Budd-Chiari syndrome is a condition resulting from the interruption of the normal outflow of blood from the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy. The primary type arises from a venous process (affecting the hepatic veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology or inferior vena cava Inferior vena cava The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy) such as thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus, but can also be from a lesion compressing or invading the veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology (secondary type). The patient typically presents with hepatomegaly, ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites, and abdominal discomfort. Onset is often subacute or chronic. Diagnosis is confirmed by Doppler Doppler Ultrasonography applying the doppler effect, with frequency-shifted ultrasound reflections produced by moving targets (usually red blood cells) in the bloodstream along the ultrasound axis in direct proportion to the velocity of movement of the targets, to determine both direction and velocity of blood flow. Ultrasound (Sonography) ultrasound. Treatment involves addressing the underlying condition that caused the venous occlusion. Further management involves prevention of further clotting ( anticoagulation Anticoagulation Pulmonary Hypertension Drugs), restoration of blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure, and decompressing the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy. Liver transplantation Liver transplantation The transference of a part of or an entire liver from one human or animal to another. Hepatocellular Carcinoma (HCC) and Liver Metastases is considered if initial treatment fails and/or the patient has decompensated liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis.
Last updated: Dec 15, 2025
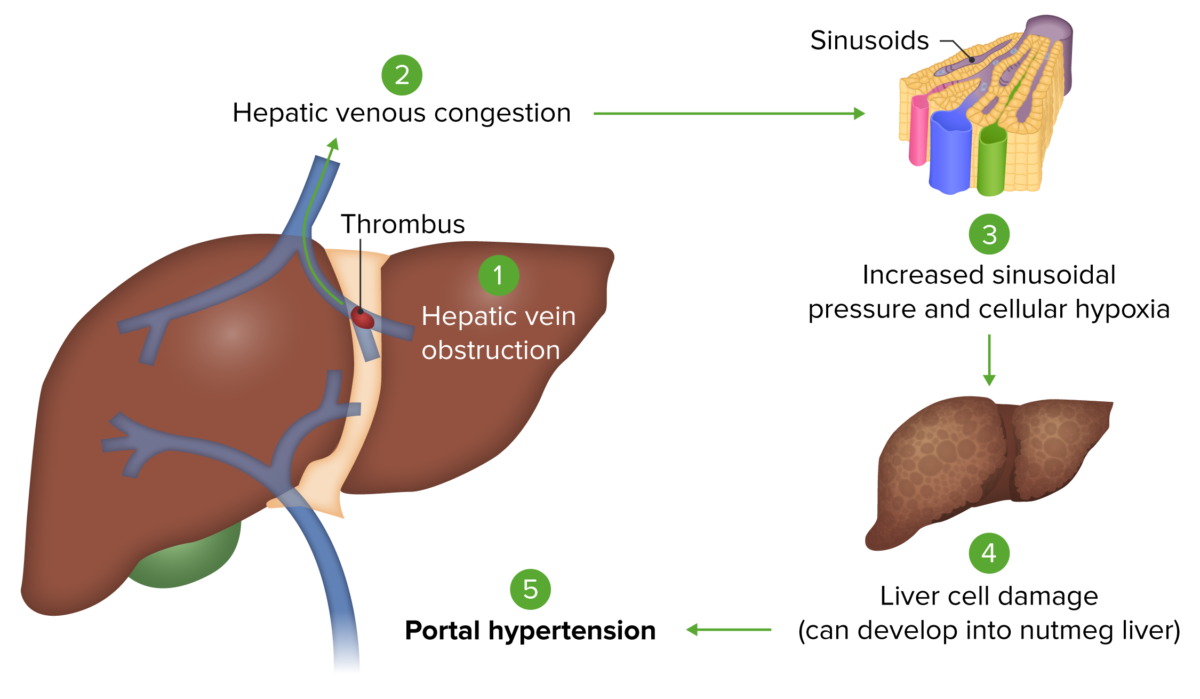
Budd-Chiari syndrome: Occlusion of hepatic veins causes hepatic venous congestion. This congestion increases the sinusoidal pressure within the liver, leading to reduced hepatic blood flow. This eventually produces hepatocellular injury from hypoxia. Hepatic damage then results in portal hypertension.
Image by Lecturio.
Image showing patient with ascites undergoing paracentesis
Image: “Draining ascites, secondary to hepatic cirrhosis” by John Campbell. License: Public Domain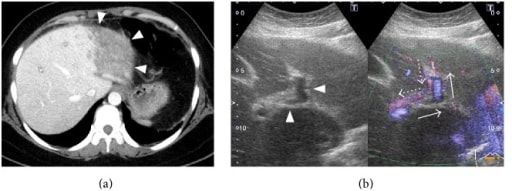
34-year-old woman with antiphospholipid syndrome presenting with acute Budd-Chiari syndrome.
(a) Dynamic CT: poor enhancement of the lateral segment of the left lobe of the liver (arrowheads).
(b) Doppler ultrasonography of the intrahepatic part of the portal vein: left branch of the portal vein (arrowheads) shows reflux (arrows: normal blood flow; dotted arrows: blood flow noted in this patient).
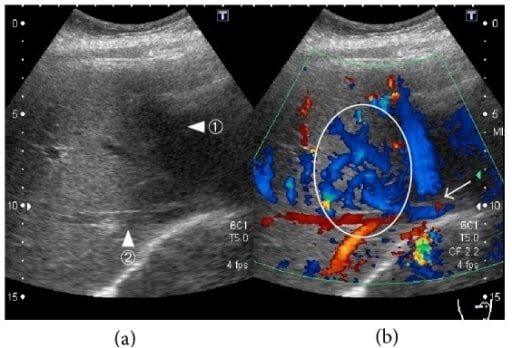
34-year-old woman with acute Budd-Chiari syndrome (thrombosis in the middle and left hepatic vein), Doppler ultrasonography of the hepatic veins:
(a) Middle hepatic vein (arrowhead ①) and right hepatic vein (arrowhead ②).
(b) Blood flow is absent in parts of the middle hepatic vein (arrow). Increased blood flow is seen in the region from the middle hepatic vein to the right hepatic vein (circle).
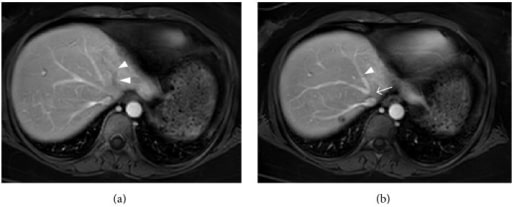
Contrast-enhanced MRI of a 34-year-old woman with acute Budd-Chiari syndrome (left and middle hepatic vein occlusion):
(a) There is no contrast enhancement in the left hepatic vein (arrowhead).
(b) The middle hepatic vein (arrowhead) is visualized, but there is no enhancement at its confluence with the inferior vena cava (arrow), suggesting obstruction.