Actinomyces is an anaerobic, gram-positive, branching, filamentous rod. Actinomyces israelii is the most common species involved in human disease. The organism is commonly found as part of the normal flora in the oral cavity, gastrointestinal tract, and reproductive tract. The disease is caused when the organism is displaced even by minor trauma or procedure, allowing the organism to move beyond the mucosal barrier. Reaching areas of low oxygen leads to the organism's multiplication. Actinomyces is associated with cervicofacial infection, which forms draining sinus tracts. Actinomyces can also affect the thoracic, abdominal, and pelvic areas. Drainage or infected tissue may have the characteristic yellow sulfur granules associated with Actinomyces. Management is with long-term penicillin and surgery, if needed.
Last updated: May 26, 2025
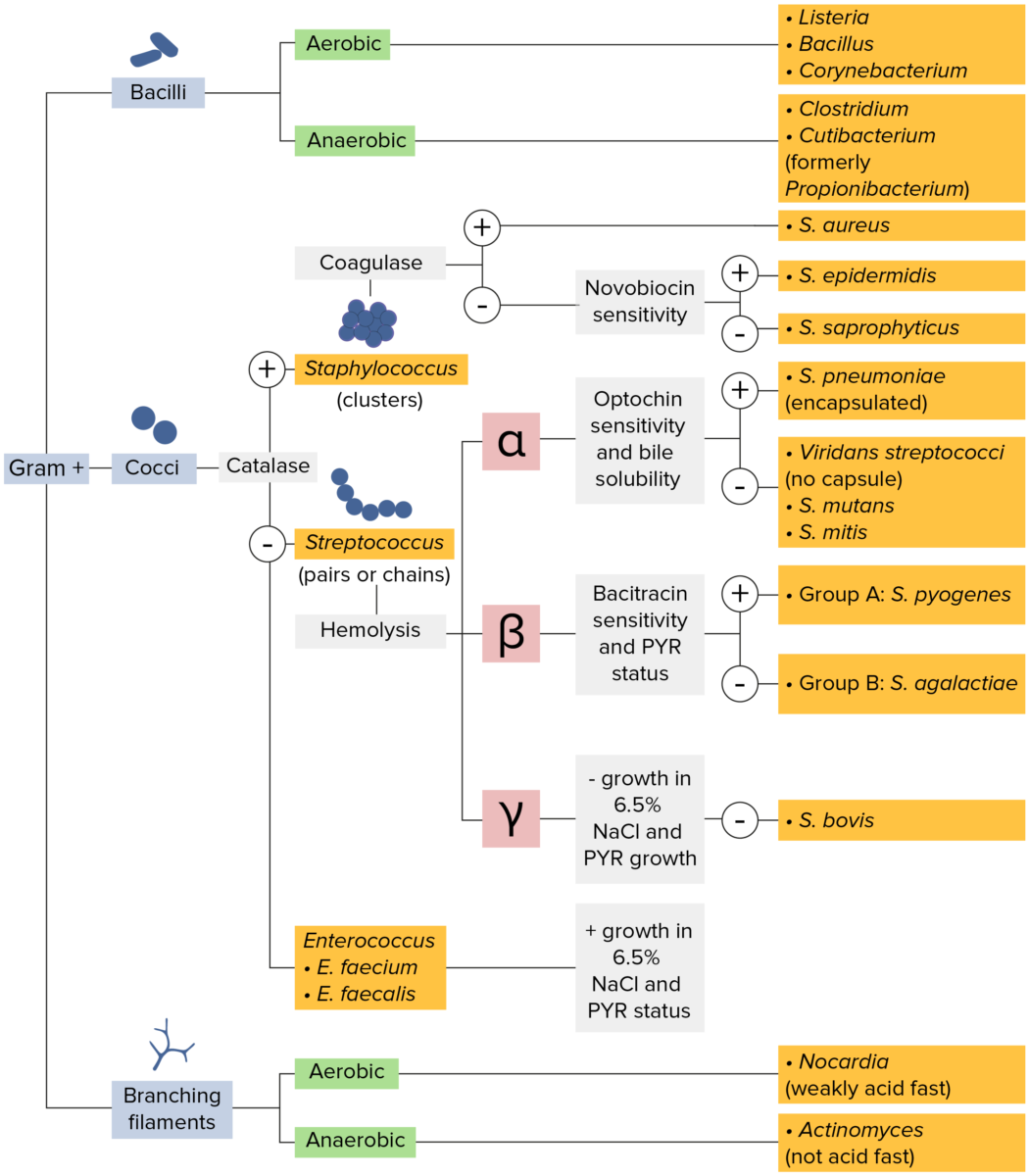
Gram-positive bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thick layer of peptidoglycan retain the crystal violet stain utilized in Gram staining but are not affected by the safranin counterstain. These bacteria appear as purple-blue on the stain, indicating that they are gram positive. The bacteria can be further classified according to morphology (branching filaments, bacilli, and cocci in clusters or chains) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The cocci can also be further identified. Staphylococci can be narrowed down on the basis of the presence of the enzyme coagulase and on their sensitivity to the antibiotic novobiocin. Streptococci are grown on blood agar and classified on the basis of which form of hemolysis they employ (α, β, or γ). Streptococci are further narrowed on the basis of their response to the pyrrolidonyl-β-naphthylamide (PYR) test, their sensitivity to specific antimicrobials (optochin and bacitracin), and their ability to grow on sodium chloride (NaCl) media.
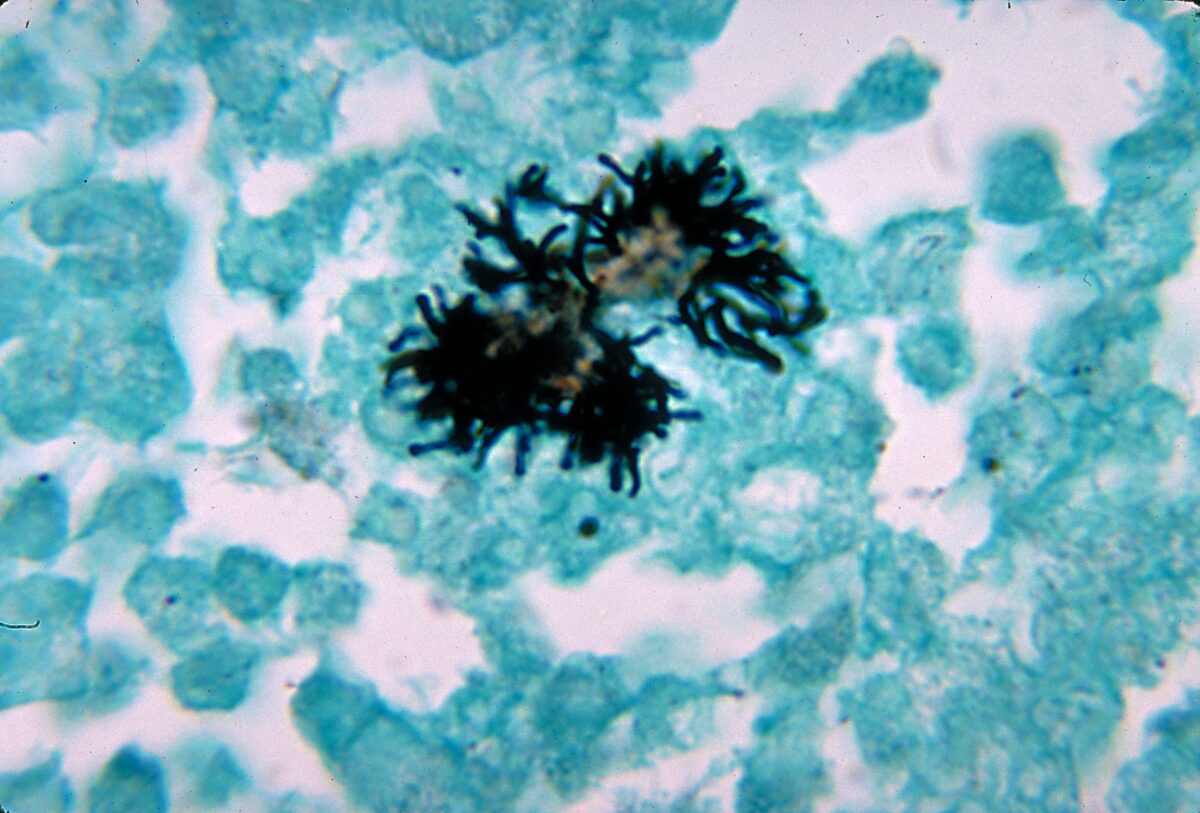
Histopathological changes of brain abscess due to A. naeslundii bacteria (in silver stain). Branching bacilli are noted.
Image: “Actinomyces naeslundii 01” by CDC/Dr. Lucille Georg. License: Public DomainReservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli:
Transmission:
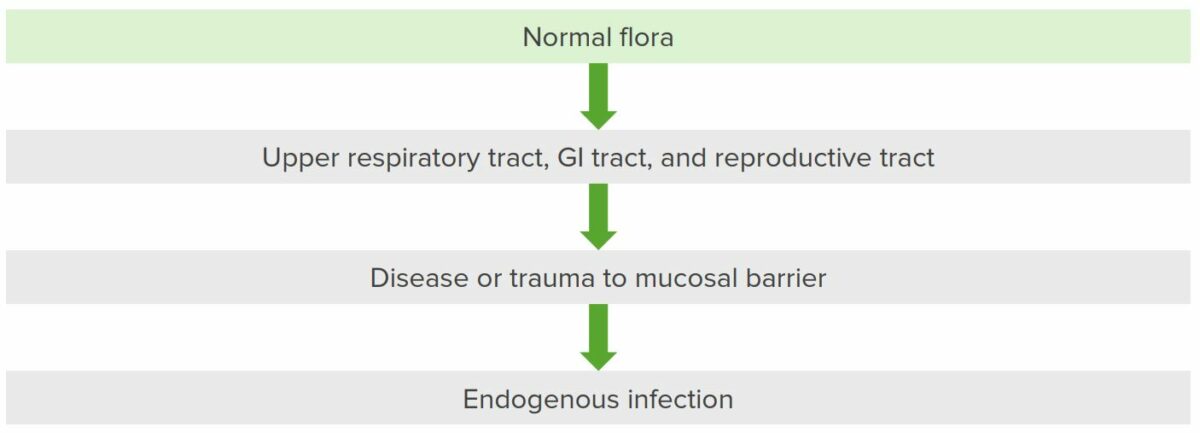
Pathogenesis of Actinomyces
When there is a breakdown of the mucosal barrier, Actinomyces from the oropharynx (which goes to respiratory areas), GI tract, and reproductive tract cause infection and spread to contiguous tissues while creating sinus tracts.

A patient with actinomycosis on the right side of the face (in front of ear)
Image: “Actinomycosis PHIL 2856 lores” by CDC/Dr. Thomas F. Sellers. License: Public Domain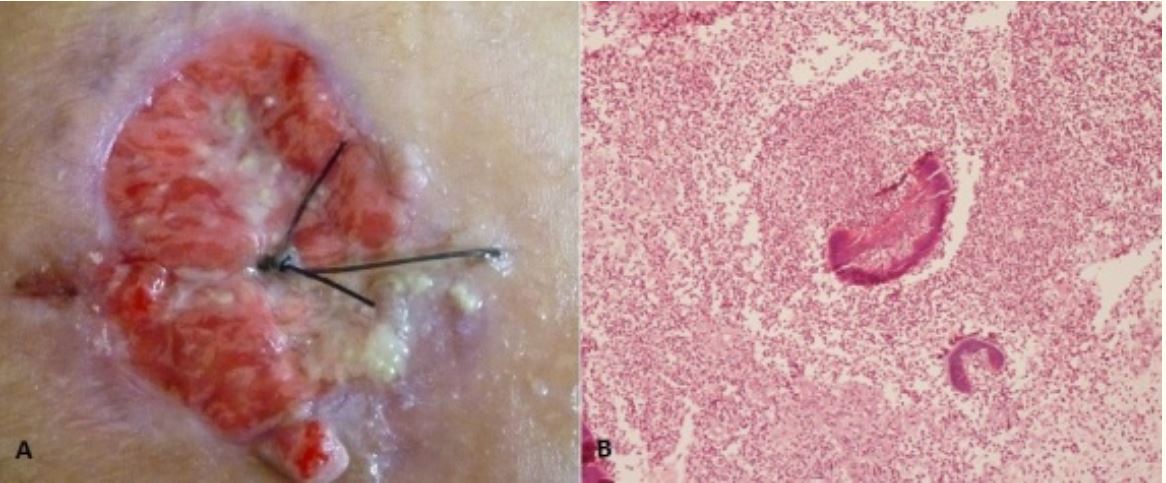
Actinomycosis of the chest wall: A: Ulcerated and burgeoning lesion in the right parasternal region, with pus mixed with sulfur granules. B: Inflammatory cells surround the basophilic sulfur granules (composed of filaments arranged in a radiating pattern).
Image: “Unusual actinomycosis of the chest wall” by Bouaddi M, Hassam B. License: CC BY 2.0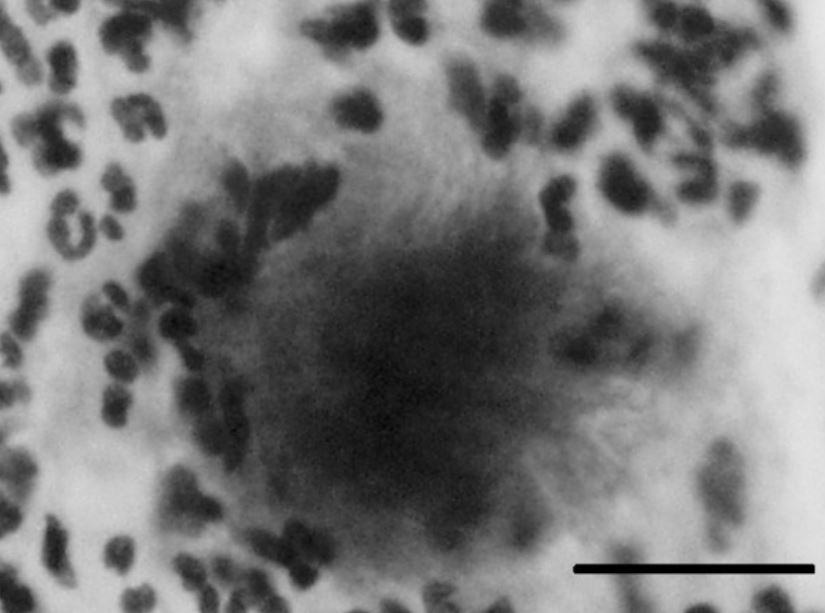
Pelvic actinomycosis due to IUD.
A typical bacterial aggregate from a cervical Papanicolaou (Pap) smear showing a cotton ball–like colony with protruding mycelial filaments, suggesting Actinomyces species infection. The bar indicates 20 μm.
Osteonecrosis of the jaw associated with Actinomyces
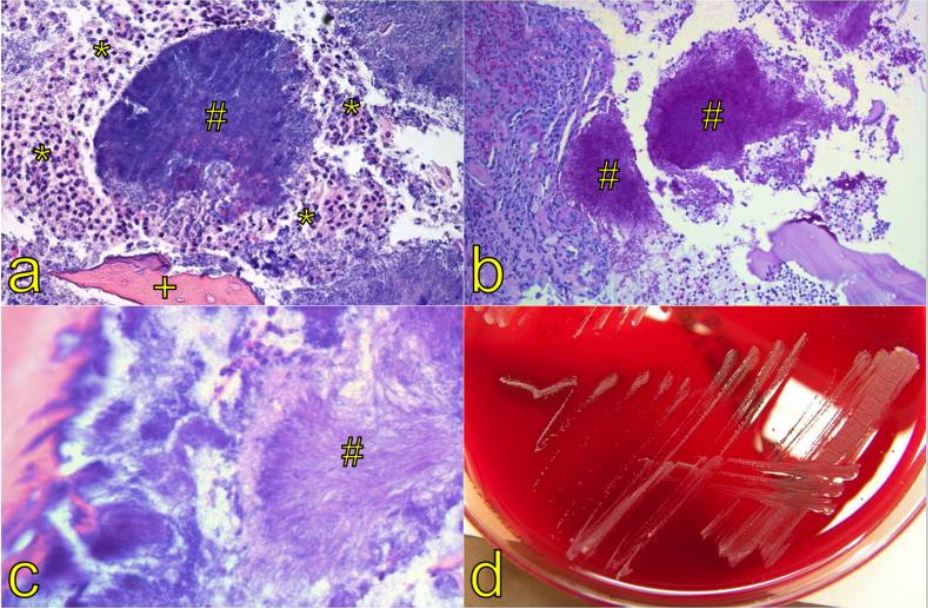
(a) Hematoxylin and eosin staining of an aggregate composed of filaments, so-called sulfur granules (#). These granules macroscopically appear as yellow granules surrounded by neutrophilic granulocytes (*) and a necrotic bone trabecula (+, magnification x 100).
(b) The granules (#) stain periodic-acid Schiff (PAS)–positive (magnification x 200).
(c) High magnification elucidates the filamentous structure (#, sun-ray morphology) of the organisms (magnification x 400).
(d) Typical growth pattern of Actinomyces spp. in microbiological culture.
Two clinically relevant gram-positive Gram-Positive Penicillins, branching, filamentous rods Filamentous rods Nocardia/Nocardiosis that must be distinguished:
| Differentiating factors | Actinomyces | Nocardia Nocardia Nocardia is a branching, filamentous, gram-positive bacilli. It is partially acid fast due to the presence of mycolic acids in the cell wall. Nocardia is a ubiquitous soil organism that most commonly affects immunocompromised patients. Nocardia is transmitted via inhalation of aerosolized bacteria or less commonly, via direct contact with wounds. Nocardia/Nocardiosis |
|---|---|---|
| Oxygen requirement | Anaerobic | Aerobic |
| Acid-fast stain Acid-Fast Stain Meningitis in Children | Not acid-fast | Acid-fast (partially) |
| Reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli/habitat | Normal oral, GI, and reproductive flora | Found in soil, water, decaying organic matter |
| Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease caused |
|
|
| Management | Penicillin Penicillin Rheumatic Fever | Trimethoprim-sulfamethoxazole |
Mnemonic:
SNAP (Sulfonamides-Nocardia, Actinomyces–Penicillin)