Ventricular tachycardia is any heart rhythm faster than 100/min, with 3 or more irregular beats in a row, arising distal to the bundle of His. Ventricular tachycardia is the most common form of wide-complex tachycardia, and it is associated with a high mortality rate. Ventricular tachycardia is often caused by myocardial ischemia, structural disease, congenital conditions, or electrolyte derangement. Individuals may present with chest pain, dyspnea, palpitations, syncope, and hemodynamic instability. Diagnosis is based on characteristic ECG findings of wide-complex QRS, fusion, and capture beats. Management may require antiarrhythmic medications or electrical cardioversion to avoid complications such as heart failure, multiorgan failure, and cardiac arrest.
Last updated: Mar 4, 2024
Diagnosis is by ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) or cardiac monitoring.[6–8]
There are 2 primary types of ventricular tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children:[6–8]
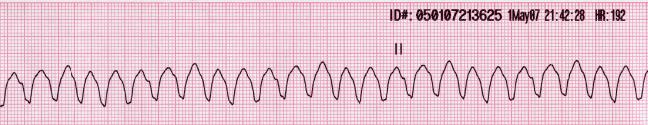
Rhythm strip of ventricular tachycardia showing a regular, wide complex rhythm with a rate over 100/min
This is a shockable rhythm.

Example of an ECG tracing showing beat-to-beat axis deviation of the QRS complexes around the baseline in torsades de pointes
Image: “Torsade de pointes” by Panthro. License: CC0 1.0The following recommendations are based on the most recent US and UK advanced life support guidelines.
Management of ventricular tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children is based on whether a pulse is present and, if it is, whether the individual is hemodynamically stable.

Ventricular fibrillation/pulseless ventricular tachycardia management algorithm
Image by Lecturio.Follow the adult cardiac arrest Cardiac arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest algorithm.[6–8]
Identify reversible causes:
| 5 Hs HS Hypertrophic scars and keloids are raised, red, and rigid (3 rs) scars that develop during cutaneous wound healing and are characterized by a local abnormal proliferation of fibroblasts with over-production of collagen. Over-expression of growth factors and decreased production of molecules that promote matrix breakdown appear to be involved in the etiology. Hypertrophic and Keloid Scars | 5 Ts |
|---|---|
| Hypovolemia | Tension pneumothorax Pneumothorax A pneumothorax is a life-threatening condition in which air collects in the pleural space, causing partial or full collapse of the lung. A pneumothorax can be traumatic or spontaneous. Patients present with a sudden onset of sharp chest pain, dyspnea, and diminished breath sounds on exam. Pneumothorax |
| Hypoxia | Tamponade Tamponade Pericardial effusion, usually of rapid onset, exceeding ventricular filling pressures and causing collapse of the heart with a markedly reduced cardiac output. Pericarditis(cardiac) |
| Hydrogen ions ( acidosis Acidosis A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up. Respiratory Acidosis) | Toxins |
| Hypokalemia or hyperkalemia Hyperkalemia Hyperkalemia is defined as a serum potassium (K+) concentration >5.2 mEq/L. Homeostatic mechanisms maintain the serum K+ concentration between 3.5 and 5.2 mEq/L, despite marked variation in dietary intake. Hyperkalemia can be due to a variety of causes, which include transcellular shifts, tissue breakdown, inadequate renal excretion, and drugs. Hyperkalemia | Thrombosis, coronary |
| Hypothermia | Thrombosis, pulmonary |
Management after successful resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome:
| Drug | Dose | Notes |
|---|---|---|
| Adenosine Adenosine A nucleoside that is composed of adenine and d-ribose. Adenosine or adenosine derivatives play many important biological roles in addition to being components of DNA and RNA. Adenosine itself is a neurotransmitter. Class 5 Antiarrhythmic Drugs | Initial dose: 6 mg IV over 1–2 seconds followed by
normal saline
Normal saline
A crystalloid solution that contains 9. 0g of sodium chloride per liter of water. It has a variety of uses, including: as a contact lens solution, in ophthalmic solutions and nasal lavage, in wound irrigation, and for fluid therapy.
Intravenous Fluids flush 2nd dose 12 mg IV over 1–2 seconds followed by normal saline Normal saline A crystalloid solution that contains 9. 0g of sodium chloride per liter of water. It has a variety of uses, including: as a contact lens solution, in ophthalmic solutions and nasal lavage, in wound irrigation, and for fluid therapy. Intravenous Fluids flush |
May be used to distinguish monomorphic wide complex
tachycardia
Tachycardia
Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia.
Sepsis in Children from supraventricular
tachycardia
Tachycardia
Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia.
Sepsis in Children The 2nd dose can be given 1–2 minutes after the 1st |
| Drug | Dose | Notes |
|---|---|---|
| Procainamide Procainamide A class ia antiarrhythmic drug that is structurally-related to procaine. Class 1 Antiarrhythmic Drugs (Sodium Channel Blockers) | Initial infusion:20–50 mg/min IV Maintenance infusion1–4 mg/min IV |
Continue initial infusion until arrhythmia is terminated, QRS is increased by > 50%, or maximum dose of 17 mg/kg is reached. Avoid in prolonged–QT syndrome or congestive heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) |
| Amiodarone Amiodarone An antianginal and class III antiarrhythmic drug. It increases the duration of ventricular and atrial muscle action by inhibiting potassium channels and voltage-gated sodium channels. There is a resulting decrease in heart rate and in vascular resistance. Pulmonary Fibrosis | Initial:150 mg IV over 10 minutes Maintenance infusion 1 mg/min IV for next 6 hours |
Initial dose may be repeated if
VT
VT
Ventricular tachycardia is any heart rhythm faster than 100 beats/min, with 3 or more irregular beats in a row, arising distal to the bundle of his. Ventricular tachycardia is the most common form of wide-complex tachycardia, and it is associated with a high mortality rate.
Ventricular Tachycardia recurs. Preferred if left ventricular (LV) dysfunction present |
| Sotalol Sotalol An adrenergic beta-antagonist that is used in the treatment of life-threatening arrhythmias. Class 3 Antiarrhythmic Drugs (Potassium Channel Blockers) | Initial: 100 mg (1.5 mg/kg) over 5 minute | Avoid in prolonged QT Prolonged QT Class 3 Antiarrhythmic Drugs (Potassium Channel Blockers). |
| Lidocaine Lidocaine A local anesthetic and cardiac depressant used as an antiarrhythmic agent. Its actions are more intense and its effects more prolonged than those of procaine but its duration of action is shorter than that of bupivacaine or prilocaine. Local Anesthetics | Initial infusion: 1–1.5 mg/kg IV, may repeat with 0.5–0.75 mg/kg every 5–10 minutes as necessary Maintenance infusion: 1–4 mg/min IV |
Maximum dose: 3 mg/kg Consider when VT VT Ventricular tachycardia is any heart rhythm faster than 100 beats/min, with 3 or more irregular beats in a row, arising distal to the bundle of his. Ventricular tachycardia is the most common form of wide-complex tachycardia, and it is associated with a high mortality rate. Ventricular Tachycardia is associated with myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease or infarction. |
| Drug | Dose | Notes |
|---|---|---|
| Magnesium Magnesium A metallic element that has the atomic symbol mg, atomic number 12, and atomic weight 24. 31. It is important for the activity of many enzymes, especially those involved in oxidative phosphorylation. Electrolytes | 1–2 g IV over 15 minutes | Effect is transient; may be repeated, but avoid hypermagnesemia Hypermagnesemia Electrolytes. |
| Isoproterenol Isoproterenol Isopropyl analog of epinephrine; beta-sympathomimetic that acts on the heart, bronchi, skeletal muscle, alimentary tract, etc. It is used mainly as bronchodilator and heart stimulant. Sympathomimetic Drugs | 2–10 µg/min IV titrated to clinical response (adults) 0.05–0.1 µg/kg/min (children) |
For polymorphic VT VT Ventricular tachycardia is any heart rhythm faster than 100 beats/min, with 3 or more irregular beats in a row, arising distal to the bundle of his. Ventricular tachycardia is the most common form of wide-complex tachycardia, and it is associated with a high mortality rate. Ventricular Tachycardia triggered by bradycardia Bradycardia Bradyarrhythmia is a rhythm in which the heart rate is less than 60/min. Bradyarrhythmia can be physiologic, without symptoms or hemodynamic change. Pathologic bradyarrhythmia results in reduced cardiac output and hemodynamic instability causing syncope, dizziness, or dyspnea. Bradyarrhythmias |
Nonpharmacologic methods[6–9]
The following tests can be performed in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship presenting with suspicious symptoms (e.g., syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope) and/or nonsustained VT VT Ventricular tachycardia is any heart rhythm faster than 100 beats/min, with 3 or more irregular beats in a row, arising distal to the bundle of his. Ventricular tachycardia is the most common form of wide-complex tachycardia, and it is associated with a high mortality rate. Ventricular Tachycardia. These can detect arrhythmias, their frequency, and their relationship with symptoms.