Chronic venous disease is a spectrum of disorders characterized by venous dilation and/or abnormal vein function in the lower extremities resulting from venous hypertension. "Chronic venous insufficiency" refers to the more severe forms of chronic venous disease Chronic venous disease Chronic venous disease is a spectrum of disorders characterized by venous dilation and/or abnormal vein function in the lower extremities resulting from venous hypertension. Skin changes typically distinguish chronic venous insufficiency from milder forms of venous disease (like varicose veins) and include skin pigmentation, stasis dermatitis, lipodermatosclerosis, and eventually, the development of ulcers. Chronic Venous Insufficiency. Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions changes typically distinguish chronic venous insufficiency Chronic venous insufficiency Chronic venous disease is a spectrum of disorders characterized by venous dilation and/or abnormal vein function in the lower extremities resulting from venous hypertension. "Chronic venous insufficiency" refers to the more severe forms of chronic venous disease. Skin changes typically distinguish chronic venous insufficiency from milder forms of venous disease. Chronic Venous Insufficiency from milder forms of venous disease (like varicose veins Varicose veins Enlarged and tortuous veins. Chronic Venous Insufficiency) and include skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions pigmentation, stasis dermatitis Stasis dermatitis Chronic Venous Insufficiency, lipodermatosclerosis Lipodermatosclerosis Chronic Venous Insufficiency, and eventually, the development of ulcers. Diagnosis is usually based on physical exam findings alone, although venous duplex ultrasonography Duplex ultrasonography Ultrasonography applying the doppler effect combined with real-time imaging. The real-time image is created by rapid movement of the ultrasound beam. A powerful advantage of this technique is the ability to estimate the velocity of flow from the doppler shift frequency. Hypercoagulable States can provide additional information about the etiology, location, and extent of disease. The mainstay of management is compression Compression Blunt Chest Trauma therapy. A variety of surgical options also exist for symptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, including ablation, sclerotherapy Sclerotherapy Treatment of varicose veins, hemorrhoids, gastric and esophageal varices, and peptic ulcer hemorrhage by injection or infusion of chemical agents which cause localized thrombosis and eventual fibrosis and obliteration of the vessels. Hemorrhoids, and valve repair. Venous ulcers are common as the disease progresses and are often very difficult to treat.
Last updated: Mar 4, 2024
Chronic venous disease Chronic venous disease Chronic venous disease is a spectrum of disorders characterized by venous dilation and/or abnormal vein function in the lower extremities resulting from venous hypertension. Skin changes typically distinguish chronic venous insufficiency from milder forms of venous disease (like varicose veins) and include skin pigmentation, stasis dermatitis, lipodermatosclerosis, and eventually, the development of ulcers. Chronic Venous Insufficiency is a spectrum of disorders characterized by venous dilation and/or abnormal vein function in the lower extremities resulting from venous hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension.
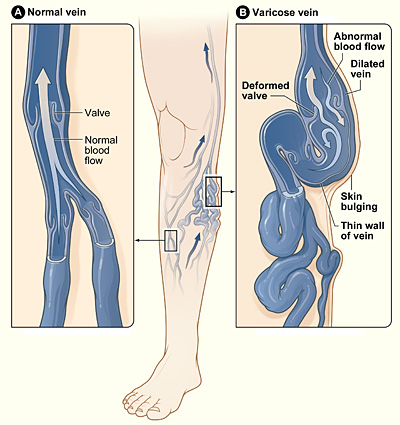
Varicose veins
Image: “Varicose veins” by National Heart Lung and Blood Institute. License: CC0 1.0
Irregular, nonhealing venous stasis ulcer on the lower leg and ankle, with unhealthy granulation tissue:
There is also surrounding lipodermatosclerosis, stasis dermatitis, and brown skin pigmentation, all characteristic of chronic venous insufficiency.

Stasis dermatitis
Image: “Stasis dermatitis” by Cardiologist61. License: Public DomainLower extremity appearance:
Venous refilling time Venous refilling time Chronic Venous Insufficiency (photoplethysmography (PPG)):[15]
Ankle–brachial index:
Other: heart, lung, and abdominal exams:
Duplex ultrasonography Duplex ultrasonography Ultrasonography applying the doppler effect combined with real-time imaging. The real-time image is created by rapid movement of the ultrasound beam. A powerful advantage of this technique is the ability to estimate the velocity of flow from the doppler shift frequency. Hypercoagulable States:[5,8,10,12]
Cross-sectional venography Venography Budd-Chiari Syndrome with CT or MRI:[5,10]
Catheter-based (invasive) venography Venography Budd-Chiari Syndrome:
Testing on venous leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy ulcers[8]
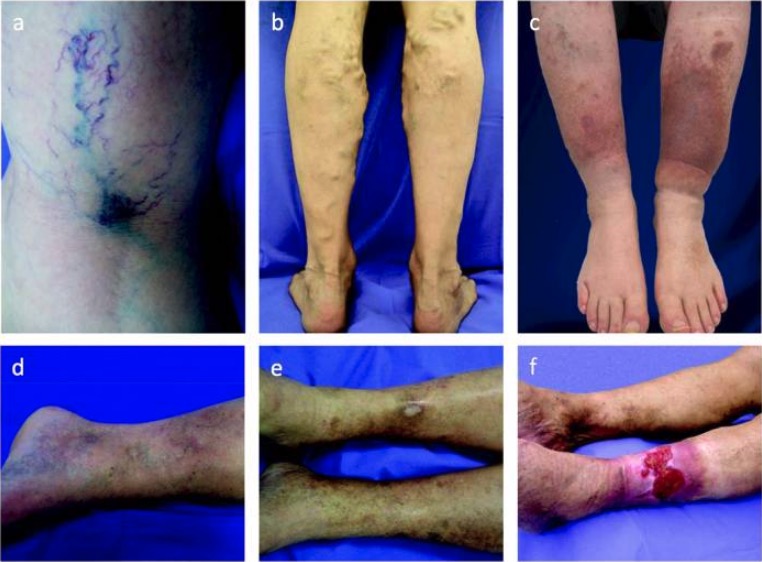
Spectrum of chronic venous disease:
Extent of disease can be classified from C1 to C6 on the basis of the following manifestations:
a: spider and reticular veins (C1)
b: varicose veins (C2)
c: edema and skin pigmentation (C4)
d: lipodermatosclerosis (C4)
e: healed ulcer (C5)
f: active venous ulcer (C6)
Venous clinical severity score[10,16]
| Clinical feature | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | None | Occasional, not restricting regular Regular Insulin daily activities | Daily, interfering with, but not preventing, regular Regular Insulin daily activities | Daily pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways that limits most regular Regular Insulin daily activities |
| Varicose veins Varicose veins Enlarged and tortuous veins. Chronic Venous Insufficiency ( ≥ 3 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma in diameter when standing) | None | Few, scattered | Multiple, confined to calf or thigh Thigh The thigh is the region of the lower limb found between the hip and the knee joint. There is a single bone in the thigh called the femur, which is surrounded by large muscles grouped into 3 fascial compartments. Thigh: Anatomy | Extensive, involving calf and thigh Thigh The thigh is the region of the lower limb found between the hip and the knee joint. There is a single bone in the thigh called the femur, which is surrounded by large muscles grouped into 3 fascial compartments. Thigh: Anatomy |
| Edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema | None | Limited to foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy and ankle | Above the ankle but below the knee | Extends to knee and above |
| Hyperpigmentation Hyperpigmentation Excessive pigmentation of the skin, usually as a result of increased epidermal or dermal melanin pigmentation, hypermelanosis. Hyperpigmentation can be localized or generalized. The condition may arise from exposure to light, chemicals or other substances, or from a primary metabolic imbalance. Malassezia Fungi | None | Limited to perimalleolar area | Diffuse, over lower ⅓ of leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy | Widespread, above lower ⅓ of leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy |
| Inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation and cellulitis Cellulitis Cellulitis is a common infection caused by bacteria that affects the dermis and subcutaneous tissue of the skin. It is frequently caused by Staphylococcus aureus and Streptococcus pyogenes. The skin infection presents as an erythematous and edematous area with warmth and tenderness. Cellulitis | None | Limited to perimalleolar area | Diffuse, over lower ⅓ of leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy | Widespread, above lower ⅓ of leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy |
| Induration Induration Dermatologic Examination | None | Limited to perimalleolar area | Diffuse, over lower ⅓ of leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy | Widespread, above lower ⅓ of leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy |
| Active ulcers | None | 1 | 2 | ≥ 3 |
| Ulcer duration | None | 3 months | 3‒12 months | > 12 months |
| Ulcer diameter | None | < 2 cm | 2‒6 cm | > 6 cm |
| Stocking use | None | Intermittent use | Most days | Constant use |
Management may vary based on practice location. The following information is based on US and European guidelines.
Goals:
Indications:[9]
Options include:[10]
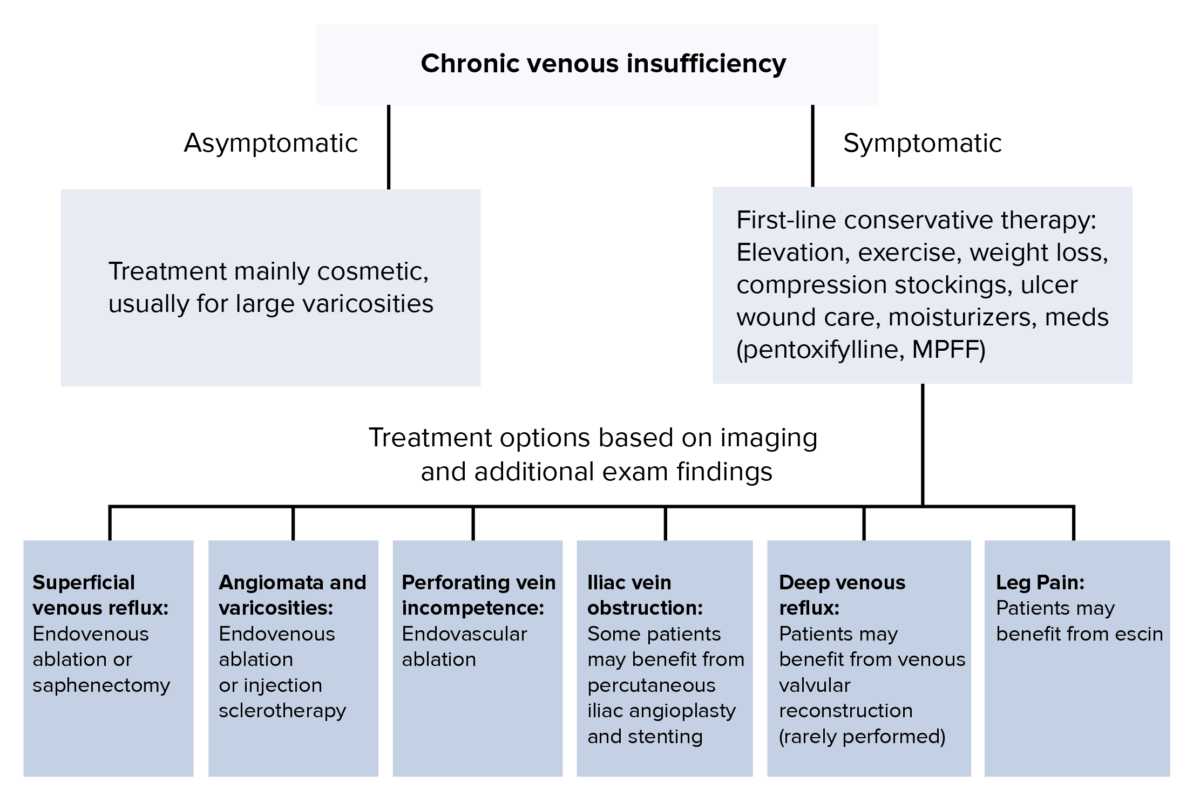
Algorithmic approach to chronic venous insufficiency treatment: If the patient is asymptomatic, treatment is primarily cosmetic for large varicosities. If the patient is asymptomatic, first line conservative therapy includes elevation, exercise, weight loss, compression stockings, ulcer wound are, moisturizers, and potentially medications such as pentoxifylline or micronized purified flavonoid fraction (MPFF). Based on other specific imaging or exam findings, additional treatments are recommended.
MPFF: micronized purified flavonoid fraction