Authors: Ahmed Elsherif 1 ; Michelle Wyatt 2
Peer Reviewers: Stanley Oiseth 3 ; Joseph Alpert 4
Affiliations: 1 Suez Canal University; 2 Medical Editor at Lecturio; 3 Chief Medical Editor at Lecturio; 4 Tucson University, Arizona
This article is not intended to substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition.
Ischemic heart disease
Types of ischemic heart disease
Image by Lecturio.Definition
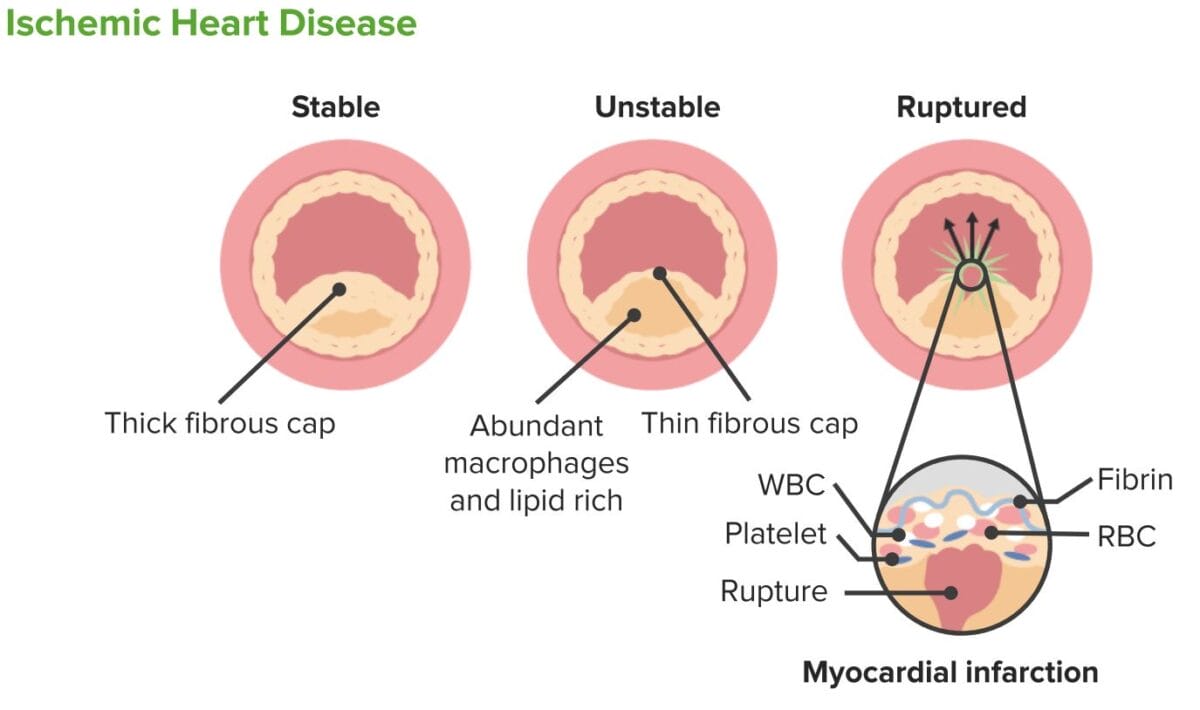
Ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease ( IHD IHD Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease) describes a wide range of clinical conditions in which there is an imbalance between oxygen supply and the myocardial demand, resulting in ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage to a portion of the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy. [5] IHD IHD Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease is classified into chronic, stable disease ( stable angina Stable angina Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia. Stable and Unstable Angina) and acute, unstable disease (acute coronary syndromes).
Stable angina Stable angina Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia. Stable and Unstable Angina refers to chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways when myocardial oxygen demand Myocardial oxygen demand Stable and Unstable Angina exceeds oxygen supply. Inadequate blood supply is most often due to coronary artery Coronary Artery Truncus Arteriosus atherosclerotic disease.
Anatomy
The major coronary vessels are the right coronary artery Right coronary artery Heart: Anatomy (RCA), the left coronary artery Left coronary artery Heart: Anatomy (LCA), the left circumflex anterior artery (LCx), and the left anterior descending (LAD) artery.
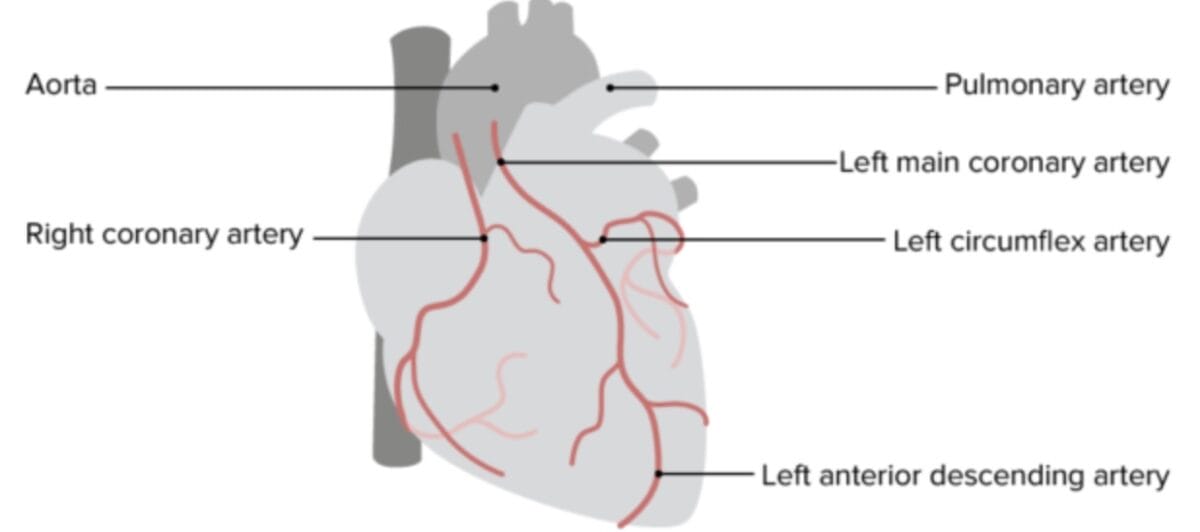
An individual’s specific coronary anatomy and dominance are clinically significant as the location of the thrombus results in varying clinical pictures (with different management indicated). Approximately 80–85% of people are “right-dominant,” [6,7] which means that the posterior descending artery (PDA) originates from the RCA. The other 15–20% are “left-dominant” (PDA originates from the LCx) or “codominant” (there are right and left PDAs originating from the RCA and LCx. The magnitude of an RCA infarct depends on the distance of the acute occlusion from the origin and the dominance of the vessel. A proximal RCA occlusion in a right-dominant patient can present with a right ventricular infarct and cardiogenic shock. In contrast, a distal RCA occlusion may present with a smaller area of inferoseptal infarct and inferior left ventricular (LV) dysfunction.
Image by Lecturio.Epidemiology
IHD IHD Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease is the leading cause of death worldwide. It is considered the most common chronic illness in the United States, accounting for 42% of cardiovascular deaths. Stable angina Stable angina Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia. Stable and Unstable Angina occurs in about 14 % of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with IHD IHD Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease, and unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina results in 1 million hospitalizations annually. [3,4]
Lifetime risk of coronary heart disease Coronary heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease: [8]
- At age 40: 49% in men and 32% in women
- At age 75: 35% in men and 24% in women
Risk Factors
The most common risk factor of coronary heart disease Coronary heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease is atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis of the epicardial coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology, resulting in partial or complete obstruction with subsequent inadequate perfusion of the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy supplied by its regional coronary artery Coronary Artery Truncus Arteriosus.
Many risk factors contribute to the pathophysiology of coronary heart disease Coronary heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease. Major modifiable risk factors include cigarette smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus, and hyperlipidemia. For the most part, atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis is an irreversible process. Defined risk factors can be reduced through lifestyle changes, including diet, exercise, maintaining a healthy weight, and smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases cessation. [9,10] Cholesterol-lowering medications such as statins Statins Statins are competitive inhibitors of HMG-CoA reductase in the liver. HMG-CoA reductase is the rate-limiting step in cholesterol synthesis. Inhibition results in lowered intrahepatocytic cholesterol formation, resulting in up-regulation of LDL receptors and, ultimately, lowering levels of serum LDL and triglycerides. Statins may cause plaque Plaque Primary Skin Lesions regression Regression Corneal Abrasions, Erosion, and Ulcers in some cases.[11,49] Other risk factors for CHD include male gender Gender Gender Dysphoria, family history Family History Adult Health Maintenance of CAD in a first-degree family member (< age 55 in men, < 65 in women), sedentary lifestyle, obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity, hyperglycemia Hyperglycemia Abnormally high blood glucose level. Diabetes Mellitus, and psychological or emotional stress.[12]
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction at young ages (<30) may have familial lipid metabolism Lipid Metabolism Lipid metabolism is the processing of lipids for energy use, energy storage, and structural component production. Lipid metabolism uses fats from dietary sources or from fat stores in the body. A complex series of processes involving digestion, absorption, and transport are required for the proper metabolism of lipids. Lipid Metabolism disorders, connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology disease, uncontrolled type 1 Type 1 Spinal Muscular Atrophy diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus, or vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus. Coronary anomalies, substance abuse disorders, antiphospholipid syndrome Antiphospholipid syndrome Antiphospholipid syndrome (APLS) is an acquired autoimmune disorder characterized by the persistent presence of antiphospholipid antibodies, which create a hypercoagulable state. These antibodies are most commonly discovered during a workup for a thrombotic event or recurrent pregnancy loss, which are the 2 most common clinical manifestations. Antiphospholipid Syndrome, and hyperviscosity Hyperviscosity Hypercoagulable States syndrome should also be considered during history taking.[13]
Pathophysiology of CHD
Stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) of the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology can lead to an insufficient oxygen supply to the myocardial tissue or decreased coronary flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure reserve, the ratio of maximum flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure to resting flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure. A vasodilatory stimulus in normal coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology results in approximately a fourfold increase in flow rate Flow rate maximum flow the ventilator will deliver a set tidal volume in liters per minute Invasive Mechanical Ventilation compared to baseline. With progressive stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), baseline flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure remains normal until the coronary artery Coronary Artery Truncus Arteriosus is narrowed by 70%–75%. However, coronary flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure reserve begins to decrease at 40%–50% diameter stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS). Coronary flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure reserve decreases to two times baseline at approximately 75% stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), indicating myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease.[14,15]
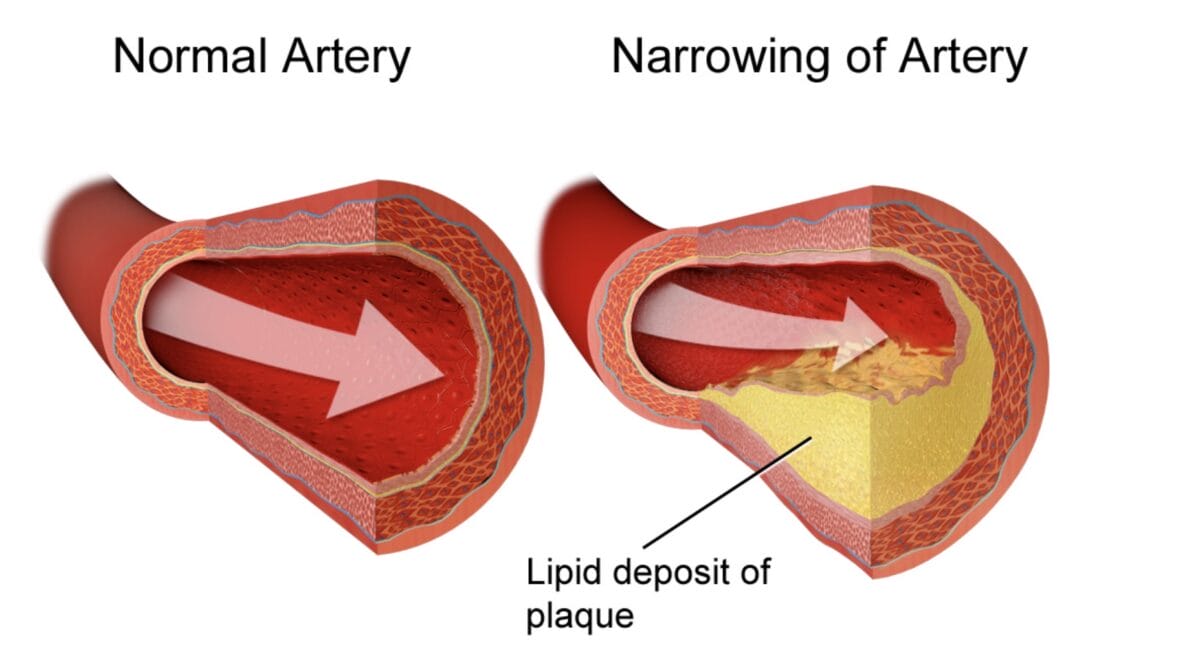
Drawings of a normal artery and an artery with an atherosclerotic plaque, as typically seen with coronary artery disease. The atherosclerotic plaque has an irregular morphology and may not involve the entire circumference of the artery, as depicted here.
Image: “Coronary Artery Disease” by BruceBlaus. License: CC BY 3.0Myocardial Oxygen Demand Myocardial oxygen demand Stable and Unstable Angina
Four major factors determine the oxygen demand of the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy:
- Heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology
- Systolic blood pressure ( afterload Afterload Afterload is the resistance in the aorta that prevents blood from leaving the heart. Afterload represents the pressure the LV needs to overcome to eject blood into the aorta. Cardiac Mechanics)
- Tension on the myocardial wall ( preload Preload Cardiac Mechanics)
- Myocardial contractility
Any clinical condition increasing these factors will also increase the myocardial oxygen demand Myocardial oxygen demand Stable and Unstable Angina and result in ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, such as tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, and ventricular hypertrophy Ventricular Hypertrophy Tetralogy of Fallot.
Myocardial Oxygen Supply Myocardial oxygen supply Stable and Unstable Angina
The capacity of the blood to carry oxygen to the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy is affected by factors such as the hemoglobin level, oxygen tension, and the amount of extracted oxygen from hemoglobin to the tissue, which is related to 2,3 diphosphoglycerate levels. Another factor is coronary artery Coronary Artery Truncus Arteriosus blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure, which is affected by the following factors:
- Coronary artery Coronary Artery Truncus Arteriosus diameter– atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis is the most frequent cause of coronary artery Coronary Artery Truncus Arteriosus narrowing and obstruction.
- Coronary artery Coronary Artery Truncus Arteriosus tone–reduces the oxygen supply without significant underlying atherosclerotic changes, as seen with vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina.
- Perfusion pressure–determined by the pressure gradient Pressure gradient Vascular Resistance, Flow, and Mean Arterial Pressure from the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy to the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology.
- Heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology– coronary artery Coronary Artery Truncus Arteriosus flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure occurs mainly during diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle; extreme tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children decreases the duration of diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle and blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure into the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology.
Any clinical condition affecting these factors will reduce the myocardial oxygen supply Myocardial oxygen supply Stable and Unstable Angina and result in ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage.[16]
The studies on the pathophysiology of atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis emphasize the roles of various factors in the progression and severity of the disease. Baumer et al AL Amyloidosis. found that cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism crystals are a crucial contributor to the development of atherosclerotic plaques.[53] Ehara et al AL Amyloidosis. reported that elevated levels of oxidized low-density lipoprotein Low-density lipoprotein A class of lipoproteins of small size (18-25 nm) and light (1. 019-1. 063 g/ml) particles with a core composed mainly of cholesterol esters and smaller amounts of triglycerides. The surface monolayer consists mostly of phospholipids, a single copy of apolipoprotein B-100, and free cholesterol molecules. The main ldl function is to transport cholesterol and cholesterol esters to extrahepatic tissues. Cholesterol Metabolism are positively associated with the severity of acute coronary syndromes, indicating its role in plaque Plaque Primary Skin Lesions instability.[54] Poznyak and colleagues highlighted the involvement of key signaling pathways and genes Genes A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. DNA Types and Structure in foam cell formation and the influence of the renin-angiotensin system on the pathogenesis of atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis, suggesting targets for cardiovascular disease treatment.[55.56]
Classification
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with coronary heart disease Coronary heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease (CHD) can present with:
- Chronic disease–most commonly presents with
stable angina
Stable angina
Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia.
Stable and Unstable Angina, defined as substernal discomfort or pressure (the most widely used descriptor) precipitated by exertion or other stress, with
radiation
Radiation
Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles).
Osteosarcoma to the shoulder,
jaw
Jaw
The jaw is made up of the mandible, which comprises the lower jaw, and the maxilla, which comprises the upper jaw. The mandible articulates with the temporal bone via the temporomandibular joint (TMJ). The 4 muscles of mastication produce the movements of the TMJ to ensure the efficient chewing of food.
Jaw and Temporomandibular Joint: Anatomy, or inner aspect of the
arm
Arm
The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior).
Arm: Anatomy relieved by rest or
nitroglycerin
Nitroglycerin
A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives.
Nitrates in less than 10 minutes. It is typically triggered by physical exertion,
psychological stress
Psychological stress
Stress wherein emotional factors predominate.
Acute Stress Disorder, or exposure to the cold. The same type and degree of exertion or stress (e.g., walking up 2 flights of stairs) produce the same symptoms. It usually subsides within 10 minutes after rest or taking
nitroglycerin
Nitroglycerin
A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives.
Nitrates. Suspect ACS in angina lasting longer than 20 minutes.
- Note: Stable anginal pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is always of similar intensity and quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement.
- Acute coronary syndromes (ACS)–almost always associated with rupture of an atherosclerotic plaque Plaque Primary Skin Lesions, followed quickly by partial or complete thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus of the affected artery. ACS is a term that includes unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina (UA) and acute myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction. Acute MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction is divided into ST-segment elevation myocardial infarctions (STEMI), and non-ST-segment elevation myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (NSTEMI), and their management differs.
-
Unstable angina
Unstable angina
Precordial pain at rest, which may precede a myocardial infarction.
Stable and Unstable Angina (UA) is defined as
myocardial ischemia
Myocardial ischemia
A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart.
Coronary Heart Disease at rest or with minimal exertion in the absence of acute myocardial injury/
necrosis
Necrosis
The death of cells in an organ or tissue due to disease, injury or failure of the blood supply.
Ischemic Cell Damage. It may be characterized by: prolonged (>20 minutes) angina at rest; new onset of angina; angina that is increasing in frequency, duration,
trigger
Trigger
The type of signal that initiates the inspiratory phase by the ventilator
Invasive Mechanical Ventilation
threshold
Threshold
Minimum voltage necessary to generate an action potential (an all-or-none response)
Skeletal Muscle Contraction, or that which occurs after a recent episode of
myocardial infarction
Myocardial infarction
MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms.
Myocardial Infarction. Many previously diagnosed UAs were probably NSTEMIs, which are now diagnosed with the sensitive biomarkers of
necrosis
Necrosis
The death of cells in an organ or tissue due to disease, injury or failure of the blood supply.
Ischemic Cell Damage,
troponin I
Troponin I
A troponin complex subunit that inhibits actomyosin ATPase activity thereby disrupting actin and myosin interaction. There are three troponin I subtypes: troponin i1, i2 and i3. Troponin i3 is cardiac-specific whereas troponin i1 and i2 are skeletal subtypes. Troponin i3 is a biomarker for damaged or injured cardiac myocytes and mutations in troponin i3 gene are associated with familial hypertrophic cardiomyopathy.
Myocardial Infarction or T. [2]
- Note: New-onset angina occurring for the first time is by definition unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina
- Sudden cardiac death Sudden cardiac death Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest ( SCD SCD Sickle cell disease (SCD) is a group of genetic disorders in which an abnormal Hb molecule (HbS) transforms RBCs into sickle-shaped cells, resulting in chronic anemia, vasoocclusive episodes, pain, and organ damage. Sickle Cell Disease)– unexpected death due to cardiac causes, usually within 1 hour of symptom onset in a person with or without known cardiac disease, or within 24 hours of last being seen well if the death is unwitnessed. SCD SCD Sickle cell disease (SCD) is a group of genetic disorders in which an abnormal Hb molecule (HbS) transforms RBCs into sickle-shaped cells, resulting in chronic anemia, vasoocclusive episodes, pain, and organ damage. Sickle Cell Disease represents the first expression of CAD in many individuals who experience out-of-hospital cardiac arrest Cardiac arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest. Most cases are related to cardiac arrhythmias, and about 50% of all cardiac deaths are attributable to SCD SCD Sickle cell disease (SCD) is a group of genetic disorders in which an abnormal Hb molecule (HbS) transforms RBCs into sickle-shaped cells, resulting in chronic anemia, vasoocclusive episodes, pain, and organ damage. Sickle Cell Disease.[17,50]
- Vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina–caused by vasospasm occurring at rest; may occur with or without underlying atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis in the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology.
- Post-infarction angina–occurs within 2 weeks after myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction.
- Silent myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease–occurs without typical symptoms. It occurs more frequently in women, older adults, patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus (due to neuropathy Neuropathy Leprosy), and patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with chronic kidney disease Chronic Kidney Disease Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease. Atypical symptoms such as dizziness Dizziness An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. Lateral Medullary Syndrome (Wallenberg Syndrome), nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, generalized weakness, malaise Malaise Tick-borne Encephalitis Virus, and epigastric pain Epigastric pain Mallory-Weiss Syndrome (Mallory-Weiss Tear) may be presenting complaints.
Diagnostics
History
The classic presentation of a patient with stable ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease starts with episodes of chest discomfort described as a sense of pressure, choking, heaviness, or tightness in the chest. The pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways starts gradually, with the intensity increasing and decreasing (crescendo-decrescendo in nature) within minutes and typically lasts for 2–5 minutes and not longer than 20 minutes. Sometimes the pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is described as central substernal discomfort that the patient can’t localize but typically places his palm or clenched fist over the sternum Sternum A long, narrow, and flat bone commonly known as breastbone occurring in the midsection of the anterior thoracic segment or chest region, which stabilizes the rib cage and serves as the point of origin for several muscles that move the arms, head, and neck. Chest Wall: Anatomy. Typical pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways radiates to one of the dermatomes Dermatomes Spinal Cord: Anatomy between C8 to T4 T4 The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form triiodothyronine which exerts a broad spectrum of stimulatory effects on cell metabolism. Thyroid Hormones, most often to the left shoulder and left arm Arm The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy. It can also radiate to the interscapular region, back, epigastrium Epigastrium Surgical Anatomy of the Abdomen, and lower jaw Jaw The jaw is made up of the mandible, which comprises the lower jaw, and the maxilla, which comprises the upper jaw. The mandible articulates with the temporal bone via the temporomandibular joint (TMJ). The 4 muscles of mastication produce the movements of the TMJ to ensure the efficient chewing of food. Jaw and Temporomandibular Joint: Anatomy.
Episodes of angina are provoked by physical exertion and emotional stress and are relieved within minutes by rest or sublingual nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates. Angina may be associated with shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, diaphoresis, dizziness Dizziness An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. Lateral Medullary Syndrome (Wallenberg Syndrome), light-headedness, and fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia.[5] Clinicians should inquire about risk factors such as smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, hyperlipidemia, hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, and diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus.
Examination
Physical examination is usually unremarkable in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with stable angina Stable angina Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia. Stable and Unstable Angina when asymptomatic; however, clinicians should look for evidence of atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis at other sites, such as carotid bruits and peripheral vascular disease. A cardiac exam also evaluates for heart murmurs Heart murmurs Heart sounds caused by vibrations resulting from the flow of blood through the heart. Heart murmurs can be examined by heart auscultation, and analyzed by their intensity (6 grades), duration, timing (systolic, diastolic, or continuous), location, transmission, and quality (musical, vibratory, blowing, etc). Heart Sounds or extra sounds as evidence of valvular disease and left ventricular dysfunction.
Resting ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG)
ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) is usually normal between attacks but may show evidence of previous myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction or conduction delays. During an episode of chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, reversible ST-segment depression (injury pattern) or elevation, with or without T-wave inversion, is suggestive of myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease.
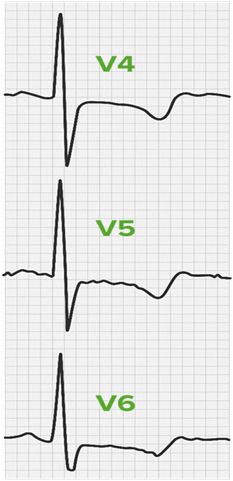
Resting ECG in a patient with stable angina during an episode of chest pain. Note the ST depression and T wave inversion in the lateral leads. These reversible changes are not seen after the pain resolves in a patient with stable CHD, and persistent changes with pain lasting more than 20 minutes signal an acute coronary syndrome with unstable angina.
Image by Lecturio.Exercise ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) (stress testing)
Noninvasive stress testing is used to establish the diagnosis and prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with stable ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease. Testing is done with a treadmill or bicycle for exercise, and imaging may be added with nuclear medicine Nuclear medicine A specialty field of radiology concerned with diagnostic, therapeutic, and investigative use of radioactive compounds. Nuclear Imaging testing, echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA), or cardiac MRI Cardiac MRI Imaging of the Heart and Great Vessels. A stress test with exercise treadmill testing (ETT) is generally safe in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with no resting abnormalities on ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG). There is a small risk of death or MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction in < 1 per 2500 tests. Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation are BP > 200/100 mm Hg, significant aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), and hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy. A treadmill ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) stress test is considered abnormal when horizontal or down-sloping ST-segment depression ≥ 1 mm at 60-80 ms MS Multiple sclerosis (MS) is a chronic inflammatory autoimmune disease that leads to demyelination of the nerves in the CNS. Young women are more predominantly affected by this most common demyelinating condition. Multiple Sclerosis after the J point is seen.[18]
In patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who cannot exercise due to physical limitations Limitations Conflict of Interest (e.g., leg Leg The lower leg, or just "leg" in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy amputation Amputation An amputation is the separation of a portion of the limb or the entire limb from the body, along with the bone. Amputations are generally indicated for conditions that compromise the viability of the limb or promote the spread of a local process that could manifest systemically. Amputation, severe arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis), pharmacologic stress testing using vasodilators Vasodilators Drugs used to cause dilation of the blood vessels. Thromboangiitis Obliterans (Buerger’s Disease) or dobutamine Dobutamine A catecholamine derivative with specificity for beta-1 adrenergic receptors. Sympathomimetic Drugs is an alternative to exercise for detecting physiologically significant coronary artery Coronary Artery Truncus Arteriosus stenoses.
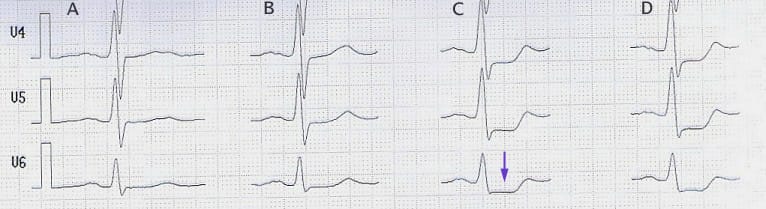
Stress-ECG showing ST-segment-depression (arrow) in columns C and D. An exercise treadmill test (ETT) is used to detect ischemia with exercise that is not present at rest. While exercising, this patient has at least 2 mm of ST depression indicative of ischemia. Some patients may have chest pain or arrhythmia provoked by stress testing. Planar or downsloping ST-segment depression of ≥ 1 mm is indicative of ischemia.
Image: “Belastungs-EKG eines Patienten mit koronarer Herzkrankheit” by J. Heuser. License: CC BY-SA 3.0Nuclear Cardiology Imaging
Stress myocardial perfusion imaging Myocardial perfusion imaging The creation and display of functional images showing where the blood is flowing into the myocardium by following over time the distribution of tracers injected into the bloodstream. Nuclear Imaging can show areas of diminished uptake of radioactive isotope by the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy at rest or during exercise. It helps diagnose CAD in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with abnormal resting ECGs and equivocal ETTs and can be performed either with an ETT or a pharmacologic stress test. [19] A stress test with single-photon emission CT ( SPECT SPECT An imaging technique using a device which combines tomography, emission-computed, single-photon and tomography, x-ray computed in the same session. Nuclear Imaging) uses 99mTc-labeled agents, such as 99mTc-sestamibi. For patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who cannot complete an adequate exercise stress test, a vasodilator stress test with SPECT SPECT An imaging technique using a device which combines tomography, emission-computed, single-photon and tomography, x-ray computed in the same session. Nuclear Imaging imaging uses agents such as dipyridamole Dipyridamole A phosphodiesterase inhibitor that blocks uptake and metabolism of adenosine by erythrocytes and vascular endothelial cells. Dipyridamole also potentiates the antiaggregating action of prostacyclin. Phosphodiesterase Inhibitors, adenosine Adenosine A nucleoside that is composed of adenine and d-ribose. Adenosine or adenosine derivatives play many important biological roles in addition to being components of DNA and RNA. Adenosine itself is a neurotransmitter. Class 5 Antiarrhythmic Drugs, or regadenoson (Lexiscan).
Angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery
Angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery visualizes the locations and severity of coronary artery Coronary Artery Truncus Arteriosus stenoses and is indicated when coronary revascularization Revascularization Thromboangiitis Obliterans (Buerger’s Disease) is considered.
CT angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery is rapidly becoming the diagnostic test of choice when coronary artery Coronary Artery Truncus Arteriosus disease is suspected. Coronary computed tomography angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery ( CCTA CCTA Imaging of the Heart and Great Vessels) evaluates the extent of CAD and helps in planning potential interventional or surgical therapy. CCTA CCTA Imaging of the Heart and Great Vessels has high sensitivity and a corresponding low rate of false negatives. The CAD-RADS (Reporting and Data System) classifies findings based on the degree of maximal coronary stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) to help guide management.[20]
Physiological assessments based on coronary computed tomography angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery, like computed tomography perfusion and FFR-CT, have proven valuable for identifying ischemia-causing lesions beyond just anatomical stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), improving diagnostic accuracy, and predicting cardiovascular outcomes. Recent studies and clinical trials demonstrate that using FFR-CT can decrease unnecessary invasive procedures and aid in determining specific lesions for revascularization Revascularization Thromboangiitis Obliterans (Buerger’s Disease), influencing treatment strategies and clinical decision-making in coronary artery Coronary Artery Truncus Arteriosus disease.[52]
Management
General measures for all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with CHD include discussion of lifestyle modification and control of the previously mentioned risk factors. It is essential to assess the extent and severity of atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis affecting different body organs.
Medical Treatment
- Antiplatelet therapy: Low-dose aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) or clopidogrel Clopidogrel A ticlopidine analog and platelet purinergic p2y receptor antagonist that inhibits adenosine diphosphate-mediated platelet aggregation. It is used to prevent thromboembolism in patients with arterial occlusive diseases; myocardial infarction; stroke; or atrial fibrillation. Antiplatelet Drugs (if aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) is contraindicated due to allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction or intolerance) should be prescribed for all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Newer agents include ticagrelor Ticagrelor An adenosine triphosphate analogue and reversible p2y12 purinoceptor antagonist that inhibits adp-mediated platelet aggregation. It is used for the prevention of thromboembolism by patients with acute coronary syndrome or a history of myocardial infarction. Antiplatelet Drugs and prasugrel Prasugrel A piperazine derivative and platelet aggregation inhibitor that is used to prevent thrombosis in patients with acute coronary syndrome; unstable angina and myocardial infarction, as well as in those undergoing percutaneous coronary interventions. Antiplatelet Drugs.
- Antianginal therapy: Nitrates Nitrates Nitrates are a class of medications that cause systemic vasodilation (veins > arteries) by smooth muscle relaxation. Nitrates are primarily indicated for the treatment of angina, where preferential venodilation causes pooling of blood, decreased preload, and ultimately decreased myocardial O2 demand. Nitrates cause venous and arterial dilatation, thus lowering myocardial oxygen demand Myocardial oxygen demand Stable and Unstable Angina by reducing the preload Preload Cardiac Mechanics and afterload Afterload Afterload is the resistance in the aorta that prevents blood from leaving the heart. Afterload represents the pressure the LV needs to overcome to eject blood into the aorta. Cardiac Mechanics on the heart. Sublingual nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates should be taken during an angina attack; it often relieves the pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways within 2–3 minutes. It can also be taken prophylactically before strenuous exercise Strenuous exercise Physical activity which is usually regular and done with the intention of improving or maintaining physical fitness or health. Contrast with physical exertion which is concerned largely with the physiologic and metabolic response to energy expenditure. Cardiovascular Response to Exercise. Isosorbide mono-and dinitrate are long-acting nitrates Nitrates Nitrates are a class of medications that cause systemic vasodilation (veins > arteries) by smooth muscle relaxation. Nitrates are primarily indicated for the treatment of angina, where preferential venodilation causes pooling of blood, decreased preload, and ultimately decreased myocardial O2 demand. Nitrates taken regularly once or twice daily.
- Beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers): work by lowering myocardial oxygen demand Myocardial oxygen demand Stable and Unstable Angina by reducing heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology and contractility. Therapy aims to relieve angina and ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage; beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) also reduce mortality Mortality All deaths reported in a given population. Measures of Health Status and re-infarction rates after MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction.
- Calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel antagonists: also lower myocardial oxygen demand Myocardial oxygen demand Stable and Unstable Angina; they reduce blood pressure and decrease contractility.
Coronary Revascularization Revascularization Thromboangiitis Obliterans (Buerger’s Disease)

A coronary angiogram is pictured in this photo, with the outline of the major coronary arteries filled with radiopaque dye. Note the left main coronary artery, the LAD, and its branches.
Image: “Coronary angiogram showing coronary circulation” by Bleiglass. License: CC BY-SA 3.0It is appropriate to manage stable angina Stable angina Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia. Stable and Unstable Angina with medical therapy. [20] Percutaneous coronary intervention Percutaneous coronary intervention A family of percutaneous techniques that are used to manage coronary occlusion, including standard balloon angioplasty (percutaneous transluminal coronary angioplasty), the placement of intracoronary stents, and atheroablative technologies (e.g., atherectomy; endarterectomy; thrombectomy; percutaneous transluminal laser angioplasty). Ptca was the dominant form of pci, before the widespread use of stenting. Cardiac Surgery (PCI) or surgery should be considered in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with:
- Low exercise capacity or ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage at a low workload
- Large areas of affected myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy on imaging
- Impaired LV function with ejection fraction Ejection fraction Cardiac Cycle <40%
PCI is mainly used in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with single-vessel or 2-vessel disease with suitable anatomy, and coronary artery Coronary Artery Truncus Arteriosus bypass graft Graft A piece of living tissue that is surgically transplanted Organ Transplantation ( CABG CABG Surgical therapy of ischemic coronary artery disease achieved by grafting a section of saphenous vein, internal mammary artery, or other substitute between the aorta and the obstructed coronary artery distal to the obstructive lesion. Cardiac Surgery) surgery is more often used in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with 3-vessel or left main coronary disease.[21]
Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas
Several prognostic indicators determine the outcome of CHD:
- LV function: Increased left ventricular end-diastolic pressure Left ventricular end-diastolic pressure Cardiac Mechanics, increased ventricular volume, and reduced ejection fraction Ejection fraction Cardiac Cycle are associated with a poor prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas.
- Location and severity of coronary artery Coronary Artery Truncus Arteriosus stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS): Stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) of the left anterior descending (LAD) artery (“the widow-maker”) is associated with greater risk and poor prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas.
- Number and severity of risk factors: patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with multiple risk factors for atherosclerotic cardiovascular disease (ASCVD) are associated with an increased risk of myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction with a worse prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas.
- The annual mortality Mortality All deaths reported in a given population. Measures of Health Status rate in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with stable ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease has improved with medical treatments; the 1-year rate of cardiovascular death is 1.9%, with an all-cause mortality Mortality All deaths reported in a given population. Measures of Health Status rate of 2.9%.[22]
Vasospastic Angina
Definition
Vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina is characterized by sudden-onset coronary artery Coronary Artery Truncus Arteriosus spasm that leads to a reduction in coronary blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure, causing chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways without exertion that lasts less than 15–30 minutes. Formerly called Prinzmetal’s angina or variant angina Variant angina Vasospastic angina, also known as prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina, vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina is promptly relieved by short-acting nitrates Nitrates Nitrates are a class of medications that cause systemic vasodilation (veins > arteries) by smooth muscle relaxation. Nitrates are primarily indicated for the treatment of angina, where preferential venodilation causes pooling of blood, decreased preload, and ultimately decreased myocardial O2 demand. Nitrates even in the absence of underlying CAD. Myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease causing ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) changes in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina is due to transient vasospasm with or without underlying CAD.
Epidemiology
Vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina is an uncommon cause of myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease, responsible for approximately 5% of angina cases. [23] Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are generally younger (< age 50) than those with stable or unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina secondary to coronary artery Coronary Artery Truncus Arteriosus atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis. This syndrome has a higher incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency in Japan compared to Western countries, with a higher prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency in women. The overall incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency has decreased significantly over the past 30 years, possibly due to the increased use of calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blockers to treat hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension.
Etiology
Coronary vasospasm Coronary vasospasm Spasm of the large- or medium-sized coronary arteries. Vasospastic Angina can be associated with risk factors such as stress, smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, cocaine Cocaine An alkaloid ester extracted from the leaves of plants including coca. It is a local anesthetic and vasoconstrictor and is clinically used for that purpose, particularly in the eye, ear, nose, and throat. It also has powerful central nervous system effects similar to the amphetamines and is a drug of abuse. Cocaine, like amphetamines, acts by multiple mechanisms on brain catecholaminergic neurons; the mechanism of its reinforcing effects is thought to involve inhibition of dopamine uptake. Local Anesthetics or amphetamine use, nitrate withdrawal, and vasoconstrictor medications such as triptans Triptans Triptans and ergot alkaloids are agents used mainly for the management of acute migraines. The therapeutic effect is induced by binding to serotonin receptors, which causes reduced vasoactive neuropeptide release, pain conduction, and intracranial vasoconstriction. Triptans and Ergot Alkaloids. Rarely, coronary artery Coronary Artery Truncus Arteriosus vasospasm may be triggered after CABG CABG Surgical therapy of ischemic coronary artery disease achieved by grafting a section of saphenous vein, internal mammary artery, or other substitute between the aorta and the obstructed coronary artery distal to the obstructive lesion. Cardiac Surgery surgery or near a stent.[24] Generally, the specific trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation is unknown. Many patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship don’t display the classical coronary risk factors except for smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases. Vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina (VSA) is associated with systemic vasomotor disorders such as migraine Migraine Migraine headache is a primary headache disorder and is among the most prevalent disorders in the world. Migraine is characterized by episodic, moderate to severe headaches that may be associated with increased sensitivity to light and sound, as well as nausea and/or vomiting. Migraine Headache and Raynaud phenomenon, which suggests it may be part of a more generalized vascular disorder.
Pathophysiology
The underlying mechanism of VSA is unclear, and many theories have been put forward in recent years. Vasospasm occurs in response to local vasoconstrictor stimuli in the coronary segment. Impaired regulation of myofibril contraction in smooth muscle cells of coronary vessels causes smooth muscle hyperactivity Hyperactivity Attention Deficit Hyperactivity Disorder, resulting in vasospasm. Abnormalities of the endothelium Endothelium A layer of epithelium that lines the heart, blood vessels (vascular endothelium), lymph vessels (lymphatic endothelium), and the serous cavities of the body. Arteries: Histology, such as a defect in nitric oxide Nitric Oxide A free radical gas produced endogenously by a variety of mammalian cells, synthesized from arginine by nitric oxide synthase. Nitric oxide is one of the endothelium-dependent relaxing factors released by the vascular endothelium and mediates vasodilation. It also inhibits platelet aggregation, induces disaggregation of aggregated platelets, and inhibits platelet adhesion to the vascular endothelium. Nitric oxide activates cytosolic guanylate cyclase and thus elevates intracellular levels of cyclic gmp. Pulmonary Hypertension Drugs synthase (NOS), can lead to reduced nitric oxide Nitric Oxide A free radical gas produced endogenously by a variety of mammalian cells, synthesized from arginine by nitric oxide synthase. Nitric oxide is one of the endothelium-dependent relaxing factors released by the vascular endothelium and mediates vasodilation. It also inhibits platelet aggregation, induces disaggregation of aggregated platelets, and inhibits platelet adhesion to the vascular endothelium. Nitric oxide activates cytosolic guanylate cyclase and thus elevates intracellular levels of cyclic gmp. Pulmonary Hypertension Drugs levels, a natural vasodilator. Coronary artery Coronary Artery Truncus Arteriosus vasospasm can result from impairment of K+ ATP-dependent channels Channels The Cell: Cell Membrane and hyperactivity Hyperactivity Attention Deficit Hyperactivity Disorder of an intracellular enzyme rho-kinase. Sudden vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure from any of these mechanisms leads to decreased coronary blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure, causing myocardial hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage and angina. Other factors have been suggested in the pathogenesis of coronary artery Coronary Artery Truncus Arteriosus spasm, including autonomic nervous system Autonomic nervous system The ANS is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ANS consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy dysfunction, magnesium deficiency Magnesium Deficiency A nutritional condition produced by a deficiency of magnesium in the diet, characterized by anorexia, nausea, vomiting, lethargy, and weakness. Symptoms are paresthesias, muscle cramps, irritability, decreased attention span, and mental confusion, possibly requiring months to appear. Deficiency of body magnesium can exist even when serum values are normal. In addition, magnesium deficiency may be organ-selective, since certain tissues become deficient before others. Electrolytes, chronic low-grade inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, and increased oxidative stress Oxidative stress A disturbance in the prooxidant-antioxidant balance in favor of the former, leading to potential damage. Indicators of oxidative stress include damaged DNA bases, protein oxidation products, and lipid peroxidation products. Cell Injury and Death. Genetic factors may be involved, as there is a 3-fold greater incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency in Japanese people. [25] It is possible that certain genetic mutations Genetic Mutations Carcinogenesis predispose to coronary artery Coronary Artery Truncus Arteriosus spasm, such as those affecting the endothelial NOS gene Gene A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. Basic Terms of Genetics.
Clinical Features: Symptoms of Vasospastic Angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship experience very severe central chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, the same type of pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways as classic angina. These attacks tend to happen at rest or during regular Regular Insulin activity. Some patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may also experience these attacks during or after exercise, especially with coexisting fixed coronary artery Coronary Artery Truncus Arteriosus stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS). Other symptoms include shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea and palpitations Palpitations Ebstein’s Anomaly. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically experience angina attacks in clusters, more often from midnight to early morning.
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with variant coronary syndrome often have asymptomatic ischemic episodes. If coronary artery Coronary Artery Truncus Arteriosus spasm causes a prolonged disturbance in coronary blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure, it can (uncommonly) lead to myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction even in the absence of underlying CAD.
Syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope may also occur if there are disturbances to the heart rhythm, such as asystole Asystole No discernible electrical activity, flatline on electrocardiogram (P waves and QRS complexes are not present). Cardiac Arrest, atrioventricular block Atrioventricular block Atrioventricular (AV) block is a bradyarrhythmia caused by delay, or interruption, in the electrical conduction between the atria and the ventricles. Atrioventricular block occurs due to either anatomic or functional impairment, and is classified into 3 types. Atrioventricular block (AV block), or ventricular tachyarrhythmias. Fatal arrhythmias may cause sudden cardiac death Sudden cardiac death Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest.
Diagnostics
Definitive
vasospastic angina
Vasospastic Angina
Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD).
Vasospastic Angina is diagnosed when chest
pain
Pain
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
Pain: Types and Pathways responds to
nitrates
Nitrates
Nitrates are a class of medications that cause systemic vasodilation (veins > arteries) by smooth muscle relaxation. Nitrates are primarily indicated for the treatment of angina, where preferential venodilation causes pooling of blood, decreased preload, and ultimately decreased myocardial O2 demand.
Nitrates, and there are transient ischemic
ECG
ECG
An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures.
Electrocardiogram (ECG) changes seen, or if coronary arteriography documents >90% spasmodic constriction during an anginal episode.
Suspected
vasospastic angina
Vasospastic Angina
Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD).
Vasospastic Angina is diagnosed if nitrate-responsive angina is present, but no definite
ECG
ECG
An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures.
Electrocardiogram (ECG) changes or coronary spasm can be documented.
Significant advancements have been made in understanding and managing coronary artery Coronary Artery Truncus Arteriosus disease (CAD) in the absence of significant arterial blockages. The 2019 scientific statement from the American Heart Association American Heart Association A voluntary organization concerned with the prevention and treatment of heart and vascular diseases. Heart Failure provides contemporary guidelines for diagnosing and managing myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction without obstructive coronary artery Coronary Artery Truncus Arteriosus disease, underscoring the importance of recognizing and treating non-obstructive mechanisms of myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease.[57]. Similarly, the 2020 guidelines by the European Society of Cardiology offer detailed strategies for the long-term management of chronic coronary syndromes, advocating for comprehensive diagnostic evaluations to assess coronary function and ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage.[58] Moreover, a 2021 article in the BMJ and a 2022 systematic review in the Journal of the American Heart Association American Heart Association A voluntary organization concerned with the prevention and treatment of heart and vascular diseases. Heart Failure highlight the prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency and clinical significance of coronary microvascular disease and vasospasm in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with nonobstructive CAD, emphasizing the need for specialized diagnostic approaches to accurately identify and manage these conditions.[59.60]
ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG)
Electrocardiography
Electrocardiography
Recording of the moment-to-moment electromotive forces of the heart as projected onto various sites on the body's surface, delineated as a scalar function of time. The recording is monitored by a tracing on slow moving chart paper or by observing it on a cardioscope, which is a cathode ray tube display.
Electrocardiogram (ECG) is one of the essential keys to diagnosing
vasospastic angina
Vasospastic Angina
Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD).
Vasospastic Angina.
ECG
ECG
An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures.
Electrocardiogram (ECG) changes demonstrate transient ST-segment elevation (≥ 0.1 mV), ST-segment depression (≥ 0.1 mV), and may also include a taller
T wave
T wave
Electrocardiogram (ECG) and negative U wave. These changes must be in at least two contiguous leads, be evident during the attack of chest
pain
Pain
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
Pain: Types and Pathways, and resolve when the
pain
Pain
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
Pain: Types and Pathways dissipates. An episode can often be induced by having the patient hyperventilate. Arrhythmias may occur during an episode of
variant angina
Variant angina
Vasospastic angina, also known as prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD).
Vasospastic Angina and manifest as ventricular
tachycardia
Tachycardia
Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia.
Sepsis in Children,
atrioventricular block
Atrioventricular block
Atrioventricular (AV) block is a bradyarrhythmia caused by delay, or interruption, in the electrical conduction between the atria and the ventricles. Atrioventricular block occurs due to either anatomic or functional impairment, and is classified into 3 types.
Atrioventricular block (AV block), or
bradyarrhythmias
Bradyarrhythmias
Bradyarrhythmia is a rhythm in which the heart rate is less than 60/min. Bradyarrhythmia can be physiologic, without symptoms or hemodynamic change. Pathologic bradyarrhythmia results in reduced cardiac output and hemodynamic instability causing syncope, dizziness, or dyspnea.
Bradyarrhythmias.
If silent episodes of coronary spasm or arrhythmias are suspected, then a 24-hour Holter ambulatory monitor can be done, which records rhythm changes during symptomatic episodes.
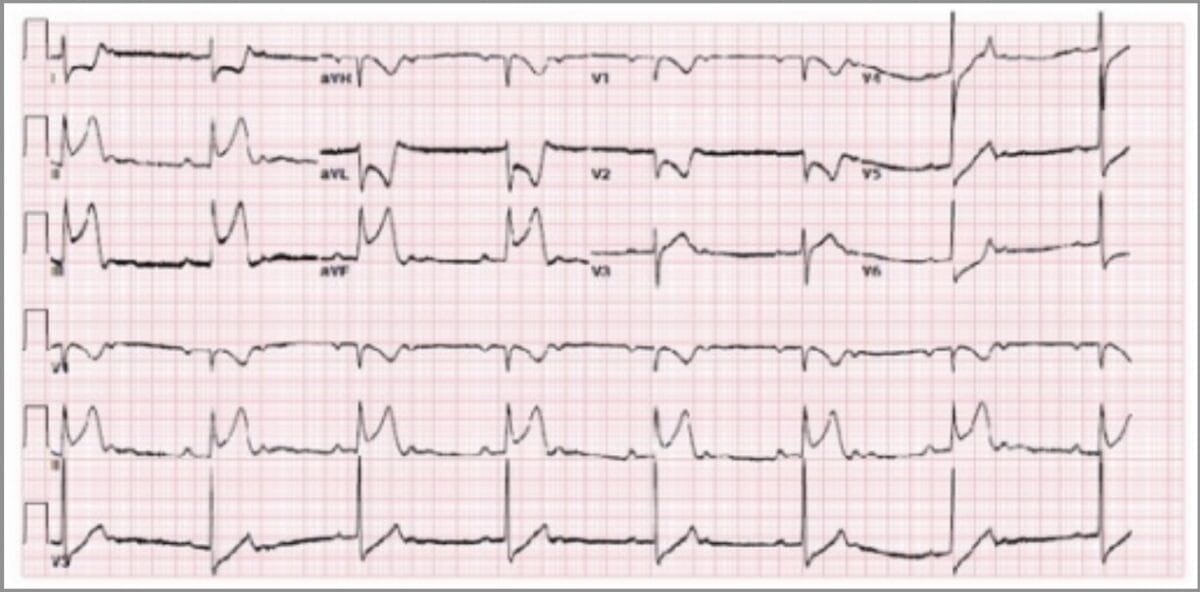
ECG recorded in a patient with an episode of variant angina showing 2:1 sinus bradycardia with a prolonged PR interval, significant ST elevation (5–6 mm) in the inferior leads, and anterior ST depression.
Image: “Prinzmetal Angina” by Beth Israel Medical Center, Albert Einstein College of Medicine, New York, NY, USA. License: CC BY 3.0Coronary Angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery
Diagnostic coronary arteriography is recommended if vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina is suspected by the history and ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) findings. It may either confirm the diagnosis or detect a high-grade fixed coronary obstruction.
Focal coronary artery Coronary Artery Truncus Arteriosus spasm significantly reduces the diameter of the lumen, causing temporary occlusion and myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease. Vasospasm can occur in normal-appearing arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology or arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology affected by atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis. The right coronary artery Right coronary artery Heart: Anatomy is most commonly affected; involvement of more than one artery is a negative prognostic factor. VSA is underdiagnosed, and documentation Documentation Systematic organization, storage, retrieval, and dissemination of specialized information, especially of a scientific or technical nature. It often involves authenticating or validating information. Advance Directives of myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease with a demonstration of coronary artery Coronary Artery Truncus Arteriosus spasm can be done with coronary angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery and a provocative stimulus such as acetylcholine Acetylcholine A neurotransmitter found at neuromuscular junctions, autonomic ganglia, parasympathetic effector junctions, a subset of sympathetic effector junctions, and at many sites in the central nervous system. Receptors and Neurotransmitters of the CNS or ergonovine.
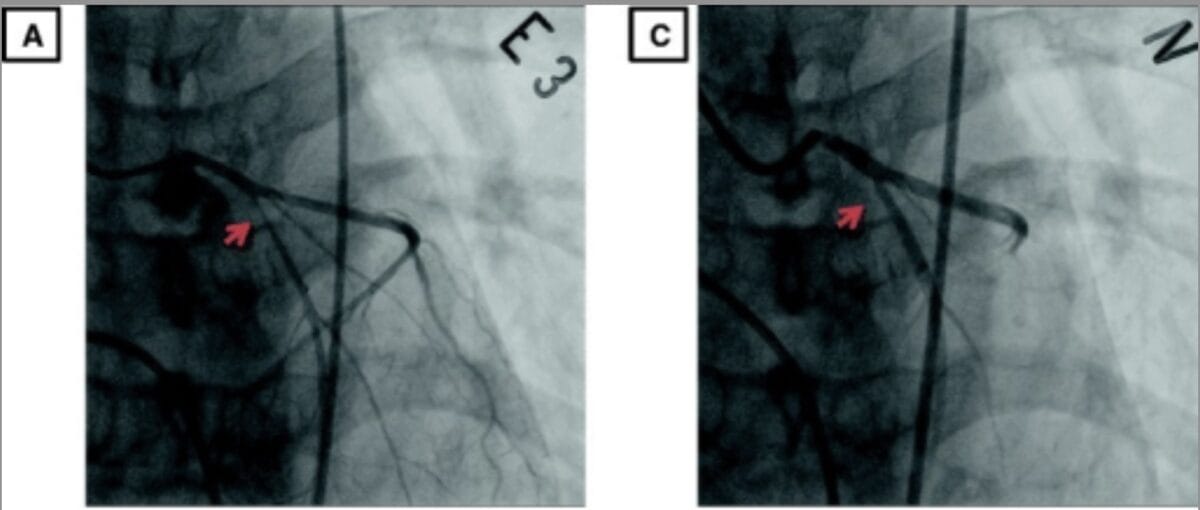
Coronary angiography in a patient with vasospastic angina. A: Coronary angiography demonstrates 95% stenosis in the proximal LAD artery (arrow in A) after administering intravenous ergonovine, which also provoked the patient’s typical chest pain; C: After injection of intracoronary nitroglycerin, the apparent stenosis completely resolved (arrow in C), thus documenting vasospasm.
Image: “Coronary angiography” by Division of Cardiology, Department of Internal Medicine, Sejong General Hospital & Sejong Heart Institute, Republic of Korea; cropped by Lecturio. License: CC BY 4.0Laboratory
With vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina, cardiac enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes are not elevated (troponins and CK-MB).
Exercise Testing
Stress testing with ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) monitoring has variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables results. ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) changes with exercise such as ST elevation or ST depression may point to fixed artery stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) or coronary artery Coronary Artery Truncus Arteriosus spasm.
Complications
Myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction and life-threatening arrhythmias include ventricular tachyarrhythmias or bradyarrhythmias Bradyarrhythmias Bradyarrhythmia is a rhythm in which the heart rate is less than 60/min. Bradyarrhythmia can be physiologic, without symptoms or hemodynamic change. Pathologic bradyarrhythmia results in reduced cardiac output and hemodynamic instability causing syncope, dizziness, or dyspnea. Bradyarrhythmias, sinus arrest Sinus arrest The omission of atrial activation that is caused by transient cessation of impulse generation at the sinoatrial node. It is characterized by a prolonged pause without P wave in an electrocardiogram. Sinus arrest has been associated with sleep apnea (rem sleep-related sinus arrest). Bradyarrhythmias, or even an AV block AV block Atrioventricular (AV) block is a bradyarrhythmia caused by delay, or interruption, in the electrical conduction between the atria and the ventricles. Atrioventricular block occurs due to either anatomic or functional impairment, and is classified into 3 types. Atrioventricular block (AV block) from a severe ischemic episode following vasospasm. Sudden cardiac arrest Cardiac arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest, with or without syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope, can occur due to ischemia-induced ventricular fibrillation Ventricular fibrillation Ventricular fibrillation (VF or V-fib) is a type of ventricular tachyarrhythmia (> 300/min) often preceded by ventricular tachycardia. In this arrhythmia, the ventricle beats rapidly and sporadically. The ventricular contraction is uncoordinated, leading to a decrease in cardiac output and immediate hemodynamic collapse. Ventricular Fibrillation (V-fib). Atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis can also occur later at the site of vasospasm, leading to local coronary thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus.
Treatment
Medical Treatment
Sublingual nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates is used for VSA attacks; calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blockers (CCB), such as diltiazem Diltiazem A benzothiazepine derivative with vasodilating action due to its antagonism of the actions of calcium ion on membrane functions. Class 4 Antiarrhythmic Drugs (Calcium Channel Blockers) or amlodipine Amlodipine A long-acting dihydropyridine calcium channel blocker. It is effective in the treatment of angina pectoris and hypertension. Hypertension Drugs, are effective in preventing ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage. Long-acting nitrates Nitrates Nitrates are a class of medications that cause systemic vasodilation (veins > arteries) by smooth muscle relaxation. Nitrates are primarily indicated for the treatment of angina, where preferential venodilation causes pooling of blood, decreased preload, and ultimately decreased myocardial O2 demand. Nitrates (e.g., isosorbide mononitrate Isosorbide Mononitrate Nitrates) can be added if a CCB is not sufficient to control the episodes. Documentation Documentation Systematic organization, storage, retrieval, and dissemination of specialized information, especially of a scientific or technical nature. It often involves authenticating or validating information. Advance Directives of suppression Suppression Defense Mechanisms of both symptomatic and more commonly occurring asymptomatic episodes by ambulatory electrocardiographic monitoring is needed. Regular Regular Insulin physical activity/exercise can also help treat VSA. [26]
An implantable cardioverter-defibrillator (ICD) is recommended for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with documented life-threatening ventricular arrhythmias.
Note: Drugs to avoid:
- Non-selective beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) (e.g., propranolol Propranolol A widely used non-cardioselective beta-adrenergic antagonist. Propranolol has been used for myocardial infarction; arrhythmia; angina pectoris; hypertension; hyperthyroidism; migraine; pheochromocytoma; and anxiety but adverse effects instigate replacement by newer drugs. Antiadrenergic Drugs) can worsen vasospasm
- Aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) at high doses because it inhibits prostacyclin Prostacyclin A prostaglandin that is a powerful vasodilator and inhibits platelet aggregation. It is biosynthesized enzymatically from prostaglandin endoperoxides in human vascular tissue. The sodium salt has been also used to treat primary pulmonary hypertension. Eicosanoids production, but low dose aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) is permitted
- Triptans Triptans Triptans and ergot alkaloids are agents used mainly for the management of acute migraines. The therapeutic effect is induced by binding to serotonin receptors, which causes reduced vasoactive neuropeptide release, pain conduction, and intracranial vasoconstriction. Triptans and Ergot Alkaloids used to treat acute migraines (e.g., sumatriptan Sumatriptan A serotonin agonist that acts selectively at 5ht1 receptors. It is used in the treatment of migraine disorders. Triptans and Ergot Alkaloids)
- Fluorouracil Fluorouracil A pyrimidine analog that is an antineoplastic antimetabolite. It interferes with DNA synthesis by blocking the thymidylate synthetase conversion of deoxyuridylic acid to thymidylic acid. Bowen Disease and Erythroplasia of Queyrat ( 5-fluorouracil 5-Fluorouracil A pyrimidine analog that is an antineoplastic antimetabolite. It interferes with DNA synthesis by blocking the thymidylate synthetase conversion of deoxyuridylic acid to thymidylic acid. Antimetabolite Chemotherapy) may cause coronary artery Coronary Artery Truncus Arteriosus spasm.
Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas
Myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction and life-threatening arrhythmias occur in approximately 25% of untreated patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.[27] Therapy appears to decrease the frequency of life-threatening events. If the condition is controlled early on, it can have a favorable prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas. Complications, such as acute myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction and cardiac death, typically occur early on after the onset of angina. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who have coronary spasm in multiple arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology are prone to having fatal arrhythmias. Individuals who do not have coexisting coronary artery Coronary Artery Truncus Arteriosus stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) generally have a more benign Benign Fibroadenoma prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas and better survival than those with severely diseased arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology and coronary artery Coronary Artery Truncus Arteriosus vasospasm. [28]
Review Questions
- An 18-year-old man presents to the emergency department with
severe chest pain
Severe Chest Pain
Flail Chest radiating to the back. ST-elevation is seen on the
ECG
ECG
An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures.
Electrocardiogram (ECG), but his cardiac
enzymes
Enzymes
Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules.
Basics of Enzymes are normal. A
coronary artery
Coronary Artery
Truncus Arteriosus catheterization reveals a normal study. What is the most likely diagnosis?
- Stable angina Stable angina Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia. Stable and Unstable Angina
- Unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina
- Ludwig angina
- Vasospastic angina Vasospastic Angina Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD). Vasospastic Angina
- Vincent angina
- A 35-year-old Japanese woman comes to the clinic complaining of chest
pain
Pain
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
Pain: Types and Pathways. For the last three years, she has had intermittent chest
pain
Pain
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
Pain: Types and Pathways, mostly at night, that lasts up to 10 minutes. It awakens her from sleep and is associated with
nausea
Nausea
An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses.
Antiemetics and sweating. An electrocardiogram is unremarkable. What would be the most likely finding on a Holter monitor during an episode of chest
pain
Pain
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
Pain: Types and Pathways?
- Normal ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG)
- PR segment depression in most leads
- Prolonged QT interval QT interval Electrocardiogram (ECG)
- Transient ST-segment elevation in the inferior leads
- Bradycardia Bradycardia Bradyarrhythmia is a rhythm in which the heart rate is less than 60/min. Bradyarrhythmia can be physiologic, without symptoms or hemodynamic change. Pathologic bradyarrhythmia results in reduced cardiac output and hemodynamic instability causing syncope, dizziness, or dyspnea. Bradyarrhythmias with no other ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) changes
- A 56-year-old man who has been diagnosed with
vasospastic angina
Vasospastic Angina
Vasospastic angina, also known as Prinzmetal or variant angina, is an uncommon cause of chest pain due to transient coronary artery spasms. The pathophysiology is distinguished from stable or unstable angina secondary to atherosclerotic coronary artery disease (CAD).
Vasospastic Angina comes to the emergency department with an acute episode of chest
pain
Pain
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
Pain: Types and Pathways. Which of the following would be the initial drug of choice for this patient?
- Nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates patch Patch Nonpalpable lesion > 1 cm in diameter Generalized and Localized Rashes
- Sublingual nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates
- Oral nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates
- Verapamil Verapamil A calcium channel blocker that is a class IV anti-arrhythmia agent. Pulmonary Hypertension Drugs
- Amlodipine Amlodipine A long-acting dihydropyridine calcium channel blocker. It is effective in the treatment of angina pectoris and hypertension. Hypertension Drugs
Answers: 1-4, 2-4, 3-2
Acute Coronary Syndrome (ACS)
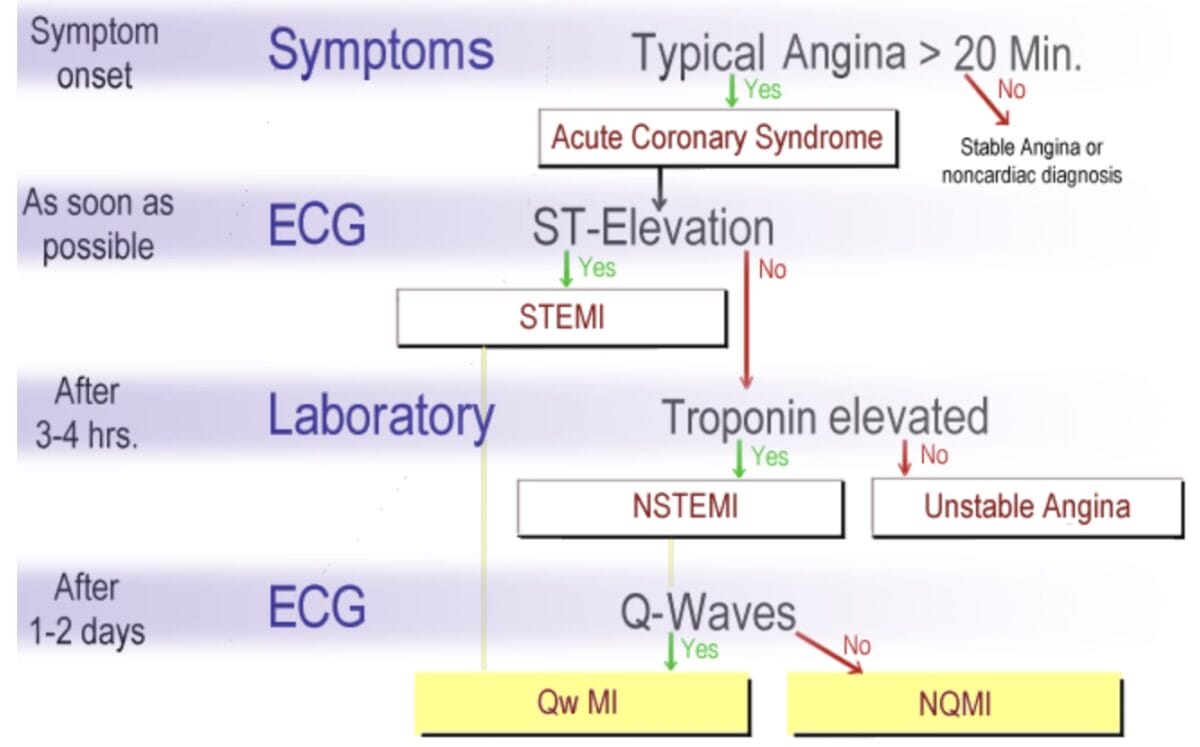
Simple diagram delineating the differences in the clinical presentation and classification of ACS. Patients with symptoms of ACS require an ECG and labs drawn for troponin levels within 10 minutes of presentation in an emergency department, and if normal, repeat troponin levels in 2 to 3 hours to assess for changes consistent with NSTEMI.
Image: “Abbreviations used for ACS” by J. Heuser. License: CC BY-SA 3.0Definition
The term acute coronary syndrome (ACS) refers to patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with suspicion or confirmation of acute myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease or infarction, associated with symptoms of chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways or pressure, with or without dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, and diaphoresis. The three types of ACS are non-ST-elevation myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (NSTEMI), ST-elevation MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (STEMI), and unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina (UA).
The Joint Task Force of the European Society of Cardiology, American College of Cardiology Foundation, the American Heart Association American Heart Association A voluntary organization concerned with the prevention and treatment of heart and vascular diseases. Heart Failure, and the World Heart Federation (ESC/ACCF/AHA/WHF) defined acute MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction in 2018 as the presence of acute myocardial injury detected by abnormal cardiac biomarkers in the setting of evidence of acute myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease. [2]
The definition of MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction was further refined by developing a clinical classification according to the assumed proximate cause of the myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease:
- Type 1 Type 1 Spinal Muscular Atrophy: an MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction caused by acute atherothrombotic CAD, usually precipitated by plaque Plaque Primary Skin Lesions disruption
- Type 2: an MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction consequent to increased oxygen demand or decreased supply, including that due to coronary dissection, vasospasm, emboli, microvascular dysfunction. Many of these patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship have CAD that will modulate the ischemic threshold Threshold Minimum voltage necessary to generate an action potential (an all-or-none response) Skeletal Muscle Contraction and depends on the severity of any given stressor that might cause ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage [29] This type also includes supply/demand mismatches without underlying CAD such as seen with arrhythmias, anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types, or severe hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension. [2, 30]
- Type 3 Type 3 Spinal Muscular Atrophy: Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with a typical presentation of myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease/infarction (symptoms and ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) changes) who died before blood for biomarkers could be drawn or before their appearance in the blood.
- Type 4a: an MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction associated with percutaneous coronary intervention Percutaneous coronary intervention A family of percutaneous techniques that are used to manage coronary occlusion, including standard balloon angioplasty (percutaneous transluminal coronary angioplasty), the placement of intracoronary stents, and atheroablative technologies (e.g., atherectomy; endarterectomy; thrombectomy; percutaneous transluminal laser angioplasty). Ptca was the dominant form of pci, before the widespread use of stenting. Cardiac Surgery (PCI) or from procedure-related complications associated with decreased coronary blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure.
- Type 4b: an intervention-related MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction with stent/scaffold thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus
- Type 5: an MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction associated with coronary artery Coronary Artery Truncus Arteriosus bypass graft Graft A piece of living tissue that is surgically transplanted Organ Transplantation surgery ( CABG CABG Surgical therapy of ischemic coronary artery disease achieved by grafting a section of saphenous vein, internal mammary artery, or other substitute between the aorta and the obstructed coronary artery distal to the obstructive lesion. Cardiac Surgery)
| Diagnosis | Clinical features | ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) findings | Laboratory findings |
| Unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina | Ischemic chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways that occurs at rest or with previously tolerated levels of exertion | None, or ST-segment depressions | None |
| Non-ST-elevation myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (NSTEMI) | Ischemic chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in any setting | None or ST-segment depressions | Elevated troponin |
| ST-elevation myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (STEMI) | Ischemic chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in any setting | ST-segment elevations | Elevated troponin |
Note: It is difficult to distinguish between ACS entities based on clinical symptoms alone.
Epidemiology
ACS is a subcategory of ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease, the leading cause of death worldwide.
- Mean age at onset: 68
- Male to female ratio: 3:2
- 70% of ACSs are NSTEMIs
Etiology
The most common cause of acute coronary syndromes is an acute thrombus in an atherosclerotic coronary artery Coronary Artery Truncus Arteriosus, with infrequent causes being cocaine Cocaine An alkaloid ester extracted from the leaves of plants including coca. It is a local anesthetic and vasoconstrictor and is clinically used for that purpose, particularly in the eye, ear, nose, and throat. It also has powerful central nervous system effects similar to the amphetamines and is a drug of abuse. Cocaine, like amphetamines, acts by multiple mechanisms on brain catecholaminergic neurons; the mechanism of its reinforcing effects is thought to involve inhibition of dopamine uptake. Local Anesthetics use, coronary spasm, and coronary artery Coronary Artery Truncus Arteriosus dissection. Endocarditis Endocarditis Endocarditis is an inflammatory disease involving the inner lining (endometrium) of the heart, most commonly affecting the cardiac valves. Both infectious and noninfectious etiologies lead to vegetations on the valve leaflets. Patients may present with nonspecific symptoms such as fever and fatigue. Endocarditis, vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus, or emboli from heart valve prostheses are rare causes.[31,32]
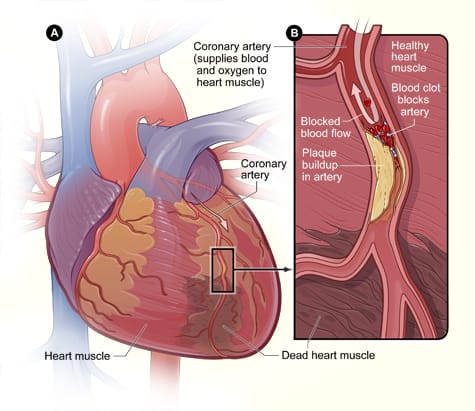
Heart showing irregular dark brown area indicating irreversibly damaged (dead/necrotic) muscle caused by acute myocardial infarction. Figure B is a longitudinal cross-section of the coronary artery with plaque buildup and an occlusive thrombus (blood clot) resulting from plaque rupture.
Image: “Hdw heartattack” by National Heart Lung and Blood Institute (NIH). License: Public DomainPathology
The pathology of ACS can be traced back to ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage resulting from reduced coronary blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure leading to myocardial cell injury Cell injury The cell undergoes a variety of changes in response to injury, which may or may not lead to cell death. Injurious stimuli trigger the process of cellular adaptation, whereby cells respond to withstand the harmful changes in their environment. Overwhelmed adaptive mechanisms lead to cell injury. Mild stimuli produce reversible injury. If the stimulus is severe or persistent, injury becomes irreversible. Cell Injury and Death or death. After the initial lipid-laden atherosclerotic plaque Plaque Primary Skin Lesions rupture in a coronary artery Coronary Artery Truncus Arteriosus occurs, there is platelet aggregation Platelet aggregation The attachment of platelets to one another. This clumping together can be induced by a number of agents (e.g., thrombin; collagen) and is part of the mechanism leading to the formation of a thrombus. Hemostasis, fibrin Fibrin A protein derived from fibrinogen in the presence of thrombin, which forms part of the blood clot. Rapidly Progressive Glomerulonephritis deposition, and thrombus formation. A complete vessel occlusion typically leads to ST-elevation myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (STEMI), causing irreversible tissue damage. Myocardial necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage begins after as little as 15 to 20 minutes of coronary occlusion. [33] After 6–12 hours, the damage can be seen by light microscopy in the form of loss of cross-striations and contraction bands. This is followed 24–72 hours later by pyknotic then lost nuclei, and heavy neutrophilic infiltrates. Grossly, the center of the infarct Infarct Area of necrotic cells in an organ, arising mainly from hypoxia and ischemia Ischemic Cell Damage is yellow-tan. At 3–7 days, dead myofibers are starting to be phagocytosed by macrophages Macrophages The relatively long-lived phagocytic cell of mammalian tissues that are derived from blood monocytes. Main types are peritoneal macrophages; alveolar macrophages; histiocytes; kupffer cells of the liver; and osteoclasts. They may further differentiate within chronic inflammatory lesions to epithelioid cells or may fuse to form foreign body giant cells or langhans giant cells. Innate Immunity: Phagocytes and Antigen Presentation at the infarct Infarct Area of necrotic cells in an organ, arising mainly from hypoxia and ischemia Ischemic Cell Damage borders. At 7–10 days, granulation Granulation Wound Healing tissue (new vessels and fibroblasts Fibroblasts Connective tissue cells which secrete an extracellular matrix rich in collagen and other macromolecules. Sarcoidosis) is seen at the margins. At 10–14 days, there is well-established (“organizing”) granulation Granulation Wound Healing tissue with prominent new blood vessels and collagen Collagen A polypeptide substance comprising about one third of the total protein in mammalian organisms. It is the main constituent of skin; connective tissue; and the organic substance of bones (bone and bones) and teeth (tooth). Connective Tissue: Histology deposition. Between 2 and 8 weeks, there is decreased cellularity, and collagen Collagen A polypeptide substance comprising about one third of the total protein in mammalian organisms. It is the main constituent of skin; connective tissue; and the organic substance of bones (bone and bones) and teeth (tooth). Connective Tissue: Histology deposition continues. After 2 months, a dense collagenous scar Scar Dermatologic Examination is formed.
Images showing the temporal evolution of pathological changes in STEMI are shown below.
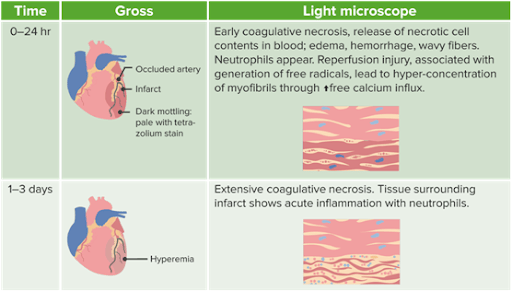
Location of Infarct: Infarcts can be classified as transmural or non-transmural depending upon the extent of heart wall involvement.
Image by Lecturio.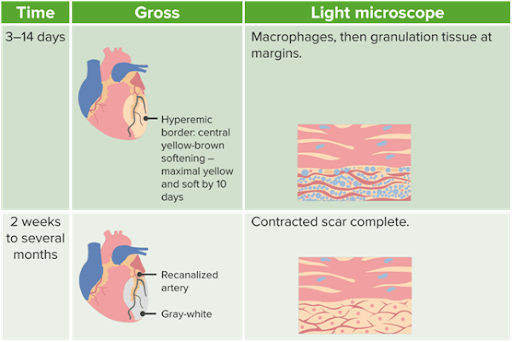
Location of Infarct: Infarcts can be classified as transmural or non-transmural depending upon the extent of heart wall involvement.
Image by Lecturio.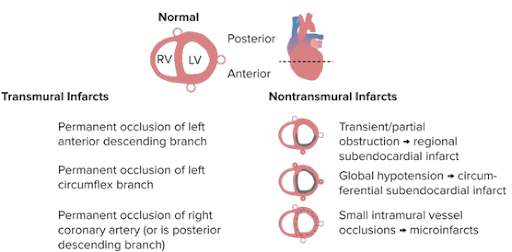
This drawing shows the different types and vessels involved in myocardial infarctions. Transmural infarcts, or STEMIs, can be due to complete occlusions of the LAD artery, left circumflex branch, or right coronary artery. The location of the affected artery corresponds with changes in the anterior, lateral, or posterior leads on ECG. Nontransmural infarcts are also called subendocardial MIs or NSTEMIs. These have less extensive ECG changes, and in addition to being caused by partial occlusion of the major coronary arteries, NSTEMIs can be seen with global hypotension and small-vessel occlusion.
Image by Lecturio.Clinical Features
There is often sudden, severe, substernal chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, typically radiating into the left shoulder and left arm Arm The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy. It can also radiate to the jaw Jaw The jaw is made up of the mandible, which comprises the lower jaw, and the maxilla, which comprises the upper jaw. The mandible articulates with the temporal bone via the temporomandibular joint (TMJ). The 4 muscles of mastication produce the movements of the TMJ to ensure the efficient chewing of food. Jaw and Temporomandibular Joint: Anatomy, teeth Teeth Normally, an adult has 32 teeth: 16 maxillary and 16 mandibular. These teeth are divided into 4 quadrants with 8 teeth each. Each quadrant consists of 2 incisors (dentes incisivi), 1 canine (dens caninus), 2 premolars (dentes premolares), and 3 molars (dentes molares). Teeth are composed of enamel, dentin, and dental cement. Teeth: Anatomy, or the right side of the body. Pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ACS often occurs without previous exertion, improves only slightly or not at all with nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates or rest, and lasts longer than 15 minutes.
The pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be described as an unbearable, cramp-like tightness in the chest. In addition, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, sense of impending doom, weakness, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, and diaphoresis are typical. Radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma into the upper abdomen, spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy, or neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess can also occur. A drop in blood pressure and tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, accompanied by cold sweating, can be signs of early cardiogenic shock Cardiogenic shock Shock resulting from diminution of cardiac output in heart disease. Types of Shock. Infarcts often happen during the early hours of the morning. [32] History should include contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation to thrombolytic therapy.
Silent myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease (or silent infarctions) especially affect diabetic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with neuropathy Neuropathy Leprosy. In these patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, about 85% of ischemic episodes occur without chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, suggesting that clinical angina only represents a small fraction of actual ischemic events. Medications that reduce anginal chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways also reduce episodes of silent ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage. [34]
Infarction pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can also be atypical, manifesting as upper abdominal pain Abdominal Pain Acute Abdomen, feeling of faintness combined with vagal symptoms such as sweating, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, or vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia. These painless or atypical presentations occur in about one-third of all cases. [35]
Physical examination may occasionally show evidence of LV dysfunction such as basilar rales Rales Respiratory Syncytial Virus, an S3 S3 Heart Sounds or S4 gallop S4 gallop Heart Sounds, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, or peripheral hypoperfusion in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with UA or NSTEMI. The exam is also important to exclude other potential causes of the patient’s symptoms, both cardiac and noncardiac.
Diagnostics
In addition to the medical history and physical examination, a 12-lead ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) and lab testing for the cardiac biomarker troponin are essential.
Accurate and timely diagnosis of acute MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction due to thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus is crucial, as management includes antithrombotic medications and possibly PCI. Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will have acute obstructive atherosclerotic coronary artery Coronary Artery Truncus Arteriosus stenoses with acute thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus ( type 1 Type 1 Spinal Muscular Atrophy MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction). However, some patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways who meet the diagnostic criteria for acute MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction based on the finding of an elevated troponin may not have an acute thrombotic event ( type 2 MI Type 2 MI Increased oxygen demand in the myocardium without adequate oxygen supply (whether or not there is underlying atherosclerotic CAD. Myocardial Infarction). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with myocardial injury unrelated to coronary artery Coronary Artery Truncus Arteriosus disease can present with myocarditis Myocarditis Myocarditis is an inflammatory disease of the myocardium, which may occur alone or in association with a systemic process. There are numerous etiologies of myocarditis, but all lead to inflammation and myocyte injury, most often leading to signs and symptoms of heart failure. Myocarditis, coronary artery Coronary Artery Truncus Arteriosus spasm, decreased oxygen supply due to severe tachyarrhythmias, or increased oxygen demand due to severe anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types. [30]
The differential diagnosis of chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways includes:
- Other cardiac conditions: aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a "false lumen." Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection, aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms, myocarditis Myocarditis Myocarditis is an inflammatory disease of the myocardium, which may occur alone or in association with a systemic process. There are numerous etiologies of myocarditis, but all lead to inflammation and myocyte injury, most often leading to signs and symptoms of heart failure. Myocarditis, stress cardiomyopathy Stress cardiomyopathy Takotsubo cardiomyopathy (also known as stress cardiomyopathy, or "broken heart syndrome") is a type of non-ischemic cardiomyopathy in which there is transient regional systolic dysfunction of the left ventricle. Patients present with symptoms of acute coronary syndrome, including chest pressure and shortness of breath. Takotsubo Cardiomyopathy (Takotsubo), pericarditis Pericarditis Pericarditis is an inflammation of the pericardium, often with fluid accumulation. It can be caused by infection (often viral), myocardial infarction, drugs, malignancies, metabolic disorders, autoimmune disorders, or trauma. Acute, subacute, and chronic forms exist. Pericarditis
- Pulmonary: Pulmonary embolism Pulmonary Embolism Pulmonary embolism (PE) is a potentially fatal condition that occurs as a result of intraluminal obstruction of the main pulmonary artery or its branches. The causative factors include thrombi, air, amniotic fluid, and fat. In PE, gas exchange is impaired due to the decreased return of deoxygenated blood to the lungs. Pulmonary Embolism, tension pneumothorax Tension Pneumothorax Pneumothorax, pleuritis Pleuritis Pleuritis, also known as pleurisy, is an inflammation of the visceral and parietal layers of the pleural membranes of the lungs. The condition can be primary or secondary and results in sudden, sharp, and intense chest pain on inhalation and exhalation. Pleuritis, pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia
- Gastrointestinal: Esophageal rupture Esophageal rupture Esophageal rupture or perforation is a transmural defect that occurs in the esophagus, exposing the mediastinum to GI content. The most common cause of esophageal perforation is iatrogenic trauma by instrumentation or surgical procedures. Esophageal Perforation, perforated peptic ulcer Peptic ulcer Peptic ulcer disease (PUD) refers to the full-thickness ulcerations of duodenal or gastric mucosa. The ulcerations form when exposure to acid and digestive enzymes overcomes mucosal defense mechanisms. The most common etiologies include Helicobacter pylori (H. pylori) infection and prolonged use of non-steroidal anti-inflammatory drugs (NSAIDs). Peptic Ulcer Disease, non-perforated peptic ulcer Peptic ulcer Peptic ulcer disease (PUD) refers to the full-thickness ulcerations of duodenal or gastric mucosa. The ulcerations form when exposure to acid and digestive enzymes overcomes mucosal defense mechanisms. The most common etiologies include Helicobacter pylori (H. pylori) infection and prolonged use of non-steroidal anti-inflammatory drugs (NSAIDs). Peptic Ulcer Disease, esophagitis Esophagitis Esophagitis is the inflammation or irritation of the esophagus. The major types of esophagitis are medication-induced, infectious, eosinophilic, corrosive, and acid reflux. Patients typically present with odynophagia, dysphagia, and retrosternal chest pain. Esophagitis, esophageal spasm, esophageal reflux, pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis, cholangitis, cholecystitis Cholecystitis Cholecystitis is the inflammation of the gallbladder (GB) usually caused by the obstruction of the cystic duct (acute cholecystitis). Mechanical irritation by gallstones can also produce chronic GB inflammation. Cholecystitis is one of the most common complications of cholelithiasis but inflammation without gallstones can occur in a minority of patients. Cholecystitis, choledocholithiasis Choledocholithiasis Presence or formation of gallstones in the common bile duct. Cholelithiasis, biliary colic
- Chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy: Costochondritis, rib fracture Rib fracture Fractures of any of the ribs. Thoracic Trauma in Children, cervical disc disease, herpes zoster Herpes Zoster Varicella-zoster virus (VZV) is a linear, double-stranded DNA virus in the Herpesviridae family. Shingles (also known as herpes zoster) is more common in adults and occurs due to the reactivation of VZV. Varicella-Zoster Virus/Chickenpox before the rash Rash Rocky Mountain Spotted Fever appears, neuropathic pain Neuropathic pain Caused by lesion or disease affecting the nervous system (PNS or CNS). Pain: Types and Pathways, fibromyalgia Fibromyalgia Fibromyalgia is a chronic pain syndrome characterized by widespread body pain, chronic fatigue, mood disturbance, and cognitive disturbance. It also presents with other comorbid symptoms such as migraine headaches, depression, sleep disturbance, and irritable bowel syndrome. Fibromyalgia
- Psychiatric: Anxiety Anxiety Feelings or emotions of dread, apprehension, and impending disaster but not disabling as with anxiety disorders. Generalized Anxiety Disorder disorders ( panic disorder Panic disorder Panic disorder is a condition marked by recurrent and episodic panic attacks that occur abruptly and without a trigger. These episodes are time-limited and present with cardiorespiratory (palpitations, shortness of breath, choking), GI (nausea, abdominal distress), and neurologic (paresthesias, lightheadedness) symptoms. Panic Disorder, hyperventilation Hyperventilation A pulmonary ventilation rate faster than is metabolically necessary for the exchange of gases. It is the result of an increased frequency of breathing, an increased tidal volume, or a combination of both. It causes an excess intake of oxygen and the blowing off of carbon dioxide. Respiratory Alkalosis), depression, somatic symptom disorder Somatic symptom disorder Somatic symptom disorder (SSD) is a condition characterized by the presence of 1 or more physical symptoms associated with excessive thoughts and feelings about symptom severity. Symptoms are usually not dangerous, but the patient devotes excessive time and energy to figuring out their underlying cause and how to treat them. Somatic Symptom Disorder
Laboratory Tests
Assessment of cardiac enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes is important to differentiate between the different entities of ACS. Various institutions use troponin I Troponin I A troponin complex subunit that inhibits actomyosin ATPase activity thereby disrupting actin and myosin interaction. There are three troponin I subtypes: troponin i1, i2 and i3. Troponin i3 is cardiac-specific whereas troponin i1 and i2 are skeletal subtypes. Troponin i3 is a biomarker for damaged or injured cardiac myocytes and mutations in troponin i3 gene are associated with familial hypertrophic cardiomyopathy. Myocardial Infarction or troponin T, which are specific and sensitive biomarkers of myocardial injury. HIgh-sensitivity troponin assays are available and use a sex-specific cutoff concentration [36]. CK-MB is used less often than in the past.
- Unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina (UA) is characterized by a lack of increase in troponin levels.
- NSTEMI and STEMI are characterized by the destruction of cardiac muscle Cardiac muscle The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Muscle Tissue: Histology tissue, resulting in elevated cardiac biomarkers.
Note: Even without an initial increase in troponin, an infarct Infarct Area of necrotic cells in an organ, arising mainly from hypoxia and ischemia Ischemic Cell Damage cannot immediately be excluded, and testing must be repeated in 2–3 hours.
Troponin levels provide information about the presence and extent of myocardial damage. The determination of troponin I Troponin I A troponin complex subunit that inhibits actomyosin ATPase activity thereby disrupting actin and myosin interaction. There are three troponin I subtypes: troponin i1, i2 and i3. Troponin i3 is cardiac-specific whereas troponin i1 and i2 are skeletal subtypes. Troponin i3 is a biomarker for damaged or injured cardiac myocytes and mutations in troponin i3 gene are associated with familial hypertrophic cardiomyopathy. Myocardial Infarction or T is considered the gold standard. It increases within 3 to 6 hours after the infarction. About 70% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship show an increase 3 hours after the incident, and that number rises to 90% six hours after the event. This timeline stresses the necessity to measure cardiac enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes again at a later time, even when the initial result was negative. Increased troponin levels on high-sensitivity assays confer an increased risk of adverse prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas. [37]
CK-MB is specific to myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction but does not start to rise until 4 hours after the occurrence of ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage. A CK-MB concentration of between 6–20% of the total CK indicates myocardial damage. Resampling of CK-MB levels can be used to detect early reinfarction because the initial levels would have returned to baseline 36 to 48 hours after infarction.
Troponin levels can also be used for detecting reinfarction. They should be measured immediately when reinfarction is suspected and repeated in 3 to 6 hours; a 20% increase in the second sample supports the diagnosis. [2]
Table of other biomarkers elevated in MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (in addition to troponin):
| Parameter | Beginning of increase | Maximum | Normal levels |
| Troponin | 3–8 hours | 12 hours | 1–2 weeks |
| CK-MB | 3–12 hours | 24 hours | 2–3 days |
| Myoglobin Myoglobin A conjugated protein which is the oxygen-transporting pigment of muscle. It is made up of one globin polypeptide chain and one heme group. Rhabdomyolysis | 1–4 hours | 4 hours | 1 day |
| LDH LDH Osteosarcoma | 6–12 hours | 2–4 days | 1–2 weeks |
| AST AST Enzymes of the transferase class that catalyze the conversion of l-aspartate and 2-ketoglutarate to oxaloacetate and l-glutamate. Liver Function Tests | 4 hours | 48 hours | 3–6 days |
ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) in UA and NSTEMI
- ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) can be normal with no specific changes, so a repeat ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) is needed every 15–30 minutes if suspicion of MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction is high or the patient continues to be symptomatic.
- In patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with NSTEMI, there is a less than total occlusion of a coronary artery Coronary Artery Truncus Arteriosus, causing a subendocardial MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (not through the entire heart muscle wall)
- ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) may show ST-segment depression or nonspecific T wave T wave Electrocardiogram (ECG) inversion (TWI), and by definition of an NSTEMI, there is no ST elevation
Echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA)
Echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA) is a valuable tool that can be used in the diagnostic workup of ACS. It provides direct visualization of the heart to assess:
- Site/size of segmental wall motion abnormalities
- LV systolic function
- Presence of complications ( aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms, valvular insufficiency, ventricular septal rupture Ventricular septal rupture Laceration or tearing of the ventricular septum, usually caused by myocardial infarction. Myocardial Infarction, and pericardial effusion Pericardial effusion Fluid accumulation within the pericardium. Serous effusions are associated with pericardial diseases. Hemopericardium is associated with trauma. Lipid-containing effusion (chylopericardium) results from leakage of thoracic duct. Severe cases can lead to cardiac tamponade. Pericardial Effusion and Cardiac Tamponade)
Coronary angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery
Coronary computed tomographic angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery ( CCTA CCTA Imaging of the Heart and Great Vessels) is a valuable noninvasive test for the assessment of coronary artery Coronary Artery Truncus Arteriosus disease (CAD) in selected patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with suspected coronary syndromes. It can determine the exact location and extent of coronary vessel stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) and guide further management, including the need for revascularization Revascularization Thromboangiitis Obliterans (Buerger’s Disease). It can also exclude the presence of CAD.[38]
Invasive coronary angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery should be performed in high-risk patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with spontaneous ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage despite appropriate medical therapy. This will help determine whether revascularization Revascularization Thromboangiitis Obliterans (Buerger’s Disease) is needed either by PCI or CABG CABG Surgical therapy of ischemic coronary artery disease achieved by grafting a section of saphenous vein, internal mammary artery, or other substitute between the aorta and the obstructed coronary artery distal to the obstructive lesion. Cardiac Surgery.[39]
Risk Assessment Risk assessment The qualitative or quantitative estimation of the likelihood of adverse effects that may result from exposure to specified health hazards or from the absence of beneficial influences. Preoperative Care
Initial evaluation of a patient with ACS must include an assessment of the risk of an acute cardiac ischemic event. Low-risk patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can be observed for several hours for repeat lab draws for troponin levels and repeat ECGs. If the findings of that brief evaluation are normal, the patient can have further testing as an outpatient. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are not low-risk should be hospitalized for further evaluation and treatment. [40]
Risk assessment Risk assessment The qualitative or quantitative estimation of the likelihood of adverse effects that may result from exposure to specified health hazards or from the absence of beneficial influences. Preoperative Care tools such as the Global Registry of Acute Coronary Events (GRACE) or Thrombolysis in Myocardial Infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (TIMI) algorithms take into account a patient’s risk variables that are predictive of major cardiac events (death, MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, or recurrent ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage).
Risk Factors
- Age > 65
- Three of more ASCVD risk factors ( hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, hyperlipidemia, family history Family History Adult Health Maintenance of CAD in a first-degree relative (< age 55 in men and < 65 in women)
- Known CAD or previous MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction
- Two or more episodes of anginal chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways at rest in the previous 24 hours
- Aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) use in the past 7 days
- ST-segment deviation
- Elevated troponin or CK-MB
Treatment of ACS: UA and NSTEMI
The initial treatment of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina (UA) or acute non-ST elevation myocardial infarction Non-ST elevation myocardial infarction A myocardial infarction that does not produce elevations in the ST segments of the electrocardiogram. ST segment elevation of the ECG is often used in determining the treatment protocol. Myocardial Infarction (NSTEMI) is similar to that used in an acute ST-elevation myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (STEMI) but without fibrinolysis. An elevation in biomarkers (troponin) may not be detectable for several hours after presentation. The treatment of UA and NSTEMI are similar; STEMI is discussed separately in the next section.
Many steps may be accomplished simultaneously by members of the emergency team. These include examination, lab draw (for troponin, CBC, chemistry panel, coagulation testing), establishing IV access, ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG), applying a cardiac monitor, and supplemental oxygen Supplemental Oxygen Respiratory Failure if O2 saturation <90% or if there is respiratory distress. Hyperoxia has a vasoconstrictor effect on the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology, and supplemental oxygen Supplemental Oxygen Respiratory Failure is no longer used in every patient with chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways.
Antianginal therapy with nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates is indicated for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and suspected ACS. Nitrates Nitrates Nitrates are a class of medications that cause systemic vasodilation (veins > arteries) by smooth muscle relaxation. Nitrates are primarily indicated for the treatment of angina, where preferential venodilation causes pooling of blood, decreased preload, and ultimately decreased myocardial O2 demand. Nitrates are venodilators at low doses and arteriolar dilators at higher doses; they may prevent recurrent ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina. Sublingual nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates is given every 5 minutes for 3 doses, unless there are contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation to nitrates Nitrates Nitrates are a class of medications that cause systemic vasodilation (veins > arteries) by smooth muscle relaxation. Nitrates are primarily indicated for the treatment of angina, where preferential venodilation causes pooling of blood, decreased preload, and ultimately decreased myocardial O2 demand. Nitrates. These include hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, severe aortic stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), hypertrophic cardiomyopathy Hypertrophic Cardiomyopathy Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiomyopathy, which is characterized by an asymmetric increase in thickness (hypertrophy) of the left ventricular wall, diastolic dysfunction, and often left ventricular outflow tract obstruction. Hypertrophic Cardiomyopathy, suspected right ventricular infarct Infarct Area of necrotic cells in an organ, arising mainly from hypoxia and ischemia Ischemic Cell Damage, marked bradycardia Bradycardia Bradyarrhythmia is a rhythm in which the heart rate is less than 60/min. Bradyarrhythmia can be physiologic, without symptoms or hemodynamic change. Pathologic bradyarrhythmia results in reduced cardiac output and hemodynamic instability causing syncope, dizziness, or dyspnea. Bradyarrhythmias or tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, or recent use of a phosphodiesterase 5 inhibitor (e.g., sildenafil Sildenafil A phosphodiesterase type-5 inhibitor; vasodilator agent and urological agent that is used in the treatment of erectile dysfunction and primary pulmonary hypertension. Phosphodiesterase Inhibitors). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ongoing or recurrent chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways should receive IV nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates titrated to symptom relief unless adverse effects develop. IV morphine Morphine The principal alkaloid in opium and the prototype opiate analgesic and narcotic. Morphine has widespread effects in the central nervous system and on smooth muscle. Opioid Analgesics is given for relief of severe chest pain Severe Chest Pain Flail Chest if not relieved.
Beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) diminish symptoms and the risk of MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ACS who are not already taking a beta-blocker. If there are no contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation (decompensated heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), advanced atrioventricular (AV) block, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension), oral or IV metoprolol Metoprolol A selective adrenergic beta-1 blocking agent that is commonly used to treat angina pectoris; hypertension; and cardiac arrhythmias. Antiadrenergic Drugs should be initiated.
Calcium-channel blockers Calcium-Channel Blockers A class of drugs that act by selective inhibition of calcium influx through cellular membranes. Heart Failure and Angina Medication cause arterial vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs, increase coronary artery Coronary Artery Truncus Arteriosus blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure, and decrease blood pressure. Oral diltiazem Diltiazem A benzothiazepine derivative with vasodilating action due to its antagonism of the actions of calcium ion on membrane functions. Class 4 Antiarrhythmic Drugs (Calcium Channel Blockers) is recommended for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation to beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers). Diltiazem Diltiazem A benzothiazepine derivative with vasodilating action due to its antagonism of the actions of calcium ion on membrane functions. Class 4 Antiarrhythmic Drugs (Calcium Channel Blockers) is contraindicated in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with LV systolic dysfunction Systolic dysfunction Dilated Cardiomyopathy or pulmonary vascular congestion.
Dual antiplatelet therapy ( aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) plus clopidogrel Clopidogrel A ticlopidine analog and platelet purinergic p2y receptor antagonist that inhibits adenosine diphosphate-mediated platelet aggregation. It is used to prevent thromboembolism in patients with arterial occlusive diseases; myocardial infarction; stroke; or atrial fibrillation. Antiplatelet Drugs or similar) should be given to patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ACS unless there are contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation such as aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction or active bleeding. [41]
Anticoagulation Anticoagulation Pulmonary Hypertension Drugs therapy should be administered to all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ACS unless contraindicated. Unfractionated IV heparin is given if a cardiac catheterization Cardiac Catheterization Procedures in which placement of cardiac catheters is performed for therapeutic or diagnostic procedures. Cardiac Surgery is planned; otherwise, low molecular weight heparins ( enoxaparin Enoxaparin Low-molecular-weight fragment of heparin, having a 4-enopyranosuronate sodium structure at the non-reducing end of the chain. It is prepared by depolymerization of the benzylic ester of porcine mucosal heparin. Therapeutically, it is used as an antithrombotic agent. Anticoagulants or dalteparin Dalteparin A low-molecular-weight fragment of heparin, prepared by nitrous acid depolymerization of porcine mucosal heparin. The mean molecular weight is 4000-6000 daltons. It is used therapeutically as an antithrombotic agent. Anticoagulants) or fondaparinux Fondaparinux Synthetic pentasaccharide that mediates the interaction of heparin with antithrombins and inhibits factor Xa; it is used for prevention of venous thromboembolism after surgery. Anticoagulants (a selective factor Xa inhibitor) are indicated. Bivalirudin Bivalirudin Anticoagulants is a direct thrombin inhibitor Direct Thrombin Inhibitor Anticoagulants that is recommended as an alternative anticoagulant for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship needing PCI. [42] Fibrinolytic therapy is not recommended for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with NSTEMI.
High-dose statin therapy is recommended in all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with UA/NSTEMI regardless of cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism levels unless contraindicated. These doses of statins Statins Statins are competitive inhibitors of HMG-CoA reductase in the liver. HMG-CoA reductase is the rate-limiting step in cholesterol synthesis. Inhibition results in lowered intrahepatocytic cholesterol formation, resulting in up-regulation of LDL receptors and, ultimately, lowering levels of serum LDL and triglycerides. Statins promote plaque Plaque Primary Skin Lesions stabilization and restore endothelial function, and reduction in ischemic events is not seen with lower doses. [43]
Some hospitals use ACE inhibitors ACE inhibitors Truncus Arteriosus for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with NSTEMI unless hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension is an issue in the first few hours; there is long-term benefit in MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, or stable chronic kidney disease Chronic Kidney Disease Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease. The evidence is more apparent in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with STEMI.[44]
Acute Myocardial Infarction: STEMI
Diagnosis: ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) in STEMI
Sequence of ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) changes in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with STEMI:
- A hyperacute T wave T wave Electrocardiogram (ECG) is often the first change. It is tall, peaked, and symmetric in at least two contiguous leads.
- Elevation of the J point and convex ST-segment elevation are the hallmarks of acute myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction.
- The ST-segment elevation becomes more prominent, and its form becomes convex or rounded upward.
- The ST segment ST segment Isoelectric segment between the s wave and the initial deflection of the t wave. Electrocardiogram (ECG) merges with the T wave T wave Electrocardiogram (ECG) in an “injury current” or so-called “tombstone” pattern. Reciprocal ST-segment depressions are usually observed in other leads.
- The ST-segment eventually returns to baseline, an initial Q wave develops, and R wave amplitude is lost. If ST-segment elevation lasts >3 weeks, suspect a ventricular aneurysm Ventricular aneurysm A localized bulging or dilatation in the muscle wall of a heart (myocardium), usually in the left ventricle. Blood-filled aneurysms are dangerous because they may burst. Fibrous aneurysms interfere with the heart function through the loss of contractility. True aneurysm is bound by the vessel wall or cardiac wall. False aneurysms are hematoma caused by myocardial rupture. Myocardial Infarction in the infarcted region.
- The T wave T wave Electrocardiogram (ECG) becomes inverted and may remain inverted or return upright.
- The R wave amplitude becomes markedly reduced, the Q wave deepens, and the T wave T wave Electrocardiogram (ECG) remains inverted or becomes positive. These usually occur within 2 weeks, but they can occur after several hours.
A left bundle branch block Left bundle branch block Bundle Branch and Fascicular Blocks ( LBBB LBBB Bundle Branch and Fascicular Blocks) often obscures ST-segment changes in acute STEMI; a new LBBB LBBB Bundle Branch and Fascicular Blocks is associated with high mortality Mortality All deaths reported in a given population. Measures of Health Status, and these patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship benefit significantly from reperfusion therapy. In the setting of LBBB LBBB Bundle Branch and Fascicular Blocks, Q waves in two of leads I, aVL, V5, and V6 or R wave regression Regression Corneal Abrasions, Erosion, and Ulcers from V1 to V4 suggest acute MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction.
Right bundle branch block Right bundle branch block Bundle Branch and Fascicular Blocks ( RBBB RBBB Bundle Branch and Fascicular Blocks) usually does not mask typical ST elevation except in rare cases of isolated true posterior MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, which has tall right precordial R waves and ST depression.
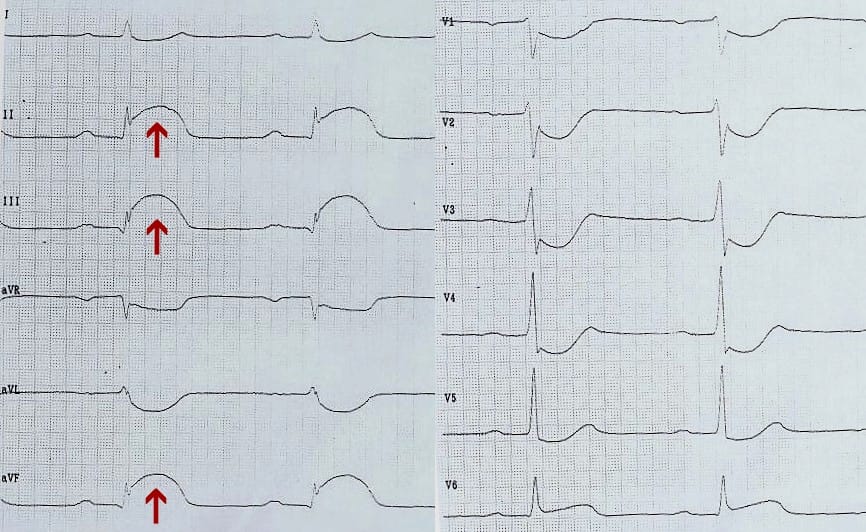
ECG in a patient with an ST-Elevation Myocardial Infarction (STEMI). Note the ST segment elevation with an injury current pattern in leads II, III, and aVF, consistent with an inferior wall MI, and reciprocal changes with ST depression in V4, V5, and aVL.
Image: “EKG eines akuten diaphragmalen Infarkts” by JHeuser. License: CC BY-SA 3.0Timing of ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) changes depending on the phase of the infarction:[33]
- Early acute phase Acute phase Short Bowel Syndrome: Begins within minutes, persists, and evolves over several hours after the infarction, typically characterized by pointed elevation of the T-wave, which is called a hyperacute T-wave (hyperacute pattern).
- Acute phase Acute phase Short Bowel Syndrome: ST segments evolve from concave to convex, and when blended with the injury pattern of blended ST-T waves, take on the “tombstone” appearance. Reciprocal changes occur (ST-segment depressions) in leads opposite those with ST elevations and are associated with larger areas of injury.
- Evolved acute phase Acute phase Short Bowel Syndrome: The ST-elevation and R-spike decrease, so-called “poor R-wave progression” occurs, and pathologic Q or QS waves develop.
- Chronic phase Chronic phase HIV Infection and AIDS: ST changes usually resolve completely in 2 weeks for inferior MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction and may take longer for large anterior MIs. Symmetrical Symmetrical Dermatologic Examination TWI can resolve within weeks to months or persist indefinitely. More than 6 months after the infarction, the changes of the QRS complex QRS complex Electrocardiogram (ECG) remain.
Localization of Infarction
The ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) leads depicting the characteristic ST changes in STEMIs provide information about which coronary artery Coronary Artery Truncus Arteriosus is most likely obstructed and the location of the infarction. They are less useful for localization in NSTEMIs.
| Localization of Infarction | ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) ST-segment elevation | |
| Extensive anterior MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (LAD artery) | I, aVL, V1-6 | |
| Anterior MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (LAD) | V1-6 | |
| Lateral MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (distal LAD or LCx) | I, aVL, V5-6 | |
| Anteroseptal MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (proximal LAD) | V1-V4 | |
| Inferior MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (RCA) | II, III, aVF | |
| Posterior MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction (left circumflex artery) | V7-9, inverse in V1-V2 | |
| Right ventricle (proximal RCA) | V4R to V6R | |
LAD: left anterior descending artery
LCx: left circumflex artery
RCA:
right coronary artery
Right coronary artery
Heart: Anatomy
Imaging
- Cardiac catheterization Cardiac Catheterization Procedures in which placement of cardiac catheters is performed for therapeutic or diagnostic procedures. Cardiac Surgery is considered the gold standard and should be performed as quickly as possible in the case of STEMI.
- Echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA) is a diagnostic tool that helps to detect wall motion abnormalities, determine LV function, and exclude complications, such as cardiac valvular defects.
- MRI cardioangiography may serve as another means of detecting wall motion abnormalities and determining the size of infarction scars.
Treatment of STEMI
Partial myocardial salvage can be achieved by reperfusion within 3 to 6 hours, and the longer the duration of ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, the lesser amount of salvageable tissue there will be.
Initial Management of Myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction
Testing for cardiac biomarkers and treatment with antianginal therapy, beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers), antiplatelet agents Antiplatelet agents Antiplatelet agents are medications that inhibit platelet aggregation, a critical step in the formation of the initial platelet plug. Abnormal, or inappropriate, platelet aggregation is a key step in the pathophysiology of arterial ischemic events. The primary categories of antiplatelet agents include aspirin, ADP inhibitors, phosphodiesterase/adenosine uptake inhibitors, and glycoprotein IIb/IIIa inhibitors. Antiplatelet Drugs, anticoagulants Anticoagulants Anticoagulants are drugs that retard or interrupt the coagulation cascade. The primary classes of available anticoagulants include heparins, vitamin K-dependent antagonists (e.g., warfarin), direct thrombin inhibitors, and factor Xa inhibitors. Anticoagulants, and statins Statins Statins are competitive inhibitors of HMG-CoA reductase in the liver. HMG-CoA reductase is the rate-limiting step in cholesterol synthesis. Inhibition results in lowered intrahepatocytic cholesterol formation, resulting in up-regulation of LDL receptors and, ultimately, lowering levels of serum LDL and triglycerides. Statins are the same as listed above for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with NSTEMI.
Reperfusion
For patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with STEMI, a method for coronary reperfusion is chosen based on the patient’s presentation and availability of the cardiac catheterization Cardiac Catheterization Procedures in which placement of cardiac catheters is performed for therapeutic or diagnostic procedures. Cardiac Surgery team. Reperfusion therapy with PCI (goal < 90 minutes from first medical contact) is optimal for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with STEMI and is the preferred approach for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship within 12 hours of the onset of symptoms and evidence of ongoing ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage. Primary PCI is much preferred to fibrinolysis. In some cases, it can be done up to 12 hours of symptom onset in high-risk patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship or with ongoing ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage.
PCI is highly effective, has little morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status, and patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship recover completely within a few hours. Its main disadvantage is restenosis (recurrence of arterial blockage), seen in 5 to 20% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.[21]
Reperfusion with surgical CABG CABG Surgical therapy of ischemic coronary artery disease achieved by grafting a section of saphenous vein, internal mammary artery, or other substitute between the aorta and the obstructed coronary artery distal to the obstructive lesion. Cardiac Surgery is recommended for left main coronary artery Coronary Artery Truncus Arteriosus disease, or if there is multiple-vessel disease involving the left anterior descending artery with LV dysfunction or diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus.
CABG CABG Surgical therapy of ischemic coronary artery disease achieved by grafting a section of saphenous vein, internal mammary artery, or other substitute between the aorta and the obstructed coronary artery distal to the obstructive lesion. Cardiac Surgery is performed using the internal thoracic artery or a reverse saphenous vein from the leg Leg The lower leg, or just "leg" in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy. One end of the bypass is attached to the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy and the other to the obstructed coronary artery Coronary Artery Truncus Arteriosus beyond the obstruction. Open chest surgery with general anesthesia General anesthesia Procedure in which patients are induced into an unconscious state through use of various medications so that they do not feel pain during surgery. Anesthesiology: History and Basic Concepts is required. The advantages of CABG CABG Surgical therapy of ischemic coronary artery disease achieved by grafting a section of saphenous vein, internal mammary artery, or other substitute between the aorta and the obstructed coronary artery distal to the obstructive lesion. Cardiac Surgery include its high effectiveness and the durability of the result. Its main disadvantage is the need for open-chest surgery, which results in increased procedural morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status, requires a 4 to 7-day hospital stay, and several weeks for a full recovery.
If PCI is not available within 120 minutes (including transfer time), then fibrinolysis is indicated in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with symptoms that have already lasted more than 2 to 3 hours if there are no absolute contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation. A regimen of a tissue plasminogen activator Tissue plasminogen activator A proteolytic enzyme in the serine protease family found in many tissues which converts plasminogen to fibrinolysin. It has fibrin-binding activity and is immunologically different from urokinase-type plasminogen activator. The primary sequence, composed of 527 amino acids, is identical in both the naturally occurring and synthetic proteases. Hemostasis (t-PA) plus IV heparin has better efficacy and lower mortality Mortality All deaths reported in a given population. Measures of Health Status than streptokinase Streptokinase Streptococcal fibrinolysin. An enzyme produced by hemolytic streptococci. It hydrolyzes amide linkages and serves as an activator of plasminogen. It is used in thrombolytic therapy and is used also in mixtures with streptodornase (streptodornase and streptokinase). Thrombolytics.[45] Longer-acting agents ( tenecteplase Tenecteplase A tissue plasminogen activator enzyme that acts as a fibrinolytic agent; it is used for the dissolution of blood clots, such as those that occur in acute myocardial infarction. Thrombolytics, reteplase Reteplase Thrombolytics) are now given more commonly than alteplase Alteplase Thrombolytics. Timing is critical, ideally less than 30 minutes from initial medical contact (ambulance or ED) to drug administration (“door-to-needle time”). It should be delivered <10 min of STEMI confirmation on the ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) (do not wait for troponin levels if the clinical presentation is typical). The benefit from thrombolytic therapy is maximal when given < 2 hours of symptom onset.
Among patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with STEMI who have undergone fibrinolysis, early recurrence of ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage by threatened reocclusion has been observed in 20 to 30% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, thrombotic coronary reocclusion in 5 to 15 %, and reinfarction in 3 to 5 % [46]. Reinfarction occurs at a median of 2 to 4 days after fibrinolytic therapy and is associated with increased mortality Mortality All deaths reported in a given population. Measures of Health Status.
Absolute Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation of Fibrinolytic Therapy
- Previous hemorrhagic stroke Hemorrhagic stroke Stroke due to rupture of a weakened blood vessel in the brain (e.g., cerebral hemispheres; cerebellum; subarachnoid space). Subarachnoid Hemorrhage at any time
- Ischemic stroke Ischemic Stroke An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke within 3 months
- Known intracranial neoplasm
- Closed head injury Closed Head Injury Subdural Hemorrhage within 3 months
- Active bleeding, or bleeding diathesis Bleeding diathesis Wiskott-Aldrich Syndrome
- Suspected aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a "false lumen." Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection
Relative Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation
- Severe uncontrolled hypertension Uncontrolled hypertension Although hypertension is defined as a blood pressure of > 130/80 mm Hg, individuals can present with comorbidities of severe asymptomatic or "uncontrolled" hypertension (≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic) that carries with it a significant risk of morbidity and mortality. Uncontrolled Hypertension > 180/110
- History of ischemic stroke Ischemic Stroke An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke > 3 months
- Prolonged CPR CPR The artificial substitution of heart and lung action as indicated for heart arrest resulting from electric shock, drowning, respiratory arrest, or other causes. The two major components of cardiopulmonary resuscitation are artificial ventilation and closed-chest cardiac massage. Cardiac Arrest > 10 minutes
- Major surgery < 3 weeks
- Recent (within 2–4 weeks) internal bleeding
Coronary Angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery after Fibrinolysis (Rescue PCI)
It is indicated in cases with:
- Failure of reperfusion evidenced by < 50% resolution of ST-segment elevation > 90 min after completion of fibrinolytic treatment
- Spontaneous recurrent ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage while in a hospital
- High-risk features: extensive ST-segment elevation, signs of heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), and hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension (systolic blood pressure < 100 mm Hg)
Complications of STEMIs
STEMI complications can be classified into early and late. Reinfarction, arrhythmias (both atrial and ventricular), and heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) can all occur shortly after MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction or a couple of weeks later. Within the first 18 hours of the initial MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, a recurrent elevation in cardiac biomarker levels alone should not be relied upon to diagnose reinfarction and requires recurrent ST-segment elevation on ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) and at least one other supporting criterion (e.g., chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, hemodynamic decompensation). For patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, more than 18 hours from the initial MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, a rise in troponin and at least one additional criterion are sufficient for the diagnosis of reinfarction.
Other early complications include sudden cardiac death Sudden cardiac death Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest ( SCD SCD Sickle cell disease (SCD) is a group of genetic disorders in which an abnormal Hb molecule (HbS) transforms RBCs into sickle-shaped cells, resulting in chronic anemia, vasoocclusive episodes, pain, and organ damage. Sickle Cell Disease), and potentially life-threatening AV block AV block Atrioventricular (AV) block is a bradyarrhythmia caused by delay, or interruption, in the electrical conduction between the atria and the ventricles. Atrioventricular block occurs due to either anatomic or functional impairment, and is classified into 3 types. Atrioventricular block (AV block) or ventricular tachyarrhythmias may happen in the first 24 hours. A few days after STEMI, patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can develop acute left heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) (HF) and pulmonary edema Pulmonary edema Pulmonary edema is a condition caused by excess fluid within the lung parenchyma and alveoli as a consequence of a disease process. Based on etiology, pulmonary edema is classified as cardiogenic or noncardiogenic. Patients may present with progressive dyspnea, orthopnea, cough, or respiratory failure. Pulmonary Edema resulting from acute pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols failure or acute mitral valve insufficiency Mitral valve insufficiency Mitral regurgitation (MR) is the backflow of blood from the left ventricle (LV) to the left atrium (LA) during systole. Mitral regurgitation may be acute (myocardial infarction) or chronic (myxomatous degeneration). Acute and decompensated chronic mr can lead to pulmonary venous congestion, resulting in symptoms of dyspnea, orthopnea, and fatigue. Mitral Regurgitation secondary to papillary muscle dysfunction. The most serious complication is cardiogenic shock Cardiogenic shock Shock resulting from diminution of cardiac output in heart disease. Types of Shock, associated with mortality Mortality All deaths reported in a given population. Measures of Health Status rates exceeding 50%.[47] In patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who have myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction with non-obstructive coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology, certain scoring systems may better predict outcomes, highlighting the need for tailored approaches in their clinical assessment and management. [61]
Late complications of STEMI include pericarditis Pericarditis Pericarditis is an inflammation of the pericardium, often with fluid accumulation. It can be caused by infection (often viral), myocardial infarction, drugs, malignancies, metabolic disorders, autoimmune disorders, or trauma. Acute, subacute, and chronic forms exist. Pericarditis, presenting either in the first week after an MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction or with Dressler syndrome Dressler syndrome Myocardial Infarction a couple of weeks later. Dressler syndrome Dressler syndrome Myocardial Infarction, also called “post-cardiac injury” syndrome is noninfectious pericarditis Pericarditis Pericarditis is an inflammation of the pericardium, often with fluid accumulation. It can be caused by infection (often viral), myocardial infarction, drugs, malignancies, metabolic disorders, autoimmune disorders, or trauma. Acute, subacute, and chronic forms exist. Pericarditis that occurs 2–20 weeks post-MI secondary to the deposition of anticardiac antibody immune complexes Immune complexes The complex formed by the binding of antigen and antibody molecules. The deposition of large antigen-antibody complexes leading to tissue damage causes immune complex diseases. C3 Deficiency in the pericardium Pericardium A conical fibroserous sac surrounding the heart and the roots of the great vessels (aorta; venae cavae; pulmonary artery). Pericardium consists of two sacs: the outer fibrous pericardium and the inner serous pericardium. The latter consists of an outer parietal layer facing the fibrous pericardium, and an inner visceral layer (epicardium) resting next to the heart, and a pericardial cavity between these two layers. Heart: Anatomy, pleura Pleura The pleura is a serous membrane that lines the walls of the thoracic cavity and the surface of the lungs. This structure of mesodermal origin covers both lungs, the mediastinum, the thoracic surface of the diaphragm, and the inner part of the thoracic cage. The pleura is divided into a visceral pleura and parietal pleura. Pleura: Anatomy, and lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy that elicit an inflammatory response. Other late complications are atrial and ventricular aneurysms which may precipitate thrombus formation and increased risk of thromboembolism Thromboembolism Obstruction of a blood vessel (embolism) by a blood clot (thrombus) in the blood stream. Systemic Lupus Erythematosus. Finally, ventricular wall rupture leading to pericardial effusion Pericardial effusion Fluid accumulation within the pericardium. Serous effusions are associated with pericardial diseases. Hemopericardium is associated with trauma. Lipid-containing effusion (chylopericardium) results from leakage of thoracic duct. Severe cases can lead to cardiac tamponade. Pericardial Effusion and Cardiac Tamponade and cardiac tamponade Tamponade Pericardial effusion, usually of rapid onset, exceeding ventricular filling pressures and causing collapse of the heart with a markedly reduced cardiac output. Pericarditis is a serious potential late complication after MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction.
This table shows the timing of complications after STEMI:
| Time | Complications |
| 0–24 h | Ventricular arrhythmia, HF, Cardiogenic shock Cardiogenic shock Shock resulting from diminution of cardiac output in heart disease. Types of Shock |
| 1–3 days | Postinfarction fibrinous pericarditis Fibrinous pericarditis Pericarditis |
| 3–14 days | Free wall rupture with tamponade Tamponade Pericardial effusion, usually of rapid onset, exceeding ventricular filling pressures and causing collapse of the heart with a markedly reduced cardiac output. Pericarditis, papillary muscle rupture Papillary muscle rupture Myocardial Infarction with mitral regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD), Interventricular septal rupture due to macrophage-mediated structural degradation, LV pseudoaneurysm Pseudoaneurysm Not an aneurysm but a well-defined collection of blood and connective tissue outside the wall of a blood vessel or the heart. It is the containment of a ruptured blood vessel or heart, such as sealing a rupture of the left ventricle. False aneurysm is formed by organized thrombus and hematoma in surrounding tissue. Thoracic Aortic Aneurysms (risk of rupture) |
| 2 weeks to several months | Dressler syndrome Dressler syndrome Myocardial Infarction, HF, arrhythmias, true ventricular aneurysm Ventricular aneurysm A localized bulging or dilatation in the muscle wall of a heart (myocardium), usually in the left ventricle. Blood-filled aneurysms are dangerous because they may burst. Fibrous aneurysms interfere with the heart function through the loss of contractility. True aneurysm is bound by the vessel wall or cardiac wall. False aneurysms are hematoma caused by myocardial rupture. Myocardial Infarction (risk of mural thrombus Mural thrombus Myocardial Infarction) |
Prevention
Since 95% of acute coronary syndrome cases are manifestations of CHD, an appropriate goal for both patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship and clinicians is the prevention of ASCVD by risk factor reduction. Lifestyle changes address healthy food choices, regular Regular Insulin physical activity, maintaining a body mass index Body mass index An indicator of body density as determined by the relationship of body weight to body height. Bmi=weight (kg)/height squared (m2). Bmi correlates with body fat (adipose tissue). Their relationship varies with age and gender. For adults, bmi falls into these categories: below 18. 5 (underweight); 18. 5-24. 9 (normal); 25. 0-29. 9 (overweight); 30. 0 and above (obese). Obesity ( BMI BMI An indicator of body density as determined by the relationship of body weight to body height. Bmi=weight (kg)/height squared (m2). Bmi correlates with body fat (adipose tissue). Their relationship varies with age and gender. For adults, bmi falls into these categories: below 18. 5 (underweight); 18. 5-24. 9 (normal); 25. 0-29. 9 (overweight); 30. 0 and above (obese). Obesity) below 25 (or similar reasonable goal for specific patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship), and smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases cessation. Other risk factor reduction includes adequate control of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, hyperlipidemia, and diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus with medication in addition to lifestyle changes.
Review Questions
- What do typical
ECG
ECG
An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures.
Electrocardiogram (ECG) changes in a patient with acute STEMI look like?
- ST-segment depression with direct transition into a T-wave
- ST-segment elevation with negative preterminal T-wave
- A pointed depression of the T-wave, the so-called “anoxic” T wave T wave Electrocardiogram (ECG)
- Q-wave
- A monophasic ST-segment elevation with direct transition into a T-wave
- What is the best laboratory test for acute
MI
MI
MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms.
Myocardial Infarction?
- LDH LDH Osteosarcoma
- Troponin I Troponin I A troponin complex subunit that inhibits actomyosin ATPase activity thereby disrupting actin and myosin interaction. There are three troponin I subtypes: troponin i1, i2 and i3. Troponin i3 is cardiac-specific whereas troponin i1 and i2 are skeletal subtypes. Troponin i3 is a biomarker for damaged or injured cardiac myocytes and mutations in troponin i3 gene are associated with familial hypertrophic cardiomyopathy. Myocardial Infarction
- CK-MB
- Myoglobin Myoglobin A conjugated protein which is the oxygen-transporting pigment of muscle. It is made up of one globin polypeptide chain and one heme group. Rhabdomyolysis
- AST AST Enzymes of the transferase class that catalyze the conversion of l-aspartate and 2-ketoglutarate to oxaloacetate and l-glutamate. Liver Function Tests
- Which medication is contraindicated when a patient has also taken
sildenafil
Sildenafil
A phosphodiesterase type-5 inhibitor; vasodilator agent and urological agent that is used in the treatment of erectile dysfunction and primary pulmonary hypertension.
Phosphodiesterase Inhibitors?
- Aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs)
- P2Y12 inhibitors (e.g., clopidogrel Clopidogrel A ticlopidine analog and platelet purinergic p2y receptor antagonist that inhibits adenosine diphosphate-mediated platelet aggregation. It is used to prevent thromboembolism in patients with arterial occlusive diseases; myocardial infarction; stroke; or atrial fibrillation. Antiplatelet Drugs)
- Nitroglycerin Nitroglycerin A volatile vasodilator which relieves angina pectoris by stimulating guanylate cyclase and lowering cytosolic calcium. It is also sometimes used for tocolysis and explosives. Nitrates
- Heparin
- Warfarin Warfarin An anticoagulant that acts by inhibiting the synthesis of vitamin K-dependent coagulation factors. Warfarin is indicated for the prophylaxis and/or treatment of venous thrombosis and its extension, pulmonary embolism, and atrial fibrillation with embolization. It is also used as an adjunct in the prophylaxis of systemic embolism after myocardial infarction. Warfarin is also used as a rodenticide. Anticoagulants
Answers: 1-5, 2-2, 3-3
References
- Mitchell, RN, Halushk, MK. (2020). Blood Vessels. In Kumar, V., Abbas, A. K., Aster, J.C., (Eds.). Robbins & Cotran Pathologic Basis of Disease. (10 ed. pp. 485–525).
- Thygesen, K, Alpert, J.S, et al. (2018). Fourth Universal Definition of Myocardial Infarction (2018). Journal of the American College of Cardiology, 72(18), 2231–64.
- Mensah, G. A., Fuster, V., Murray, C. J. L., et al. (2023). Global burden of cardiovascular diseases and risks, 1990-2022. *Journal of the American College of Cardiology*. https://doi.org/10.1016/j.jacc.2023.11.007
- Martin, S. S., Aday, A. W., Almarzooq, Z. I., Anderson, C. A. M., Arora, P., Avery, C. L., Baker-Smith, C. M., Barone Gibbs, B., Beaton, A. Z., Boehme, A. K., Commodore-Mensah, Y., Currie, M. E., Elkind, M. S. V., Evenson, K. R., Generoso, G., Heard, D. G., Hiremath, S., Johansen, M. C., Kalani, R., … on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2024). 2024 heart disease and stroke statistics: A report of US and global data from the American Heart Association. Circulation, 149(8). https://doi.org/10.1161/CIR.0000000000001209
- Antonopoulos, AS, Siasos, G, Antoniades, C, Tousoulis, D. (2018). Ch. 2.1, Functional Anatomy. In Tousoulis, D. Coronary Artery Disease: From Biology to Clinical Practice. pp. 121–126. https://doi.org/10.1016/B978-0-12-811908-2.00008-8
- Wu, JC. (2019). Ch. 18, Acute Myocardial Infarction. In Solomon, SD, Wu, JC, and Gillam, LD. Essential Echocardiography: A Companion to Braunwald’s Heart Disease (1st Ed, pp.195–199).
- Rapsomaniki, E, Timmis, A, et al. (2014). Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet, 383(9932), 1899–911.
- Lloyd-Jones, DM. (2019). Ch 46, Epidemiology of cardiovascular disease. In Crow, MK, et al. (Eds.), Goldman-Cecil Medicine. (26th ed. Vol 1, pp. 237–239).
- Arnett DK, Blumenthal RS, et al. (2019). ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Sep 10;140(11):e596–e646.
- Almeida, S.O., & Budoff, M. (2019). Effect of statins on atherosclerotic plaque. Trends in cardiovascular medicine, 29(8), 451–5.
- Goldman, L. (2019) Chapter 45, Approach to the patient with possible cardiovascular disease. In Crow, MK et al. (Eds.), Goldman-Cecil Medicine. (26th ed. Vol 1, pp. 230–237).
- Gulati, R, Behfar, A, et al. (2020). Acute Myocardial Infarction in Young Individuals. Mayo Clinic Proceedings, 95(1), 136–56.
- Gewirtz, H. (2019). Coronary circulation: Pressure/flow parameters for assessment of ischemic heart disease. Journal of nuclear cardiology: official publication of the American Society of Nuclear Cardiology, 26(2), 459–70.
- Khav, N, Ihdayhid, AR, & Ko, B. (2020). CT-Derived Fractional Flow Reserve (CT-FFR) in the Evaluation of Coronary Artery Disease. Heart, lung & circulation, 29(11), 1621–32.
- Shao, C, Wang, J, Tian, J, & Tang, YD. (2020). Coronary Artery Disease: From Mechanism to Clinical Practice. Advances in experimental medicine and biology, 1177, 1–36.
- Isbister, J., & Semsarian, C. (2019). Sudden cardiac death: an update. Internal medicine journal, 49(7), 826–33.
- Hoffmann U, Ferencik M, Udelson JE, et al. (2017). Prognostic value of noninvasive cardiovascular testing in patients with stable chest pain: insights from the PROMISE trial (prospective multicenter imaging study for evaluation of chest pain). Circulation.135:2320–2332.
- Kramer, CM, Beller, GA, & Hagspiel, KD. (2019). Ch. 50, Noninvasive cardiac imaging. In Crow, MK et al. (Eds.), Goldman-Cecil Medicine. (26th ed. Vol 1, pp. 261–264).
- Teoh, Z, & Al-Lamee, RK. (2020). COURAGE, ORBITA, and ISCHEMIA: Percutaneous Coronary Intervention for Stable Coronary Artery Disease. Interventional cardiology clinics, 9(4), 469–82.
- Teirstein, PS. (2019). Ch. 65, Interventional and surgical treatment of coronary artery disease. In Crow, MK et al. (Eds.), Goldman-Cecil Medicine. (26th ed. Vol 1, pp. 737–405).
- Long, L, Anderson, L, Dewhirst AM, et al. (2018). Exercise-based cardiac rehabilitation for adults with stable angina. Cochrane Database Syst Rev. 2018;2:CD012786.
- Jenkins, K., Pompei, G., Ganzorig, N., Brown, S., Beltrame, J., & Kunadian, V. (2024). Vasospastic angina: A review on diagnostic approach and management. Therapeutic Advances in Cardiovascular Disease, 18, 17539447241230400. https://doi.org/10.1177/17539447241230400
- Hata, R, Oka, N, Kubo, S, et al. (2018). Impact of Stent Type and Presence of Vasospastic Angina on Long-Term Prognosis. Circulation journal: official journal of the Japanese Circulation Society, 82(2), 469–76.
- Kusama, Y, Kondani, E, et al. (2011). Variant angina and coronary artery spasm: the clinical spectrum, pathophysiology, and management. Journal of Nippon Medical School. 78(1), 4–12.
- Winzer, EB, Woitek, F, & Linke, A. (2018). Physical Activity in the Prevention and Treatment of Coronary Artery Disease. Journal of the American Heart Association, 7(4), e007725.
- Saito, K, Kondo, Y, et al. (2021). Factors that predict ventricular arrhythmias in the late phase after acute myocardial infarction. ESC heart failure, 8(5), 4152-60.
- Kim, HL, & Jo, SH. (2021). Current Evidence on Long-Term Prognostic Factors in Vasospastic Angina. Journal of clinical medicine, 10(18), 4270.
- Horiuchi, Y, Wettersten, N, Patel, MP, Met al. (2020). Biomarkers Enhance Discrimination and Prognosis of Type 2 Myocardial Infarction. Circulation, 142(16), 1532–44.
- McCarthy, CP, Kolte, D, Kennedy, KF, Vaduganathan, M, Wasfy, JH, & Januzzi, JL. (2021). Patient Characteristics and Clinical Outcomes of Type 1 Versus Type 2 Myocardial Infarction. Journal of the American College of Cardiology, 77(7), 848–57.
- Krittanawong, C., Khawaja, M., Tamis‐Holland, J. E., Girotra, S., & Rao, S. V. (2023). Acute myocardial infarction: Etiologies and mimickers in young patients. Journal of the American Heart Association, 12(18), e029971. https://doi.org/10.1161/JAHA.123.029971
- Lange, RA & Mukherjee, D. (2019). Ch 63, Acute coronary syndrome: unstable angina and Non–ST elevation myocardial infarction. In Crow, MK et al. (Eds.), Goldman-Cecil Medicine. (26th ed. Vol 1, pp. 379–387).
- Anderson, JL & Fang, JC. (2019). Ch. 64, ST elevation acute myocardial infarction and complications of myocardial infarction. In Crow, MK et al. (Eds.), Goldman-Cecil Medicine. (26th ed. Vol 1, pp. 388–400).
- Mancini, GBJ, Boden WE, et al. (2018). Impact of treatment strategies on outcomes in patients with stable coronary artery disease and type 2 diabetes mellitus according to presenting angina severity: A pooled analysis of three federally-funded randomized trials. Atherosclerosis.;277: 186–194.
- Hedayati, T, Yadav, N, & Khanagavi, J. (2018). Non-ST-Segment Acute Coronary Syndromes. Cardiology clinics, 36(1), 37–52.
- Hartikainen, TS, Sörensen, NA, et al. (2021). Application of the Fourth Universal Definition of MI Using FDA-Recommended Sex-Specific Troponin Cutoff Concentrations. Journal of the American College of Cardiology, 77(18), 2346–8.
- Than, MP, Aldous, SJ, et al. (2018). Detectable High-Sensitivity Cardiac Troponin within the Population Reference Interval Conveys High 5-Year Cardiovascular Risk: An Observational Study. Clinical chemistry, 64(7), 1044–53.
- Narula, J, Chandrashekhar, Y, Ahmadi, A, et al. (2021). SCCT 2021 Expert Consensus Document on Coronary Computed Tomographic Angiography: A Report of the Society of Cardiovascular Computed Tomography. Journal of cardiovascular computed tomography, 15(3), 192–217.
- Jobs A, Mehta SR, Montalescot G, et al. Optimal timing of an invasive strategy in patients with non-ST-elevation acute coronary syndrome: a meta-analysis of randomized trials. Lancet. 2017;390:737–746.
- Yukselen, Z., Majmundar, V., Dasari, M., Arun Kumar, P., & Singh, Y. (2024). Chest pain risk stratification in the emergency department: Current perspectives. Open Access Emergency Medicine : OAEM, 16, 29–43. https://doi.org/10.2147/OAEM.S419657
- Virk, H. U. H., Escobar, J., Rodriguez, M., Bates, E. R., Khalid, U., Jneid, H., Birnbaum, Y., Levine, G. N., Smith, S. C., & Krittanawong, C. (2023). Dual antiplatelet therapy: A concise review for clinicians. Life, 13(7), 1580. https://doi.org/10.3390/life13071580
- Bhogal, S, Mukherjee, D, et al. (2020). Bivalirudin Versus Heparin During Intervention in Acute Coronary Syndrome: A Systematic Review of Randomized Trials. Cardiovascular & hematological disorders drug targets, 20(1), 3–15.
- Vavuranakis M, Kariori M, Siasos G, et al. (2017). Statins in acute coronary syndromes. Current Pharmaceutical Design. 2017;23:7086–7098.
- Byrne, R. A., Rossello, X., Coughlan, J. J., Barbato, E., Berry, C., Chieffo, A., Claeys, M. J., Dan, G.-A., Dweck, M. R., Galbraith, M., et al. (2023). 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal, 44(38), 3720-3826. https://doi.org/10.1093/eurheartj/ehad191
- Krittanawong, C, Hahn, J, Kayani, W, & Jneid, H. (2021). Fibrinolytic Therapy in Patients with Acute ST-elevation Myocardial Infarction. Interventional cardiology clinics, 10(3), 381–90.
- Govea, A, Lipinksi, J, & Patel, MP. (2021). Prehospital Evaluation, ED Management, Transfers, and Management of Inpatient STEMI. Interventional cardiology clinics, 10(3), 293–306.
- Ye, F, Winchester, D, Jansen, M, et al. (2019). Assessing Prognosis of Acute Coronary Syndrome in Recent Clinical Trials: A Systematic Review. Clinical medicine & research, 17(1–2), 11–9.
- Rivera, F. B., Cha, S. W., Varona, M. C., Fernandez Co, E. M., Magalong, J. V., Aparece, J. P., De Oliveira-Gomes, D., Kaur, G., & Gulati, M. (2024). Atherosclerotic coronary plaque regression from lipid-lowering therapies: A meta-analysis and meta-regression. American Journal of Preventive Cardiology, 18, 100645. https://doi.org/10.1016/j.ajpc.2024.100645
- Rivera, F. B., Cha, S. W., Varona, M. C., Fernandez Co, E. M., Magalong, J. V., Aparece, J. P., De Oliveira-Gomes, D., Kaur, G., & Gulati, M. (2024). Atherosclerotic coronary plaque regression from lipid-lowering therapies: A meta-analysis and meta-regression. American Journal of Preventive Cardiology, 18, 100645. https://doi.org/10.1016/j.ajpc.2024.100645
- Jaramillo, A. P., Yasir, M., Iyer, N., Hussein, S., & Sn, V. P. (2023). Sudden cardiac death: A systematic review. Cureus, 15(8), e42859. https://doi.org/10.7759/cureus.42859
- Yang, S., & Koo, B.-K. (2024). Noninvasive coronary physiological assessment derived from computed tomography. Journal of Structural and Functional Assessment in Cardiology. https://doi.org/10.1016/j.jscai.2024.101304
- Yang, S., & Koo, B.-K. (2024). Noninvasive coronary physiological assessment derived from computed tomography. Journal of Structural and Functional Assessment in Cardiology. https://doi.org/10.1016/j.jscai.2024.101304
- Baumer Y, Mehta NN, Dey AK, et al. (2020). Cholesterol crystals and atherosclerosis. European Heart Journal, 41, 2236.
- Ehara S, Ueda M, Naruko T, et al. (2021). Elevated levels of oxidized low-density lipoprotein show a positive relationship with the severity of acute coronary syndromes. Circulation, 103, 1955.
- Poznyak AV, Wu WK, Melnichenko AA, et al. (2020). Signaling Pathways and Key Genes Involved in Regulation of Foam Cell Formation in Atherosclerosis. Cells, 9.
- Poznyak AV, Bharadwaj D, Prasad G, et al. (2021). Renin-Angiotensin System in Pathogenesis of Atherosclerosis and Treatment of CVD. International Journal of Molecular Sciences, 22.
- Tamis-Holland, J. E., Jneid, H., Reynolds, H. R., et al. (2019). Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement From the American Heart Association. Circulation, 139, e891.
- Knuuti, J., Wijns, W., Saraste, A., et al. (2020). 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. European Heart Journal, 41, 407.
- Beltrame, J. F., Tavella, R., Jones, D., Zeitz, C. (2021). Management of ischaemia with non-obstructive coronary arteries (INOCA). BMJ, 375, e060602.
- Mileva, N., Nagumo, S., Mizukami, T., et al. (2022). Prevalence of Coronary Microvascular Disease and Coronary Vasospasm in Patients With Nonobstructive Coronary Artery Disease: Systematic Review and Meta-Analysis. Journal of the American Heart Association, 11, e023207.
- Fedele, D., Canton, L., Bodega, F., Suma, N., Tattilo, F. P., Impellizzeri, A., Amicone, S., Di Iuorio, O., Ryabenko, K., Armillotta, M., Sansonetti, A., Stefanizzi, A., Cavallo, D., Casuso, M., Bertolini, D., Lovato, L., Gallinoro, E., Belmonte, M., Rinaldi, A., Angeli, F., Casella, G., Foà, A., Bergamaschi, L., Paolisso, P., & Pizzi, C. (2023). Performance of prognostic scoring systems in MINOCA: A comparison among GRACE, TIMI, HEART, and ACEF scores. J. Clin. Med., 12, 5687. https://doi.org/10.3390/jcm1217567