Start your online microbiology course
taught by Sean Elliot, MD, University of Arizona, and Vincent Racaniello, PhD, Columbia University
Infectious diseases are still a prominent cause of morbidity and mortality worldwide. Their treatment builds on the understanding of microorganisms and their relationship to disease processes. Gaining an overview of the many classes and groups is challenging for many students at first.
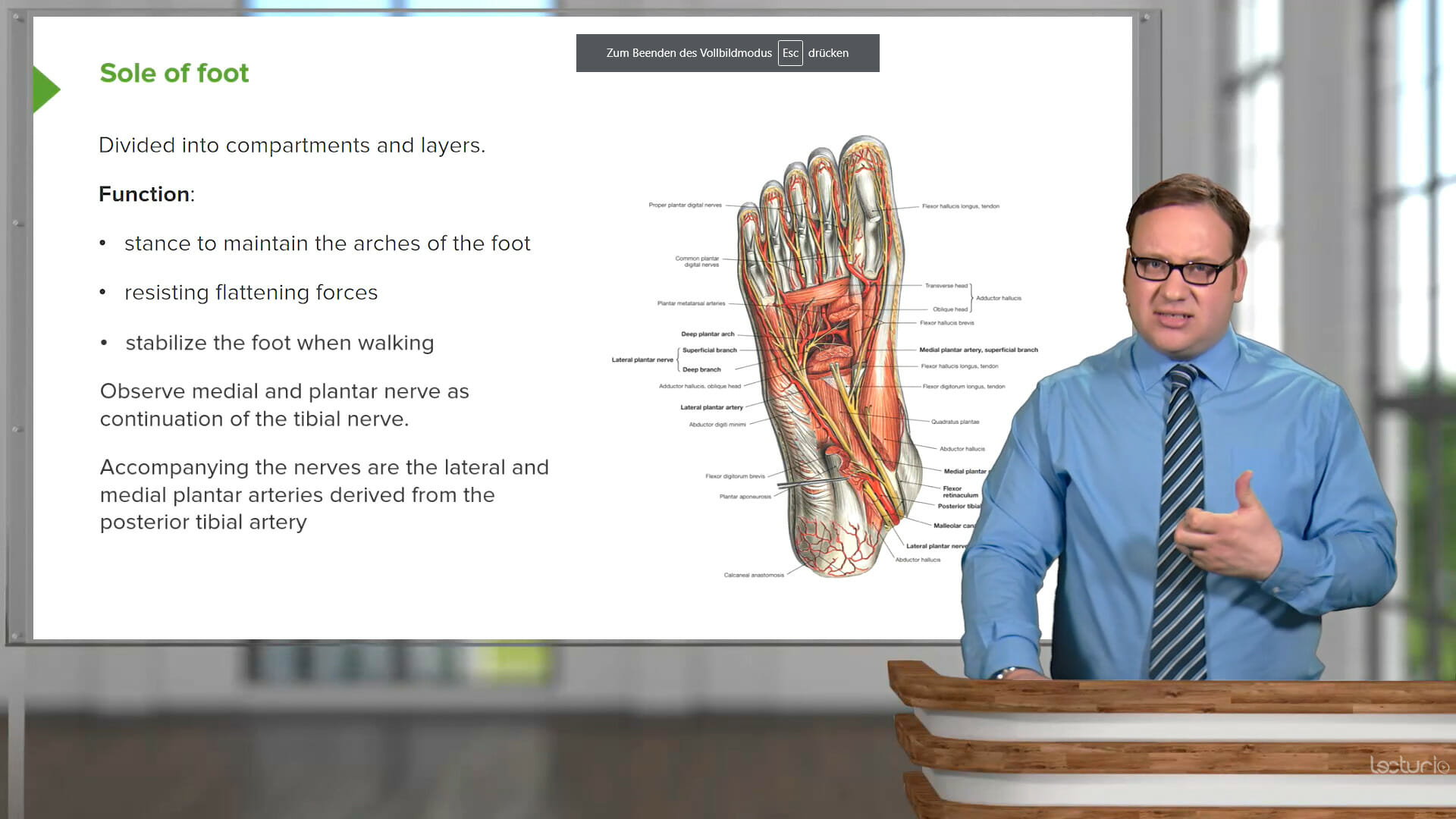
This course covers the major groups and families of microorganisms relevant to human health, including bacteria, viruses, fungi, parasites, and prions. You will learn about the mechanisms of contagion and prevention, and explore critical related concepts like genetic engineering. Your educators are Vincent Racaniello, PhD who is an experienced Professor of Microbiology, and Sean Elliot, MD, who is a pediatric infectious disease specialist.
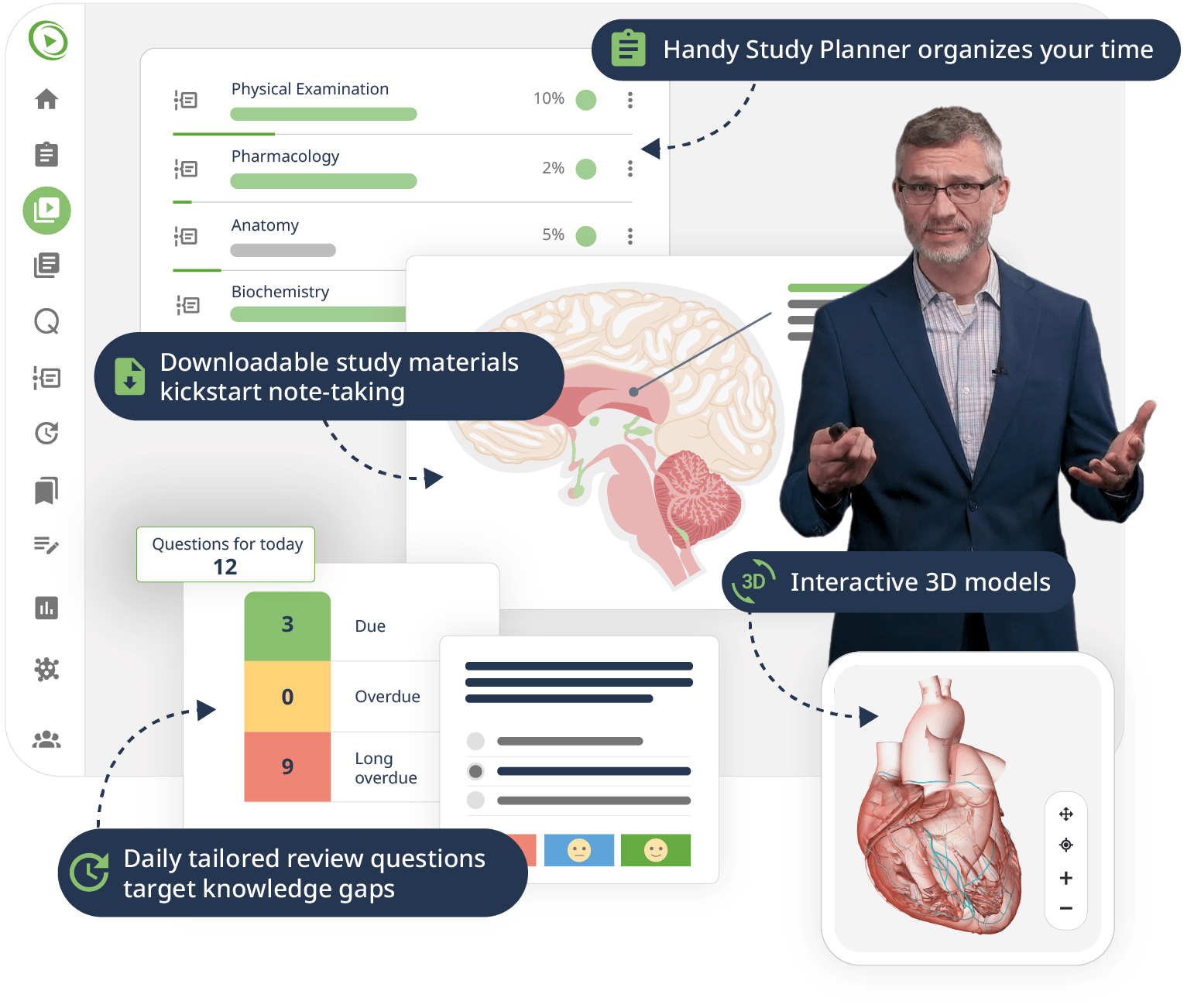
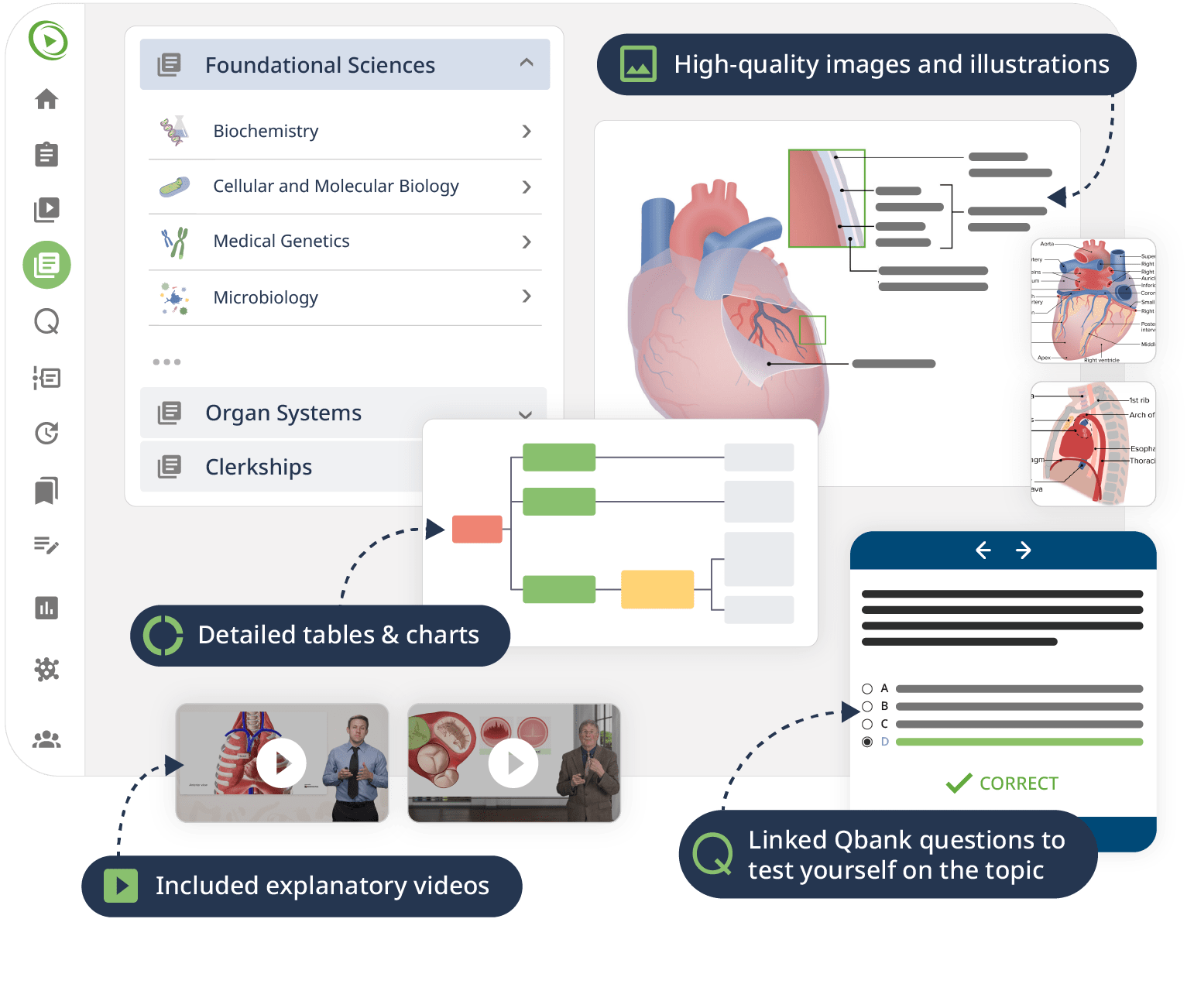
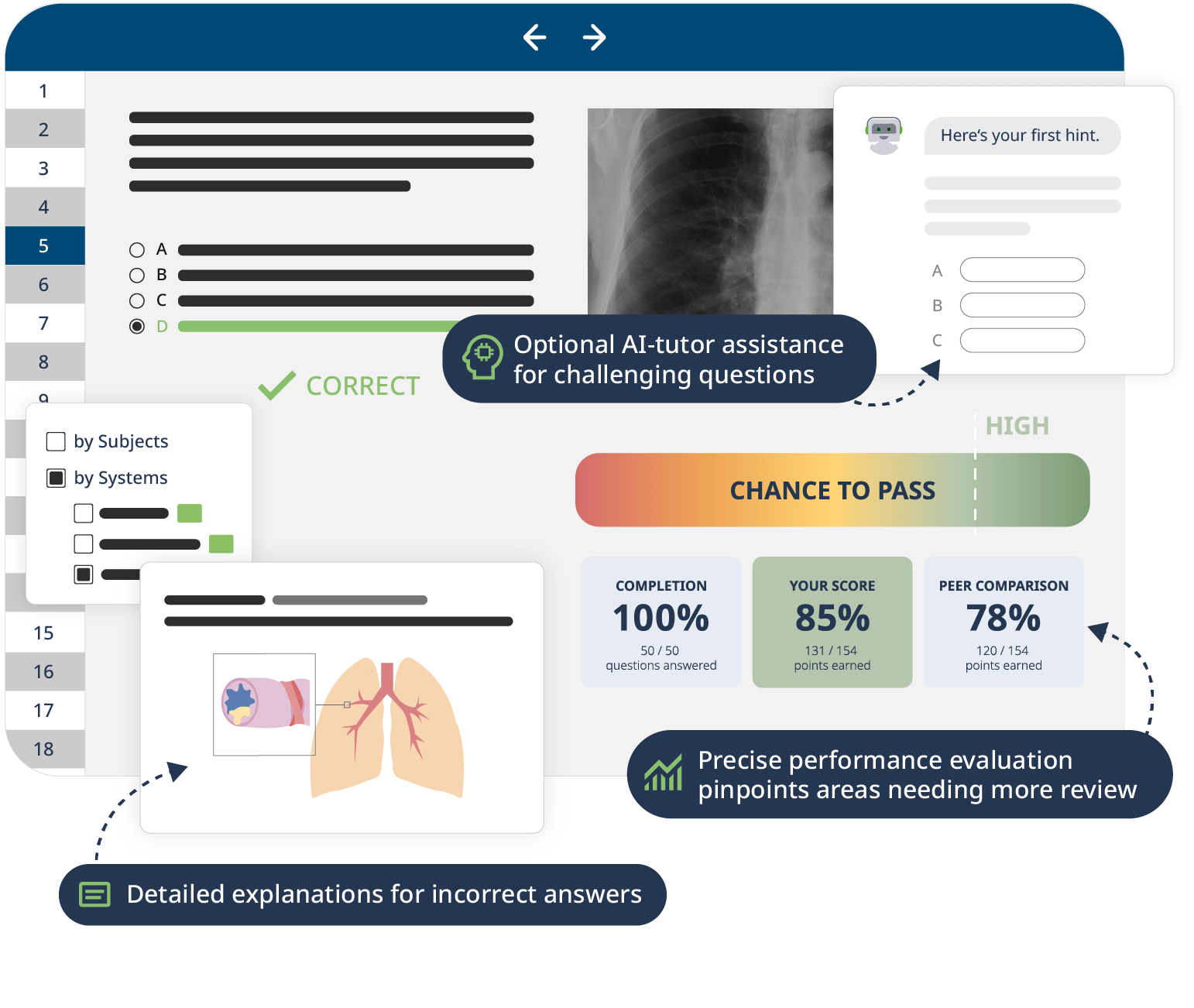
The combination of Video Lessons with interactive quiz questions, downloadable study materials, and a USMLE-style Qbank makes it easy to understand and retain the topics. By the end of this course, you will have a comprehensive understanding of microbiology, ready to apply this knowledge in clinical settings and excel in your exams.