Acute pancreatitis is an inflammatory disease of the pancreas due to autodigestion. Common etiologies include gallstones and excessive alcohol use. Patients typically present with epigastric pain radiating to the back. Diagnosis requires 2 of 3 criteria, including: characteristic abdominal pain, serum amylase and lipase 3 times the upper limit of normal, or characteristic radiology findings. Ranson criteria is commonly used to assess the severity. Management includes aggressive intravenous hydration, analgesia, nutritional support, and treatment of the underlying cause.
Last updated: Mar 4, 2024
Acute pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis is classified according to the Revised Atlanta Classification system, which describes:
| Type | Interstitial edematous pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis | Necrotizing pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis |
|---|---|---|
| CT findings | ||
| Fluid collection ≤ 4 weeks (no definable wall) | Acute peripancreatic fluid collection | Acute necrotic collection |
| Fluid collection > 4 weeks (well-defined wall) | Pancreatic pseudocyst Pancreatic pseudocyst Cyst-like space not lined by epithelium and contained within the pancreas. Pancreatic pseudocysts account for most of the cystic collections in the pancreas and are often associated with chronic pancreatitis. Acute Cholangitis | Walled-off necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage |
Acute pancreatitis
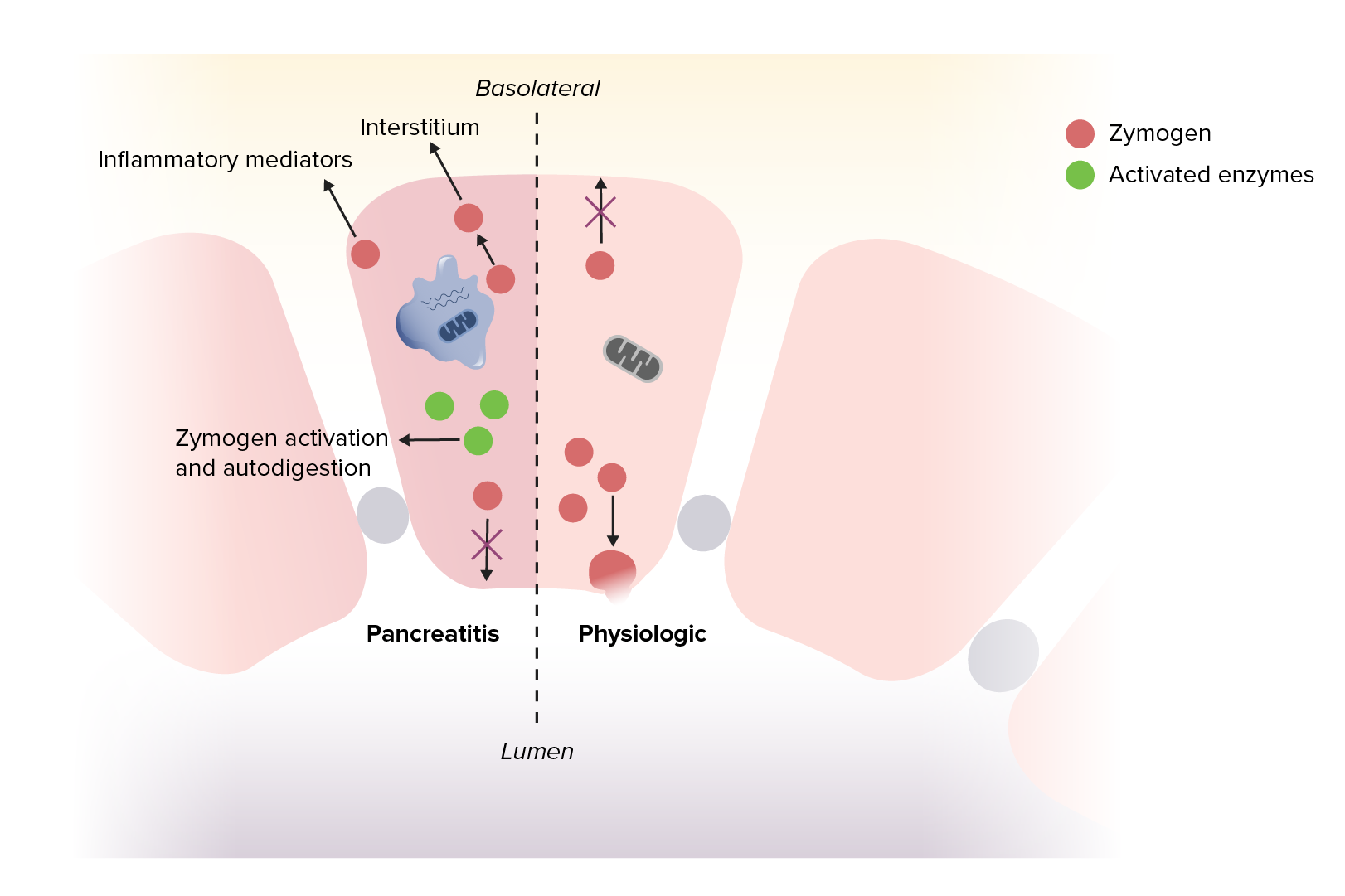
Image by Lecturio.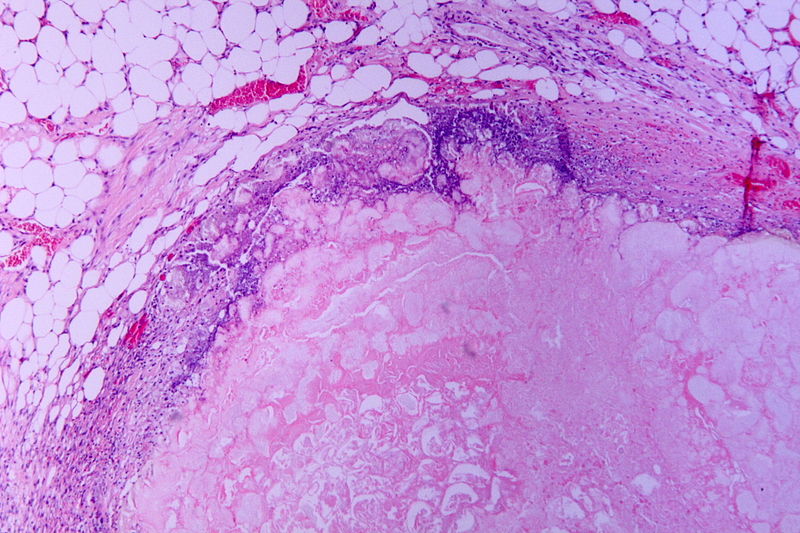
Hematoxylin and eosin (H&E) stain of necrotic pancreatitis (eosinophilic area without architecture: necrosis), surrounded by basophilic inflammatory cells and normal fat cells
Image: “Tryptic fat tissue necrosis in severe pancreatitis” by Patho. License: CC BY-SA 3.0.
Cullen’s sign, signaling blood in the peritoneum
Image: “Cullen’s sign” by Herbert L. Fred, MD. License: CC BY 2.0.
Grey-Turner’s sign due to hemorrhagic pancreatitis
Image: by Herbert L. Fred, MD and Hendrik A. van Dijk. License: CC BY 2.0.The diagnosis of acute pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis requires at least 2 of the following:
Pancreatic tests ( enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body’s constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes and other products):
Metabolic tests:
Hematologic tests and inflammatory markers:
Additional tests:
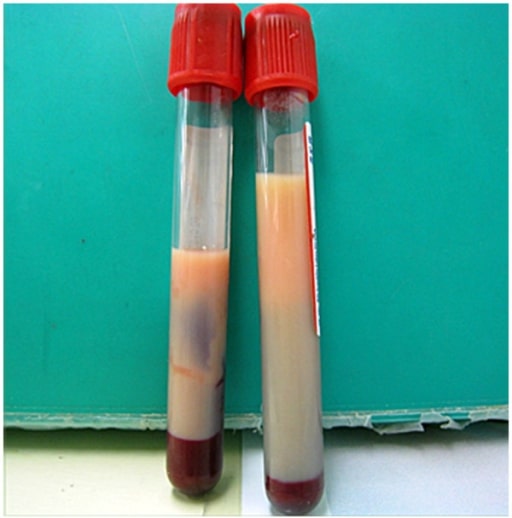
Milky plasma seen in a patient with hypertriglyceridemia: If seen, milky plasma should be considered as a potential cause of acute pancreatitis.
Image: “Milky plasma” by the Department of Emergency and Critical Care Medicine, Ohta Nishinouchi Hospital, 2-5-20 Nishinouchi, Koriyama, Fukushima, 963-8558, Japan. License: CC BY 2.0.Imaging may not be required if the 1st 2 diagnostic criteria are met MET Preoperative Care, but can be used for evaluating the underlying cause and complications:
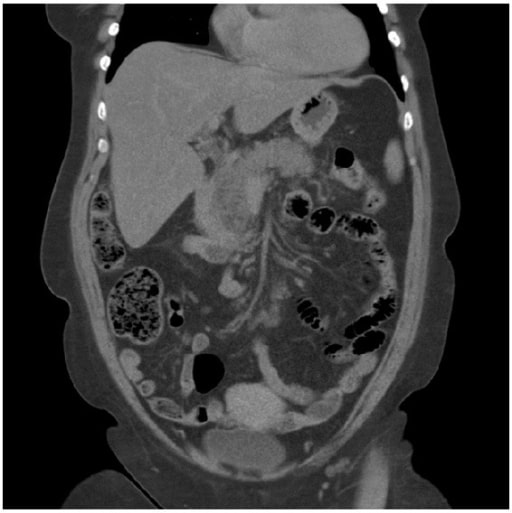
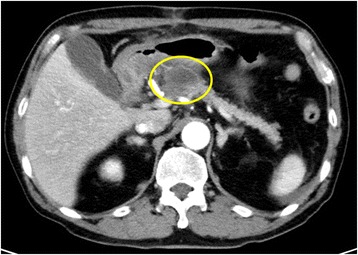
Acute pancreatitis: A CT scan showing pancreatitis changes, which appears enlarged and edematous.
Image: “A computed tomography scan” by Department of Surgery, Helsingborg Hospital, 25187 Helsingborg, Sweden. License: CC BY 3.0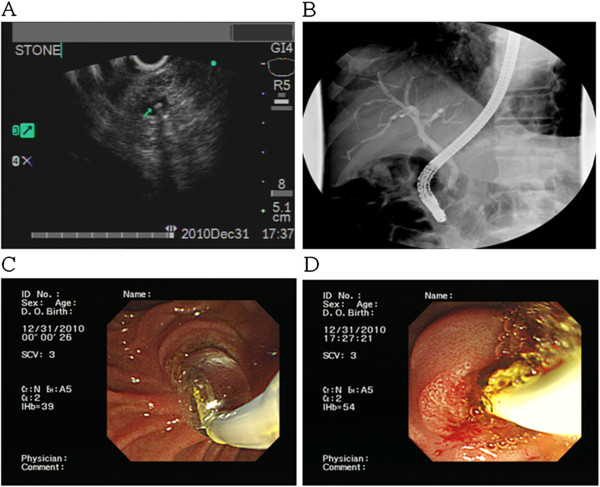
A tiny CBD stone is revealed using US. Such stones should be considered a potential etiology in a patient presenting with acute pancreatitis.
Image: “F2” by the Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Veterans General Hospital, 386 Ta-Chung 1st Road, Kaohsiung 81362, Taiwan. License: CC BY 2.0, edited by Lecturio.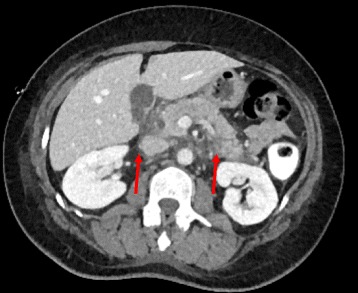
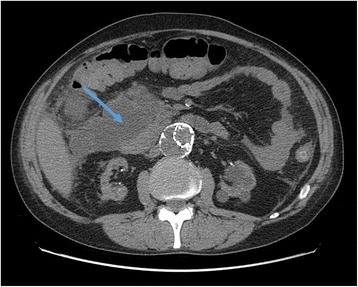
Acute pancreatitis on CT scan, showing edema around the pancreas
Image: “Arterial phase contrast CT showing an acute pancreatitis” by Benoît Bédat et al. License: CC BY 4.0.Identifying the severity of acute pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis is helpful in order to ensure the patient is treated appropriately:
| Present on admission | At 48 hours after admission |
|---|---|
| Age > 55 years | Decrease in hematocrit Hematocrit The volume of packed red blood cells in a blood specimen. The volume is measured by centrifugation in a tube with graduated markings, or with automated blood cell counters. It is an indicator of erythrocyte status in disease. For example, anemia shows a low value; polycythemia, a high value. Neonatal Polycythemia > 10% |
| WBC > 16,000/μL | Increase in BUN by ≥ 5 mg/dL |
| Blood glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance > 200 mg/dL | Serum Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts) < 8 mg/dL |
| Serum LDH LDH Osteosarcoma > 350 IU/L | PaO2 < 60 mm Hg |
| Aspartate Aspartate One of the non-essential amino acids commonly occurring in the l-form. It is found in animals and plants, especially in sugar cane and sugar beets. It may be a neurotransmitter. Synthesis of Nonessential Amino Acids transaminase Transaminase A subclass of enzymes of the transferase class that catalyze the transfer of an amino group from a donor (generally an amino acid) to an acceptor (generally a 2-keto acid). Most of these enzymes are pyridoxyl phosphate proteins. Catabolism of Amino Acids ( AST AST Enzymes of the transferase class that catalyze the conversion of l-aspartate and 2-ketoglutarate to oxaloacetate and l-glutamate. Liver Function Tests) > 250 IU/L | Base deficit > 4 mEq/L |
| Estimated fluid sequestration > 6 L |
| BUN | > 25 mg/dL |
|---|---|
| Impaired mental status | GCS GCS A scale that assesses the response to stimuli in patients with craniocerebral injuries. The parameters are eye opening, motor response, and verbal response. Coma < 15 |
| Systemic inflammatory response syndrome Systemic Inflammatory Response Syndrome Sepsis in Children (SIRS) | Evidence of SIRS |
| Age | > 60 years |
| Pleural effusion Pleural Effusion Pleural effusion refers to the accumulation of fluid between the layers of the parietal and visceral pleura. Common causes of this condition include infection, malignancy, autoimmune disorders, or volume overload. Clinical manifestations include chest pain, cough, and dyspnea. Pleural Effusion | Positive finding on imaging |
| Characteristics | CTSI | MCTSI | |
|---|---|---|---|
| Pancreatic inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation | Normal pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy | 0 | 0 |
| Focal or diffuse enlargement of the pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy | 1 | 2 | |
| Intrinsic pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy abnormalities or peripancreatic inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation | 2 | 2 | |
| Single acute fluid collection | 3 | 4 | |
| ≥ 2 acute fluid collections or peripancreatic gas | 4 | 4 | |
| Pancreatic parenchymal necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage | None | 0 | 0 |
| < 30% | 2 | 2 | |
| 30–50% | 4 | 4 | |
| > 50% | 6 | 4 | |
| Extrapancreatic complications | Pleural effusion Pleural Effusion Pleural effusion refers to the accumulation of fluid between the layers of the parietal and visceral pleura. Common causes of this condition include infection, malignancy, autoimmune disorders, or volume overload. Clinical manifestations include chest pain, cough, and dyspnea. Pleural Effusion, ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites, GI/vascular/parenchymal complications | N/A | 2 |
| Score interpretation | |||
| Patient risk factors | |
|---|---|
| Laboratory findings | |
| Radiologic findings |
Basic treatment:[3,12,15,17–19]
Setting and specific nutrition:[3,15,17–20,22]
Antibiotics:[15,18.19]
Gallstones Gallstones Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis:[3,15,18,19]
Hypertriglyceridemia Hypertriglyceridemia A condition of elevated levels of triglycerides in the blood. Lipid Disorders:[5]
Alcohol:[17]
Abdominal CT scan showing the initial area of patchy necrosis around the head of the pancreas
Image: “Abdominal CT scan” by Francesco Fontana. License: CC BY 4.0.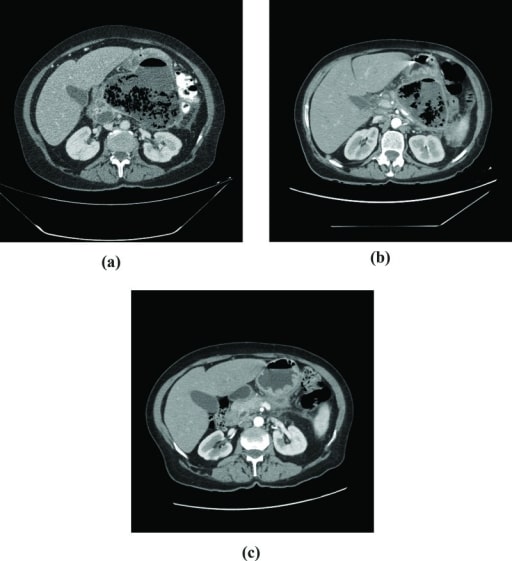
CT scans in a patient who developed infected pancreatic necrosis:
A: Extensive pancreatic necrosis with a large amount of gas is seen in the body and tail of the pancreas.
B: After 60 days of follow-up, a small decrease in the collection of gas is noted.
C: 4 months after hospital discharge: atrophy of pancreatic parenchyma
Acute pancreatitis repeatedly occurred 1 month after the 1st operation, and a pancreatic pseudocyst developed at the same site. Enhanced CT showed a cyst with a diameter of 29 mm in the body of the pancreas.
Image: “Pancreatic pseudocyst” by the Department of Gastroenterological Surgery, Kumamoto University Graduate School of Medical Sciences, 1-1-1 Honjo, Kumamoto, 860-8556 Japan. License: CC BY 4.0.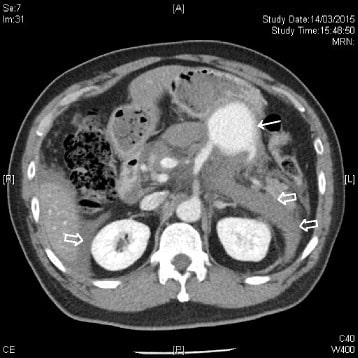
CT scan of the abdomen with IV contrast showing a contrast-enhanced mass (solid arrow) at the splenic artery (branching from the superior mesenteric artery) compatible with a splenic artery pseudoaneurysm. Hemoretroperitoneum and hemoperitoneum were demonstrated (hollow arrows).
Image: “CT scan of the abdomen” by the Accident and Emergency Department, Ruttonjee Hospital, Wanchai, Hong Kong. License: CC BY 4.0.
Contrast-enhanced CT scan of the abdomen reveals a 5 × 6 × 7 cm complex cystic mass in the region of the uncinate process of the pancreatic head with an enhancing capsule and a small hyperdensity consistent with pseudoaneurysm of a peripancreatic vessel with active bleeding into the pancreatic pseudocyst.
Image: “Contrast-enhanced CT scan” by Rohan Mandaliya. License: CC BY 2.0.