Acute lymphoblastic leukemia/ lymphoma Lymphoma A general term for various neoplastic diseases of the lymphoid tissue. Imaging of the Mediastinum (ALL/LBL) are hematologic malignancies characterized by the uncontrolled proliferation of lymphoid precursor cells. Acute lymphoblastic leukemia/ lymphoma Lymphoma A general term for various neoplastic diseases of the lymphoid tissue. Imaging of the Mediastinum, the most common forms of cancer affecting children, show the presence of increased lymphoblasts Lymphoblasts Lymphocytosis. In ALL/LBL, lymphoblasts Lymphoblasts Lymphocytosis replace the normal marrow, eventually entering the circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment and infiltrating other organs. The clinical presentation includes fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia, bleeding, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, and infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, all of which are related to anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types, thrombocytopenia Thrombocytopenia Thrombocytopenia occurs when the platelet count is < 150,000 per microliter. The normal range for platelets is usually 150,000-450,000/µL of whole blood. Thrombocytopenia can be a result of decreased production, increased destruction, or splenic sequestration of platelets. Patients are often asymptomatic until platelet counts are < 50,000/µL. Thrombocytopenia, and the lack of functional WBCs. The onset of symptoms takes days to weeks. Mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast effects of malignant infiltration (in bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types, liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy) are common; thus, hepatosplenomegaly Hepatosplenomegaly Cytomegalovirus and lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy are seen. Diagnosis is by peripheral blood smear Peripheral Blood Smear Anemia: Overview and Types examination and bone marrow Bone marrow The soft tissue filling the cavities of bones. Bone marrow exists in two types, yellow and red. Yellow marrow is found in the large cavities of large bones and consists mostly of fat cells and a few primitive blood cells. Red marrow is a hematopoietic tissue and is the site of production of erythrocytes and granular leukocytes. Bone marrow is made up of a framework of connective tissue containing branching fibers with the frame being filled with marrow cells. Bone Marrow: Composition and Hematopoiesis biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma, which show the presence of lymphoblasts Lymphoblasts Lymphocytosis. Immunophenotyping Immunophenotyping Process of classifying cells of the immune system based on structural and functional differences. The process is commonly used to analyze and sort T-lymphocytes into subsets based on CD antigens by the technique of flow cytometry. Non-Hodgkin Lymphomas, histochemistry, and genetic studies aid in the classification and guidance of treatment. Management is mainly by chemotherapy Chemotherapy Osteosarcoma, which is administered in phases (induction, consolidation Consolidation Pulmonary Function Tests, and maintenance). Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas varies according to the age of onset and type of leukemia. The cure rate in children is 85%.
Last updated: Jun 4, 2025
Acute lymphoblastic leukemia/
lymphoma
Lymphoma
A general term for various neoplastic diseases of the lymphoid tissue.
Imaging of the Mediastinum (ALL/LBL) are hematologic malignancies characterized by the pathological proliferation of lymphoid precursor cells (primarily the B and T cell lineages)
in the
bone marrow
Bone marrow
The soft tissue filling the cavities of bones. Bone marrow exists in two types, yellow and red. Yellow marrow is found in the large cavities of large bones and consists mostly of fat cells and a few primitive blood cells. Red marrow is a hematopoietic tissue and is the site of production of erythrocytes and granular leukocytes. Bone marrow is made up of a framework of connective tissue containing branching fibers with the frame being filled with marrow cells.
Bone Marrow: Composition and Hematopoiesis, with subsequent
displacement
Displacement
The process by which an emotional or behavioral response that is appropriate for one situation appears in another situation for which it is inappropriate.
Defense Mechanisms of other blood cell precursors.
WHO system 2016 (supersedes the French-American-British classification):
Hematopoiesis Hematopoiesis The development and formation of various types of blood cells. Hematopoiesis can take place in the bone marrow (medullary) or outside the bone marrow (extramedullary hematopoiesis). Bone Marrow: Composition and Hematopoiesis starts with a hematopoietic stem cell, which is prompted to divide and differentiate with appropriate chemical stimuli (hemopoietic growth factors).
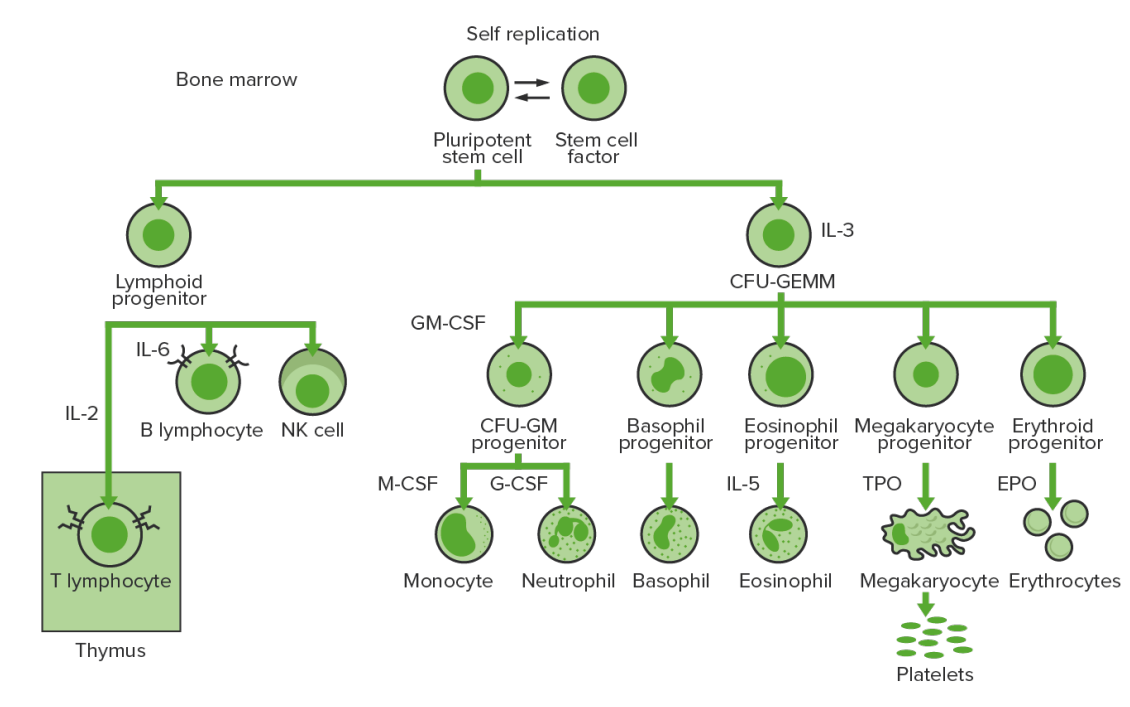
Bone marrow hematopoiesis:
Proliferation and differentiation of the formed elements of blood:
In CML, there is sustained proliferation of cells in the granulocytic line (myeloblasts → neutrophils, basophils, eosinophils). Both mature and maturing cells are seen; thus, there are cells that are only partially effective.
CFU-GEMM: colony-forming unit–granulocyte, erythrocyte, monocyte, megakaryocyte
CFU-GM: colony-forming unit–granulocyte macrophage
GM-CSF: granulocyte macrophage colony-stimulating factor
M-CSF: macrophage colony-stimulating factor
G-CSF: granulocyte colony-stimulating factor
NK: natural killer
TPO: thrombopoietin
| Features | Acute lymphoblastic leukemia | Acute myeloid leukemia Acute Myeloid Leukemia Acute myeloid leukemia (AML) is a hematologic malignancy characterized by the uncontrolled proliferation of myeloid precursor cells. Seen predominantly in older adults, AML includes an accumulation of myeloblasts and a replacement of normal marrow by malignant cells, which leads to impaired hematopoiesis. Acute Myeloid Leukemia |
|---|---|---|
| Population | More common in children | More common in adults |
| Common characteristics |
|
|
| Clinical findings |
|
|
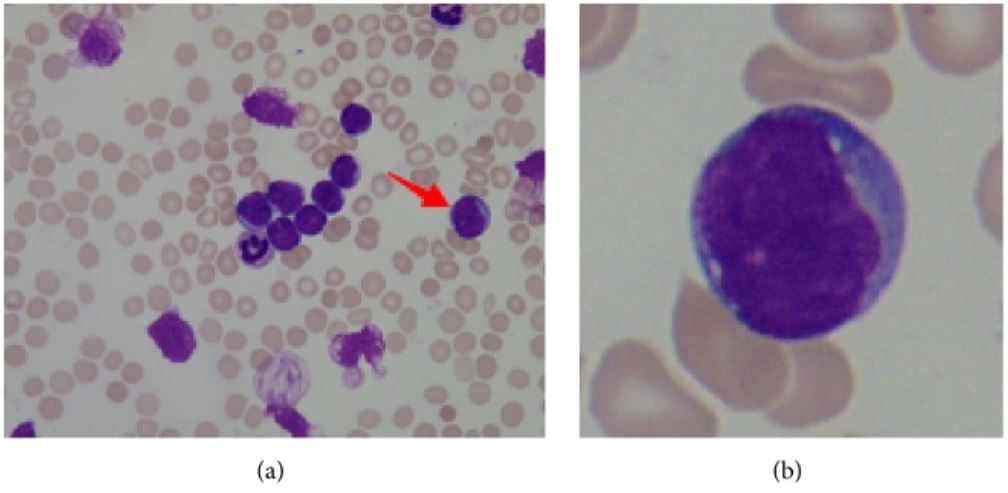
a: bone marrow smear from a patient with acute lymphoblastic leukemia (ALL), arrow pointing to lymphoblast
b: lymphoblast: large nucleus, scant cytoplasm
| Features | Acute lymphoblastic leukemia | Acute myeloid leukemia Acute Myeloid Leukemia Acute myeloid leukemia (AML) is a hematologic malignancy characterized by the uncontrolled proliferation of myeloid precursor cells. Seen predominantly in older adults, AML includes an accumulation of myeloblasts and a replacement of normal marrow by malignant cells, which leads to impaired hematopoiesis. Acute Myeloid Leukemia |
|---|---|---|
| Laboratory findings | Anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types, thrombocytopenia Thrombocytopenia Thrombocytopenia occurs when the platelet count is < 150,000 per microliter. The normal range for platelets is usually 150,000-450,000/µL of whole blood. Thrombocytopenia can be a result of decreased production, increased destruction, or splenic sequestration of platelets. Patients are often asymptomatic until platelet counts are < 50,000/µL. Thrombocytopenia, varying WBCs | |
| Peripheral smear or bone marrow Bone marrow The soft tissue filling the cavities of bones. Bone marrow exists in two types, yellow and red. Yellow marrow is found in the large cavities of large bones and consists mostly of fat cells and a few primitive blood cells. Red marrow is a hematopoietic tissue and is the site of production of erythrocytes and granular leukocytes. Bone marrow is made up of a framework of connective tissue containing branching fibers with the frame being filled with marrow cells. Bone Marrow: Composition and Hematopoiesis examination (morphology) |
Lymphoblasts
Lymphoblasts
Lymphocytosis:
|
Myeloblasts:
|
| Cytochemistry |
|
|
| Immunophenotyping Immunophenotyping Process of classifying cells of the immune system based on structural and functional differences. The process is commonly used to analyze and sort T-lymphocytes into subsets based on CD antigens by the technique of flow cytometry. Non-Hodgkin Lymphomas |
|
CD13, CD33, CD117, HLA-DR |
Chemotherapy Chemotherapy Osteosarcoma, which can span 2–3 years, is highly effective in young patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.
| Management | Acute lymphoblastic leukemia | Acute myeloid leukemia Acute Myeloid Leukemia Acute myeloid leukemia (AML) is a hematologic malignancy characterized by the uncontrolled proliferation of myeloid precursor cells. Seen predominantly in older adults, AML includes an accumulation of myeloblasts and a replacement of normal marrow by malignant cells, which leads to impaired hematopoiesis. Acute Myeloid Leukemia |
|---|---|---|
| Induction |
|
|
| Consolidation Consolidation Pulmonary Function Tests | Options:
|
Additional chemotherapy Chemotherapy Osteosarcoma ( cytarabine Cytarabine A pyrimidine nucleoside analog that is used mainly in the treatment of leukemia, especially acute non-lymphoblastic leukemia. Cytarabine is an antimetabolite antineoplastic agent that inhibits the synthesis of DNA. Its actions are specific for the s phase of the cell cycle. It also has antiviral and immunosuppressant properties. Antimetabolite Chemotherapy) |
| Maintenance |
|
Nonmyelosuppressive chemotherapy Chemotherapy Osteosarcoma and/or targeted agent |
| Additional treatment |
|
Acute promyelocytic leukemia
Acute promyelocytic leukemia
An acute myeloid leukemia in which abnormal promyelocytes predominate. It is frequently associated with disseminated intravascular coagulation.
Acute Myeloid Leukemia:
|
| Hematopoietic cell transplantation | For patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with poor prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas | |
| Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas |
|
|