Irritable bowel syndrome (IBS) is a functional bowel disease characterized by chronic abdominal pain and altered bowel habits without an identifiable organic cause. The etiology and pathophysiology of this disease are not well understood, and there are many factors that may contribute. Irritable bowel syndrome is a diagnosis of exclusion, and organic causes should be ruled out. Once diagnosed, the emphasis is on education and reassurance. Dietary modifications and symptom-control measures may also be instituted, depending on the predominant symptoms.
Last updated: Mar 4, 2024
Although no specific organic cause has been identified, there are several possible pathogenic mechanisms.
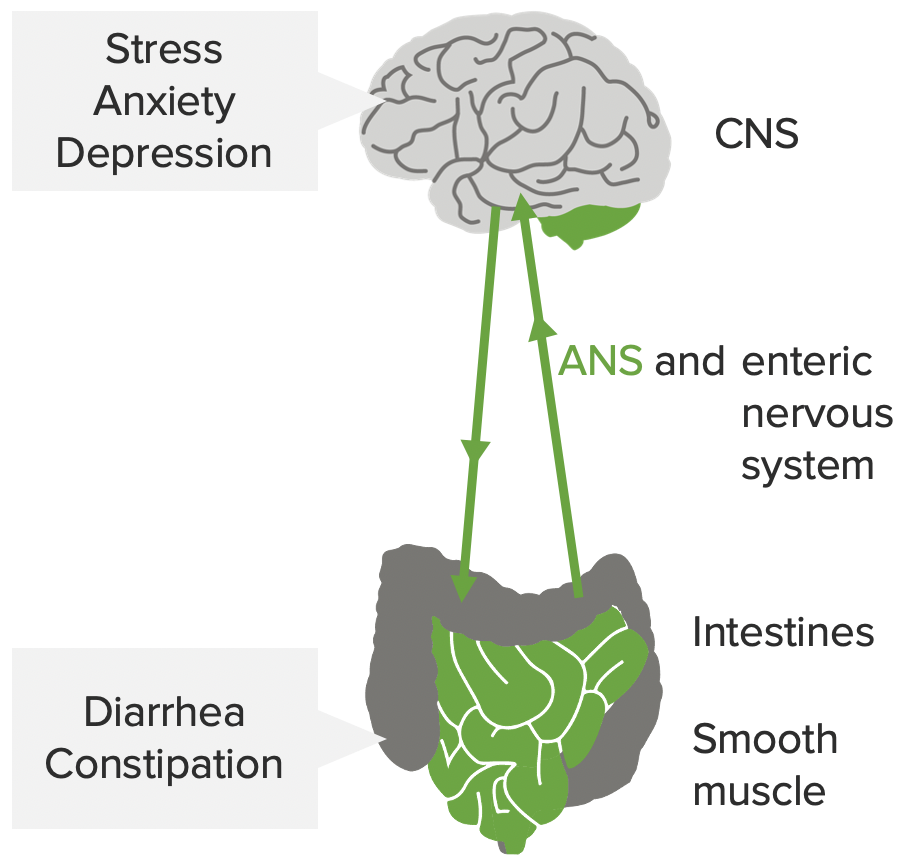
The mind-gut interaction contributing to the pathophysiology of IBS: stress, anxiety, and depression influence the CNS, autonomic nervous system (ANS), and enteric nervous system. This may affect the smooth muscles in the intestines, leading to the symptoms of IBS.
Image by Lecturio.Irritable bowel syndrome Irritable bowel syndrome Irritable bowel syndrome (IBS) is a functional bowel disease characterized by chronic abdominal pain and altered bowel habits without an identifiable organic cause. The etiology and pathophysiology of this disease are not well understood, and there are many factors that may contribute. Irritable Bowel Syndrome is classified based on the clinical presentation.
Irritable bowel syndrome Irritable bowel syndrome Irritable bowel syndrome (IBS) is a functional bowel disease characterized by chronic abdominal pain and altered bowel habits without an identifiable organic cause. The etiology and pathophysiology of this disease are not well understood, and there are many factors that may contribute. Irritable Bowel Syndrome is a diagnosis of exclusion, but the Rome IV criteria Rome Iv Criteria Elimination Disorders (calculator) help provide a standardized diagnosis:
To define abnormal bowel movements, the Bristol Stool Form Scale Scale Dermatologic Examination is used. Types 1 and 2 (found in IBS-C) and 6 and 7 (found in IBS-D) are considered abnormal:
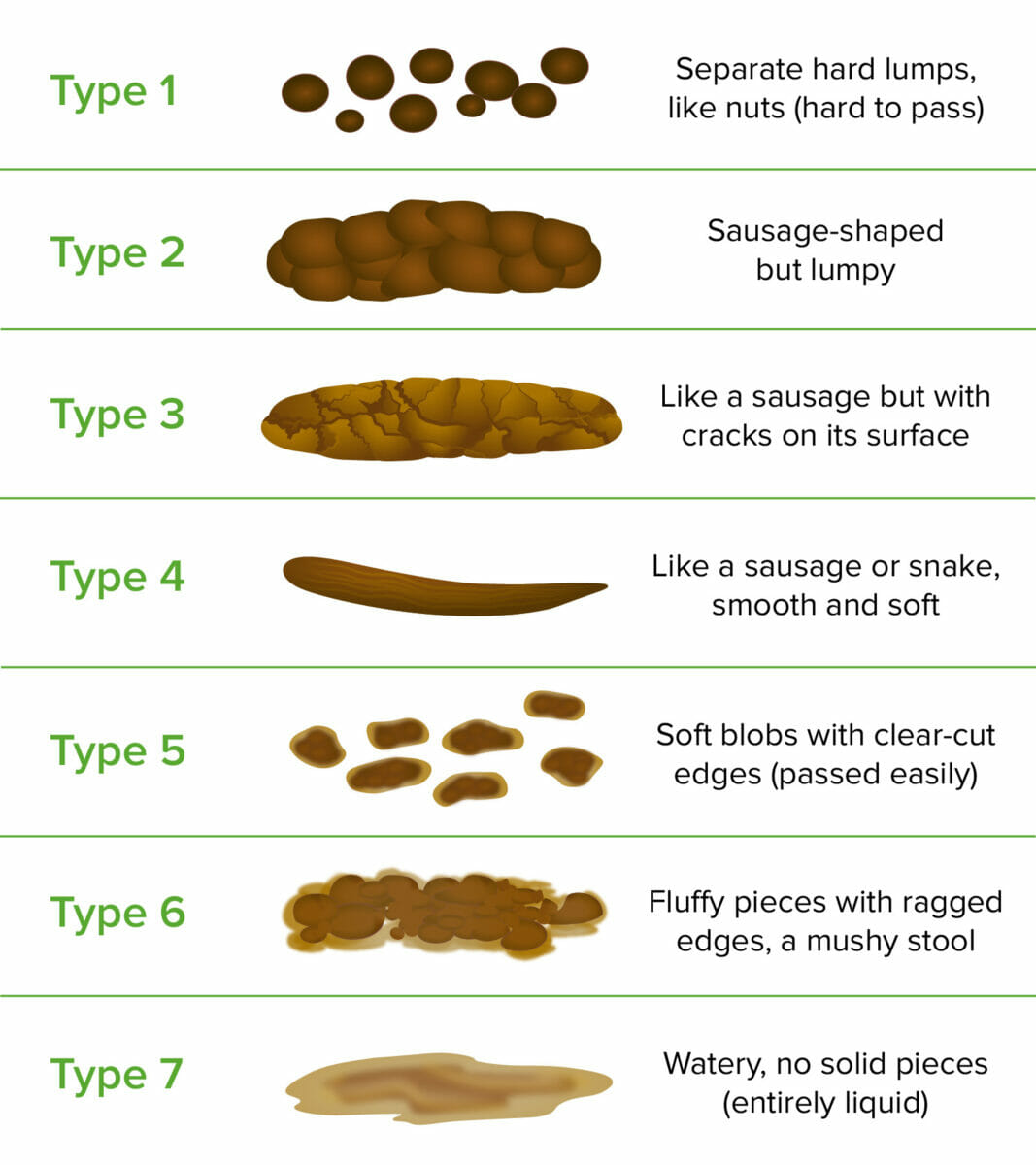
Bristol Stool Form Scale.
Image by Lecturio.Work-up will be guided by the patient’s clinical presentation. Those who meet the diagnostic criteria and do not have other alarm features (or warning signs) require limited tests.[8,9,10]
Management may vary depending on practice location. The following information is based on US and UK literature and guidelines for adult patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.
IBS-D:
| Medication | Typical dose (adult) |
|---|---|
| Loperamide Loperamide One of the long-acting synthetic antidiarrheals; it is not significantly absorbed from the gut, and has no effect on the adrenergic system or central nervous system, but may antagonize histamine and interfere with acetylcholine release locally. Antidiarrheal Drugs | |
| Cholestyramine Cholestyramine A strongly basic anion exchange resin whose main constituent is polystyrene trimethylbenzylammonium cl(-) anion. Lipid Control Drugs | 2–4 g/day |
| Colesevelam Colesevelam An allylamine derivative that binds bile acids in the intestine and is used as an anticholesteremic agent in the treatment of hypercholesterolemia and hyperlipidemias. Lipid Control Drugs | 3.75 g daily |
| Ondansetron Ondansetron A competitive serotonin type 3 receptor antagonist. It is effective in the treatment of nausea and vomiting caused by cytotoxic chemotherapy drugs, including cisplatin, and has reported anxiolytic and neuroleptic properties. Antiemetics | 4–8 mg up to 3 times daily |
| Alosetron | 0.5 mg 2 times daily |
| Eluxadoline | |
| Rifaximin Rifaximin A synthetic rifamycin derivative and anti-bacterial agent that is used for the treatment of gastroenteritis caused by Escherichia coli infections. It may also be used in the treatment of hepatic encephalopathy. Hepatic Encephalopathy | 550 mg 3 times daily for 14 days |
IBS-C:[6,8,11]
| Medication | Typical dose (adult) |
|---|---|
| Lubiprostone | 8 μg 2 times daily (for adult women) |
| Linaclotide | 290 μg daily |
| Plecanatide | 3 mg daily |
| Tegaserod | 6 mg 2 times daily |
| Tenapanor | 50 mg 2 times daily |
Abdominal pain Abdominal Pain Acute Abdomen and bloating Bloating Constipation:
Other recommendations: