Trichotillomania (hair-pulling disorder (HPD)) is defined as repetitive pulling of one’s hair resulting in hair loss that may be visible to others. This disorder is classified under obsessive-compulsive and related disorders, as there is tension prior to the act that is relieved after the hair-pulling. Diagnosis is made clinically through history taking and physical exam. Treatment is multimodal, using behavioral interventions to recognize and properly respond to the tension and pharmacotherapy, which is beneficial in some cases.
Last updated: Dec 17, 2024
Trichotillomania, also known as hair-pulling disorder, is characterized by a repetitive or deliberate desire to pull one’s hair, done unconsciously.
Most people suffering from trichotillomania tend to pull out hair from their head, eyelashes, eyebrows, legs, arms, face, and pubic region Pubic region Anterior Abdominal Wall: Anatomy.
2 types of hair pulling:
Oral manipulation often occurs:

Trichotillomania lesions on the vertex of the scalp
Image: “Trichotillomania lesions on vertex of scalp” by Department of General Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, India. License: CC BY 3.0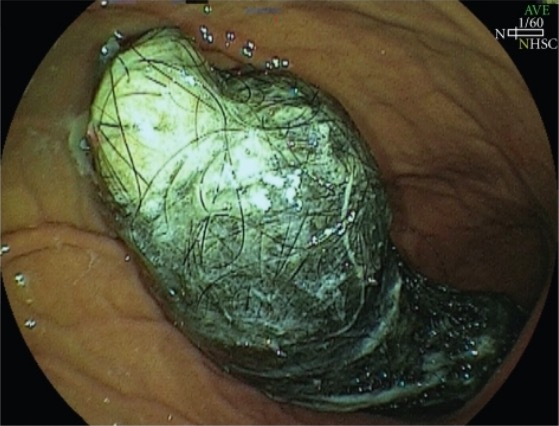
Swallowed hair: endoscopic image of an intragastric trichobezoar
Image: “Intragastric trichobezoar” by Department of Surgery, School of Medicine, University of Campinas (Unicamp), Rua Tessália Vieira de Camargo, 126 – Cidade Universitária Zeferino Vaz, Campínas – SP – CEP: 13083-887, Brazil. License: CC BY 3.0Management usually involves collaborative care between dermatologists and psychiatrists.
Cognitive-behavioral therapy Cognitive-behavioral therapy Cognitive-behavioral therapy corrects faulty assumptions and tries to replace maladaptive behavior with healthier alternatives. Psychotherapy (habit-reversal training):
Behavioral treatments such as self-monitoring and biofeedback Biofeedback The therapy technique of providing the status of one’s own autonomic nervous system function (e.g., skin temperature, heartbeats, brain waves) as visual or auditory feedback in order to self-control related conditions (e.g., hypertension, migraine headaches). Psychotherapy also have exhibited some effectiveness.