Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto's disease (autoimmune thyroiditis) is the leading cause in non–iodine-deficient regions. Primary hypothyroidism occurs with thyroid gland disorders, while the central type arises from pituitary and hypothalamic conditions. Thyroid hormones are integral in metabolic processes and in the development of the brain and other organs. Congenital hypothyroidism can result in significant mental disability due to the loss of thyroid hormones. The features of acquired hypothyroidism also reflect the effects of slowed organ function, such as fatigue, bradycardia, cold intolerance, and exertional dyspnea. Diagnosis is by thyroid function testing. Elevated thyroid stimulating hormone and low free thyroxine (T4) levels are noted. Treatment is with synthetic T4.
Last updated: Mar 4, 2024
Hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto’s disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism is an endocrine disorder resulting from thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormone deficiency.
By onset:
By organs affected with disease:
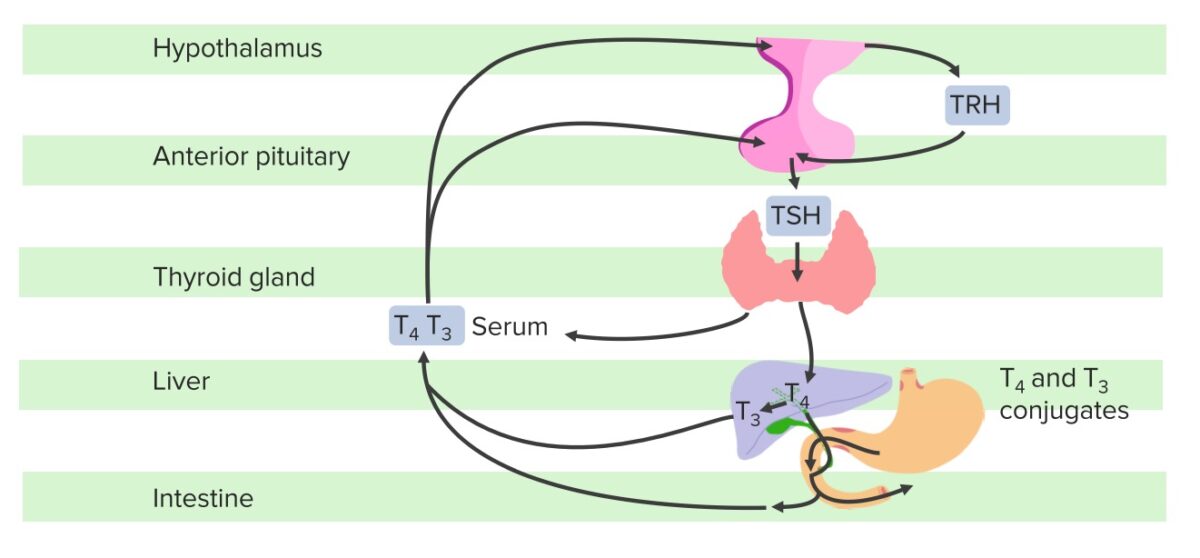
Schematic diagram of the hypothalamic–pituitary–thyroid axis:
The hypothalamus produces TRH, which stimulates the pituitary gland to synthesize and secrete TSH, which then stimulates the synthesis and secretion of T3 and T4 by the thyroid gland. T4 is converted to T3 in the liver and other tissues. A fraction of T4 and T3 is conjugated with glucuronide and sulfate in the liver, excreted in the bile, and partially hydrolyzed in the intestine; some of this fraction in the intestine may be reabsorbed. If the hypothalamus senses low FT3 and FT4, there will be an increase in TRH and subsequently, TSH; conversely, in this negative feedback loop, T3 and T4 inhibit the release of TSH from the hypothalamus and the pituitary once normal levels are achieved.
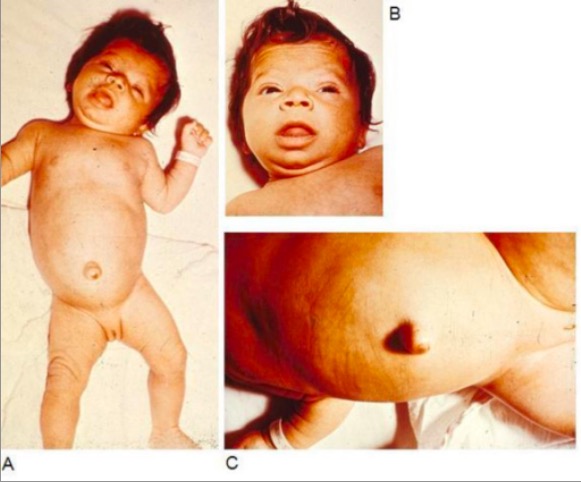
Infant with congenital hypothyroidism displaying typical signs and symptoms, such as hypotonia (A), myxedematous facies and macroglossia (B), and an umbilical hernia (C)
Image: “Infant with congenital hypothyroidism” by Department of Pediatrics, Division of Endocrinology, Oregon Health & Science University, 707 SW Gaines Street, Portland, OR, USA. License: CC BY 2.0Common signs and symptoms:[8,9]
In the elderly:
Myxedema coma Myxedema Coma Hypothyroidism:
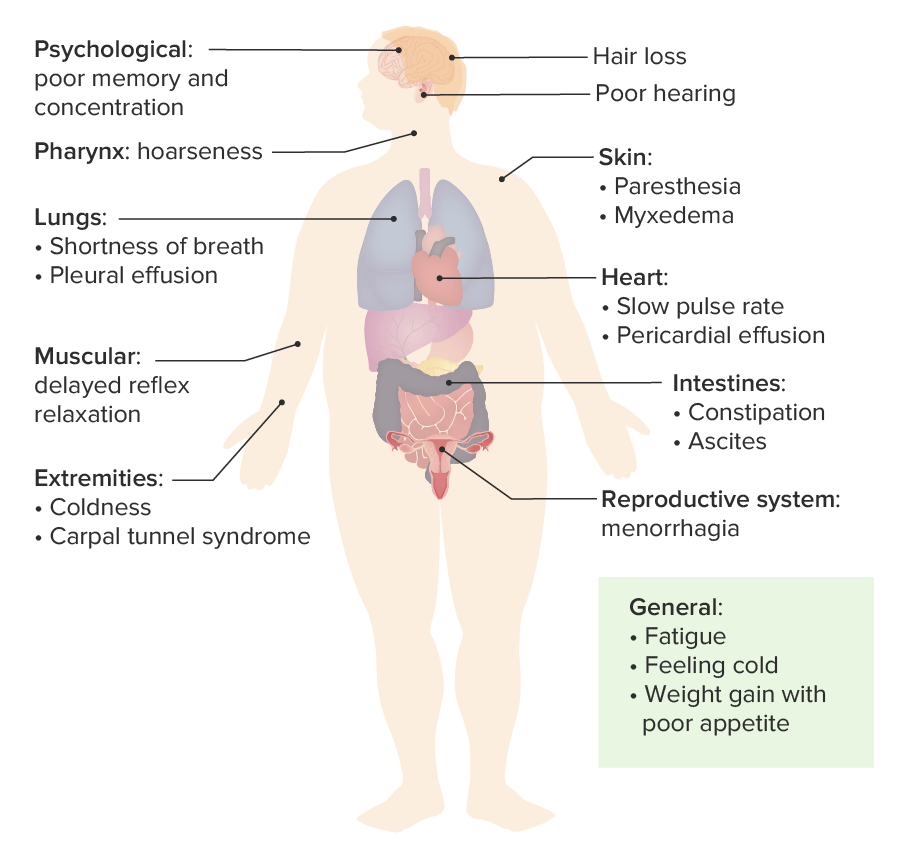
Diagram of the most common signs and symptoms of hypothyroidism
Image by Lecturio.Mandatory screening Screening Preoperative Care in all newborns ( newborn Newborn An infant during the first 28 days after birth. Physical Examination of the Newborn screening Screening Preoperative Care (NBS)):[10,11]
Imaging:[10,11]
Early diagnosis and treatment can prevent long-term mental disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman’s compensation benefits. ABCDE Assessment.
Thyroid function tests Thyroid Function Tests Blood tests used to evaluate the functioning of the thyroid gland. Ion Channel Myopathy:
Antibody testing:
Imaging studies:
Additional workup:
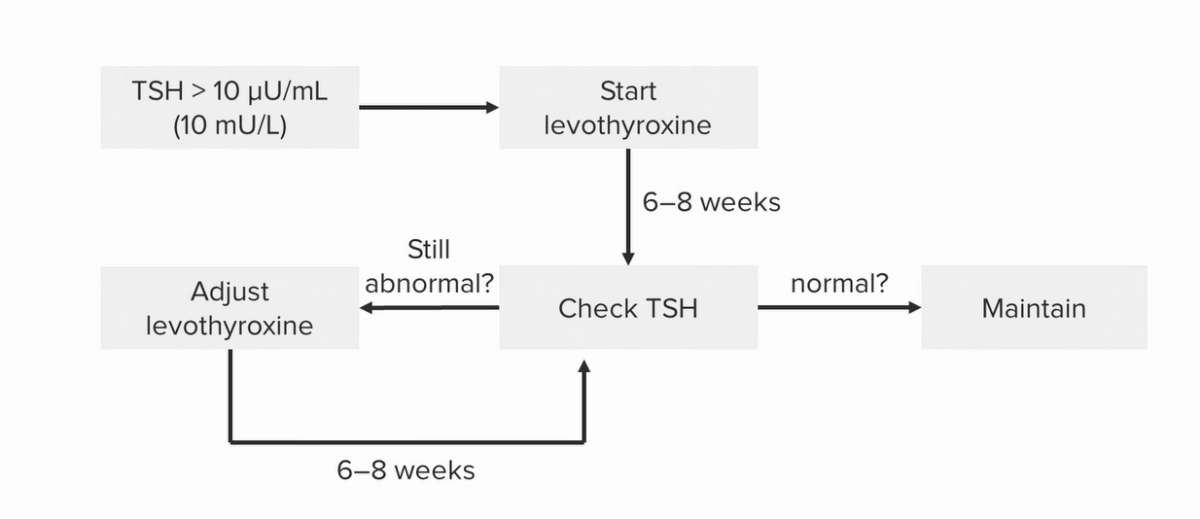
Schematic diagram of the management of Hashimoto’s thyroiditis:
Note that the adjustments depend on TSH levels.
| Organization | Recommendation |
|---|---|
| American Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy Association | TSH > 10 mIU/L: Consider treatment. |
| TSH ≤ 10 mIU/L: Consider treatment if symptoms of hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto’s disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism, if TPO antibody–positive, or if there are risk factors/evidence of atherosclerotic cardiovascular disease, or heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR). | |
| European Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy Association | Age < 65 years:
|
| Age ≥ 65 years:
|
|
| National Institute for Health and Care Excellence |
|

A man with myxedema due to hypothyroidism:
Note the expressionless face, periorbital puffiness, pallor, peripheral edema, and massive ascites. Because it is curable, myxedema should be considered in every patient with conspicuous ascites, except perhaps those with widespread or terminal malignancy. The patient shown received thyroid replacement therapy, and all of his physical abnormalities resolved. If ascites persists after treatment, a coexisting cause should be sought.