Polyarteritis nodosa (PAN) is a necrotizing, systemic, primarily medium-vessel vasculitis. Most cases of PAN are idiopathic. Etiologic factors in secondary PAN are hepatitis B and C infection and hairy cell leukemia. PAN presents with systemic symptoms and signs such as fatigue, weight loss, fever, weakness, arthralgias, hypertension, and limb edema. Because it is a multisystem disease affecting the skin, nerves, muscles, kidneys, and blood vessels supplying the heart and GI tract, the clinical presentation depends on the organs involved. A diagnosis is made based on the history, physical examination, and laboratory test results and confirmed by biopsy or angiography. Management depends on the severity and extent of the disease. The primary treatment method is with oral glucocorticoids; immunosuppressive agents may also be needed for patients with moderate-to-severe disease.
Last updated: May 16, 2024
Polyarteritis nodosa Polyarteritis nodosa A form of necrotizing non-granulomatous inflammation occurring primarily in medium-sized arteries, often with microaneurysms. It is characterized by muscle, joint, and abdominal pain resulting from arterial infarction and scarring in affected organs. Polyarteritis nodosa with lung involvement is called churg-strauss syndrome. Vasculitides (PAN) is a systemic, primarily medium-vessel vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus characterized by necrotizing inflammatory lesions. This condition eventually results in microaneurysms, which lead to bleeding, thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus, organ ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, and infarction.
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with PAN typically present with multisystem involvement and systemic signs and symptoms. However, there is also a skin-limited form called cutaneous PAN.
| System | Clinical presentation |
|---|---|
| Renal |
|
| Cutaneous |
|
| Nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification |
|
| Muscular |
|
| Gastrointestinal |
|
| Cardiovascular |
|
| Reproductive |
|
| Ophthalmic |
|

Bilateral palpable purpura as a cutaneous manifestation of PAN
Image: “Bilateral palpable purpura in lower extremities” by gan Y, Doğru A, Şencan H, Şahin M, Ercan Tunç Ş. License: CC BY 4.0
PAN associated with HCV infection.
A panniculitis-type skin rash with tender hard nodules is present
The diagnosis of PAN is made based on history, physical examination, and laboratory test results and should be confirmed by biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma whenever possible.
Laboratory findings are generally nonspecific, and studies may be used to assess organ system involvement and rule out other likely diagnoses.
Skin biopsy shows perivascular lymphocytic and neutrophilic infiltration with fibrinoid necrosis of vessel wall and leukocytoclastic and red cell extravasations in an individual with polyarteritis nodosa.
Image: “Skin biopsy shows perivascular lymphocytic and neutrophilic infiltration” by Rodrigo D et al. License: CC BY 2.0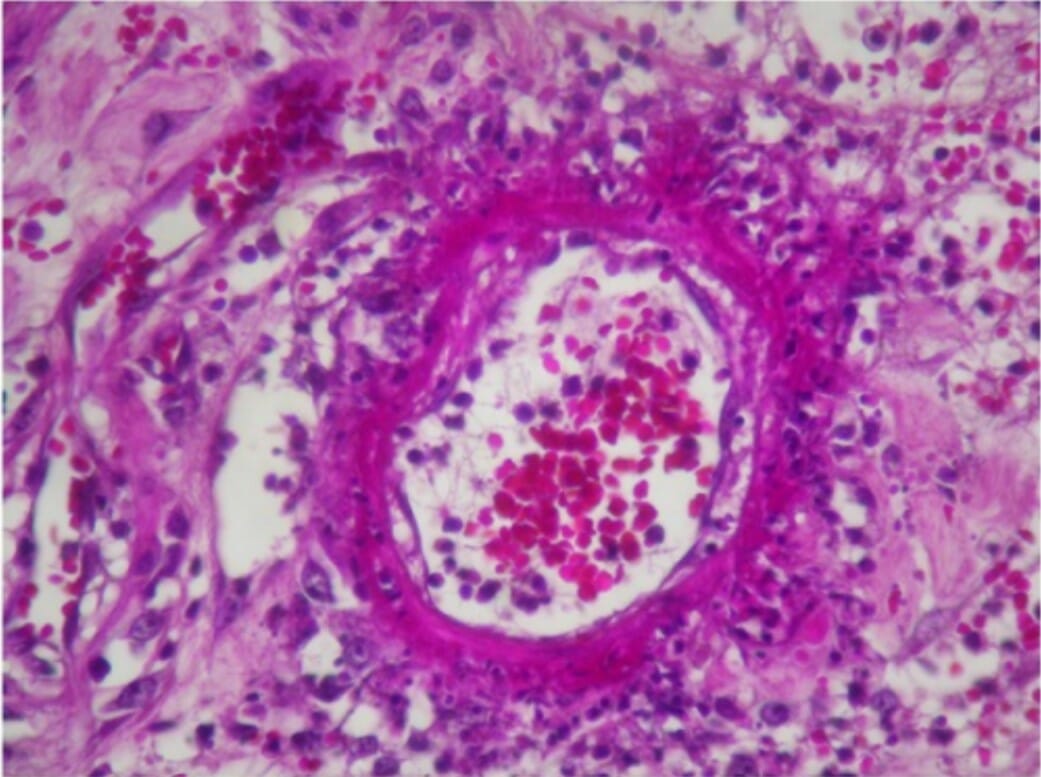
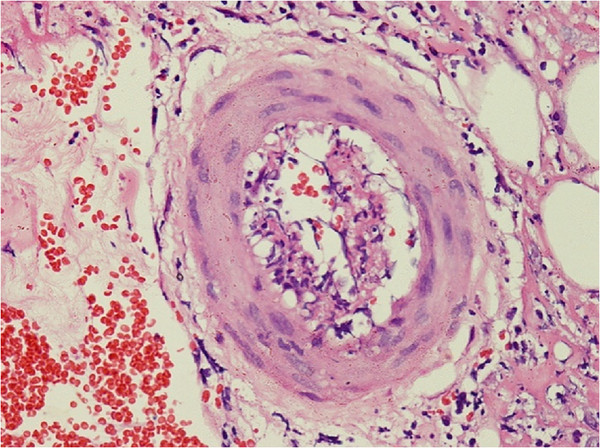
Ischemic colitis due to PAN vasculitis:
Histologic examination of the resected colon demonstrates fibrinoid necrosis with an inflammatory infiltrate rich in neutrophils.
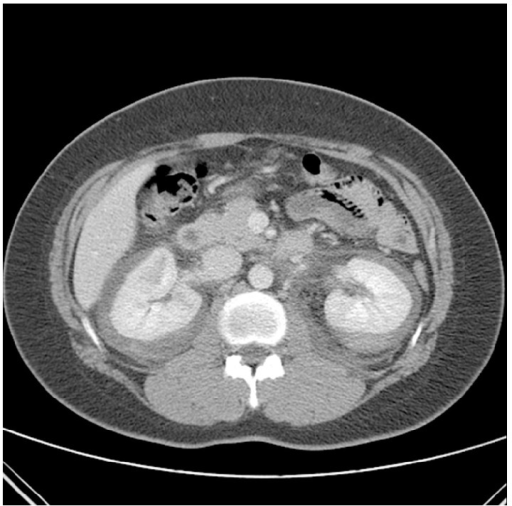
Contrast-enhanced CT with spontaneous bilateral perirenal hemorrhage (rare complication) as the initial presentation of PAN in an individual with flank pain and hypovolemia
Image: “Contrast enhanced CT on the day of admission. CT revealed nonspecific spontaneous bilateral perirenal hemorrhage and delayed enhancing lesion of renal medulla” by Choi HI, Kim YG, Kim SY, Jeong da W, Kim KP, Jeong KH, Lee SH, Moon JY. License: CC BY 3.0Assessing disease severity is helpful for determining the best management option.
Management depends on the severity and extent of the disease and should be guided by a specialist (rheumatologist). The primary treatment method is with oral glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids. Immunosuppressive agents may also be needed for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with moderate-to-severe disease.
Mild PAN:
Moderate-to-severe PAN:
Monitoring of PAN:
The prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas depends on disease severity and response to treatment.