetes Drugs |
|
|
|
| Thiazolidinediones Thiazolidinediones Thiazoles with two keto oxygens. Members are insulin-sensitizing agents which overcome insulin resistance by activation of the peroxisome proliferator activated receptor gamma (ppar-gamma). Non-insulinotropic Diabetes Drugs |
|
|
|
| Alpha-glucosidase inhibitors Alpha-Glucosidase Inhibitors Non-insulinotropic Diabetes Drugs |
|
|
|
| Sodium-glucose transport protein 2 (SGLT2) inhibitors |
|
|
|
| Amylin analogs |
|
|
|
The effects of diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus medications on weight may be a factor in an individual’s therapy choice: