The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism ( carbohydrates Carbohydrates A class of organic compounds composed of carbon, hydrogen, and oxygen in a ratio of cn(H2O)n. The largest class of organic compounds, including starch; glycogen; cellulose; polysaccharides; and simple monosaccharides. Basics of Carbohydrates, proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis, lipids Lipids Lipids are a diverse group of hydrophobic organic molecules, which include fats, oils, sterols, and waxes. Fatty Acids and Lipids, hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types), nutrient storage (e.g., iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements and vitamins), synthesis Synthesis Polymerase Chain Reaction (PCR) of coagulation factors Coagulation factors Endogenous substances, usually proteins, that are involved in the blood coagulation process. Hemostasis, formation of bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy, filtration, and storage of blood. The liver can be divided into 4 lobes or 8 segments. Microscopically, it is divided into hepatic lobules Lobules Breasts: Anatomy. Its main neurovascular bundle is found within the transverse fissure Fissure A crack or split that extends into the dermis Generalized and Localized Rashes of the liver, also called the porta hepatis.
Last updated: Dec 15, 2025
The liver is the largest gland in the body. It extends from the right to the left hypochondriac region (¾ of the liver is in the right superior quadrant).
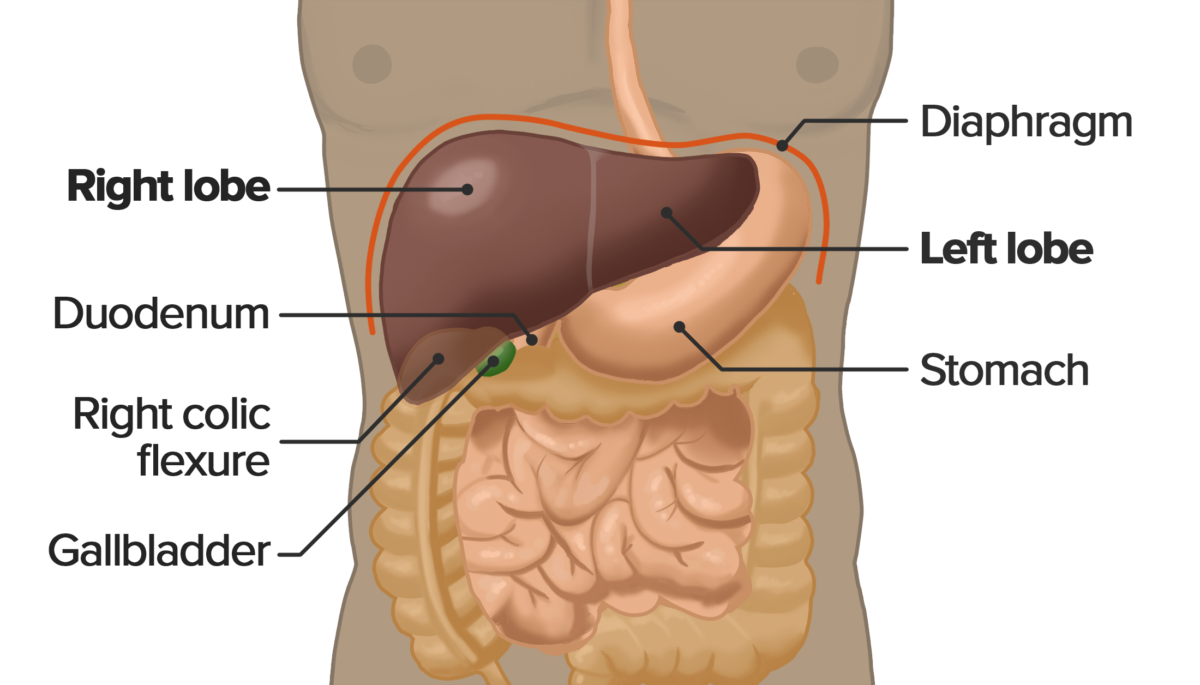
Location of the liver within the abdominal cavity
Image by Lecturio.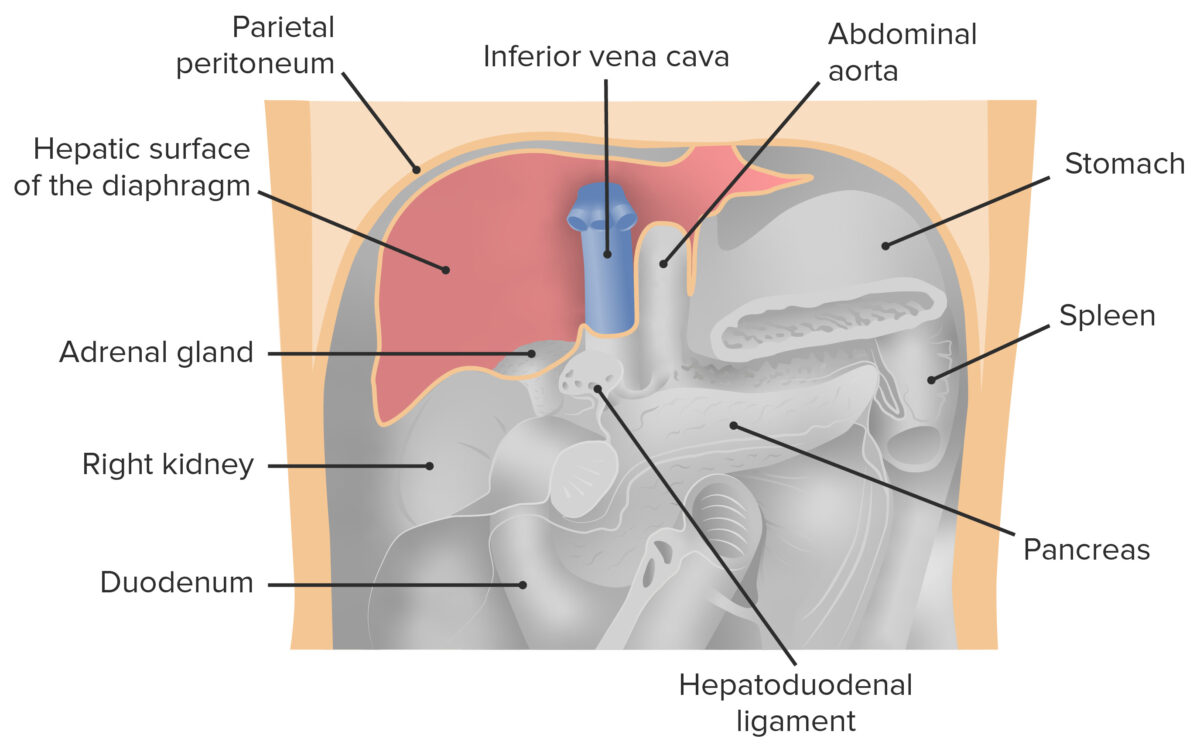
Frontal view of the abdominal cavity with the liver removed. Image shows the position of the liver in the peritoneal cavity in relation to neighboring organs.
Image by Lecturio.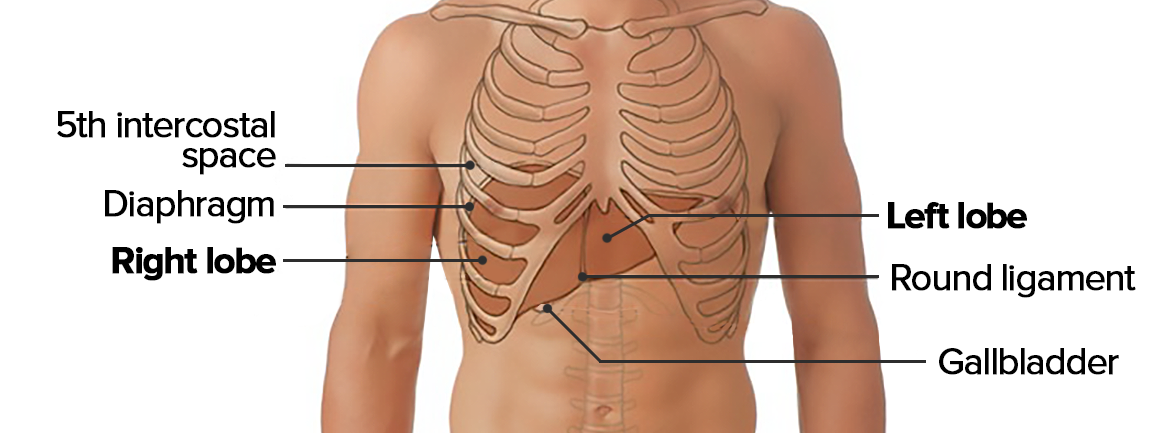
Topography of the liver
Image by Lecturio.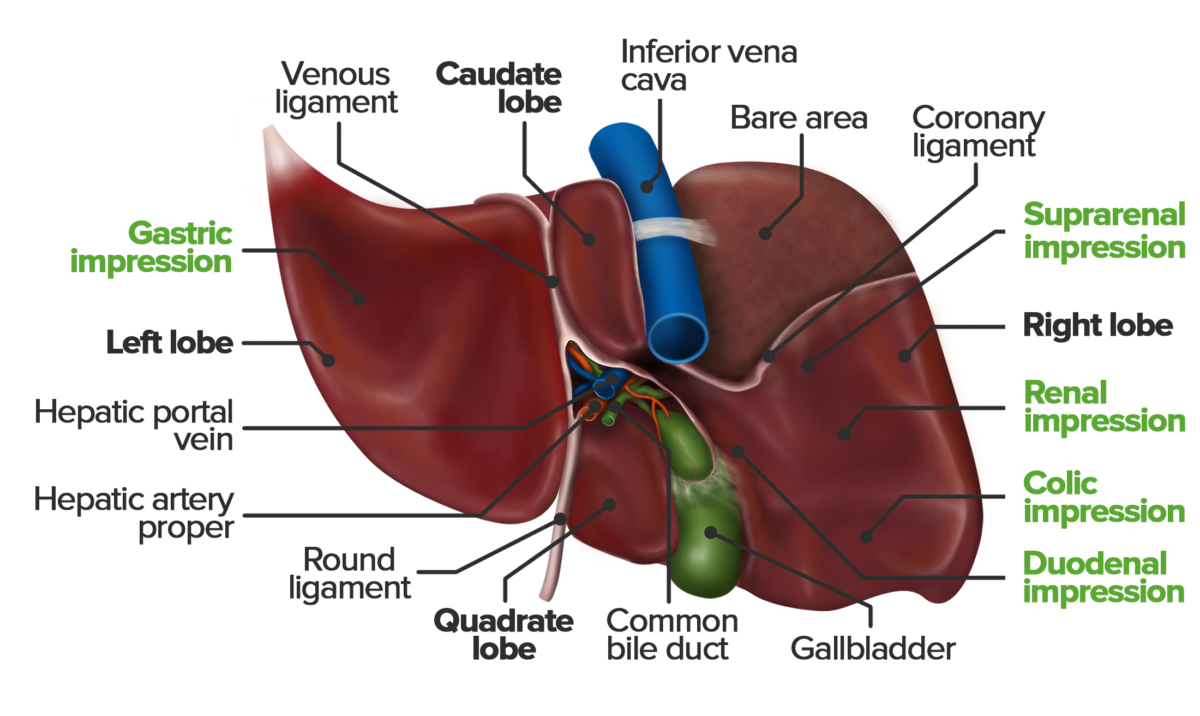
Inferior view of the visceral surface of the liver. Note the uneven structure that results from impressions of the neighboring organs. The colic impression is caused by the colon’s hepatic flexure; the descending portion of the duodenum forms the duodenal impression.
Image by Lecturio.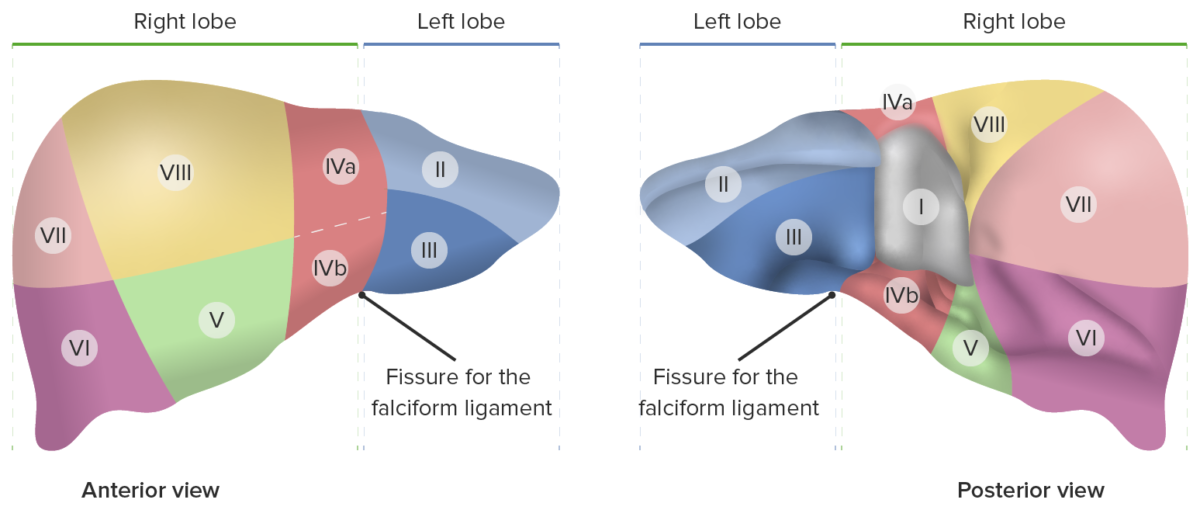
Eight hepatic segments according to the Couinaud classification system.
Image by Lecturio.The porta hepatis (also called the hepatic portal) is a transverse fissure Fissure A crack or split that extends into the dermis Generalized and Localized Rashes that separates the caudate and quadrate lobes and serves as a passageway for the following:
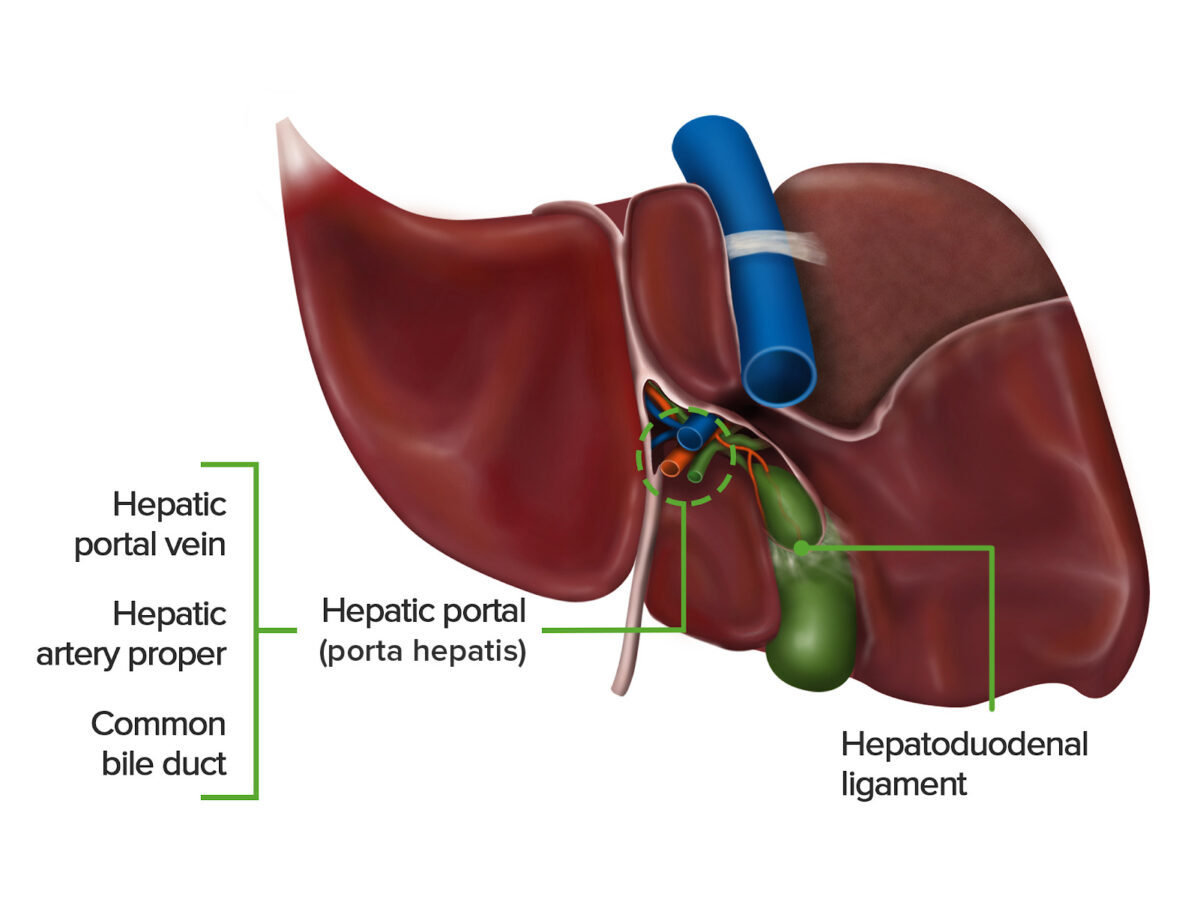
Inferior view of the visceral surface of the liver, featuring the hepatic portal and surrounding hepatoduodenal ligament.
Image by Lecturio.Definition: Ligaments of the liver are double layers of visceral peritoneum Visceral peritoneum Peritoneum: Anatomy that fix the position of the liver by attaching it to the surrounding structures.
|
Coronary ligaments
Coronary ligaments
Knee Joint: Anatomy (anterior and posterior) |
Peritoneal reflection from the
diaphragm
Diaphragm
The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force.
Diaphragm: Anatomy to the liver Demarcates the bare area (surface of the liver with no peritoneal covering) |
| Falciform ligament |
Peritoneal reflection from the umbilicus to the liver Remnant of the embryonic ventral mesentery Mesentery A layer of the peritoneum which attaches the abdominal viscera to the abdominal wall and conveys their blood vessels and nerves. Peritoneum: Anatomy Its free edge contains the round ligament Round ligament A fibromuscular band that attaches to the uterus and then passes along the broad ligament, out through the inguinal ring, and into the labium majus. Uterus, Cervix, and Fallopian Tubes: Anatomy of the liver. |
| Hepatoduodenal ligament |
Portion of the lesser
omentum
Omentum
Peritoneum: Anatomy Extends from the porta hepatis to the superior part of the duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy contents: hepatic artery proper, portal vein, common hepatic duct |
| Hepatogastric ligament |
Extends from the liver to the
lesser curvature
Lesser curvature
Stomach: Anatomy of the
stomach
Stomach
The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus.
Stomach: Anatomy contents: gastric arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology |
|
Round ligament
Round ligament
A fibromuscular band that attaches to the uterus and then passes along the broad ligament, out through the inguinal ring, and into the labium majus.
Uterus, Cervix, and Fallopian Tubes: Anatomy (also known as ligamentum teres) |
Remnant of the intra-abdominal portion of the
umbilical vein
umbilical vein
Venous vessels in the umbilical cord. They carry oxygenated, nutrient-rich blood from the mother to the fetus via the placenta. In humans, there is normally one umbilical vein.
Prenatal and Postnatal Physiology of the Neonate Extends from the umbilicus to the liver on the free edge of the falciform ligament |
| Triangular ligaments |
Formed by the fusion of the anterior and posterior folds of the coronary ligament 1 left and 1 right; both extend from the liver to the diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy |
|
Venous ligament (also known as ligamentum venosum) |
Remnant of the
ductus venosus
Ductus venosus
Development of the Heart Extends from the remnant of the intra-abdominal portion of the umbilical vein umbilical vein Venous vessels in the umbilical cord. They carry oxygenated, nutrient-rich blood from the mother to the fetus via the placenta. In humans, there is normally one umbilical vein. Prenatal and Postnatal Physiology of the Neonate to the inferior vena cava Inferior vena cava The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy |
| Left fissure Fissure A crack or split that extends into the dermis Generalized and Localized Rashes | Impressions of the round and venous ligaments |
| Right fissure Fissure A crack or split that extends into the dermis Generalized and Localized Rashes | Impressions of the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy and the inferior caval vein |
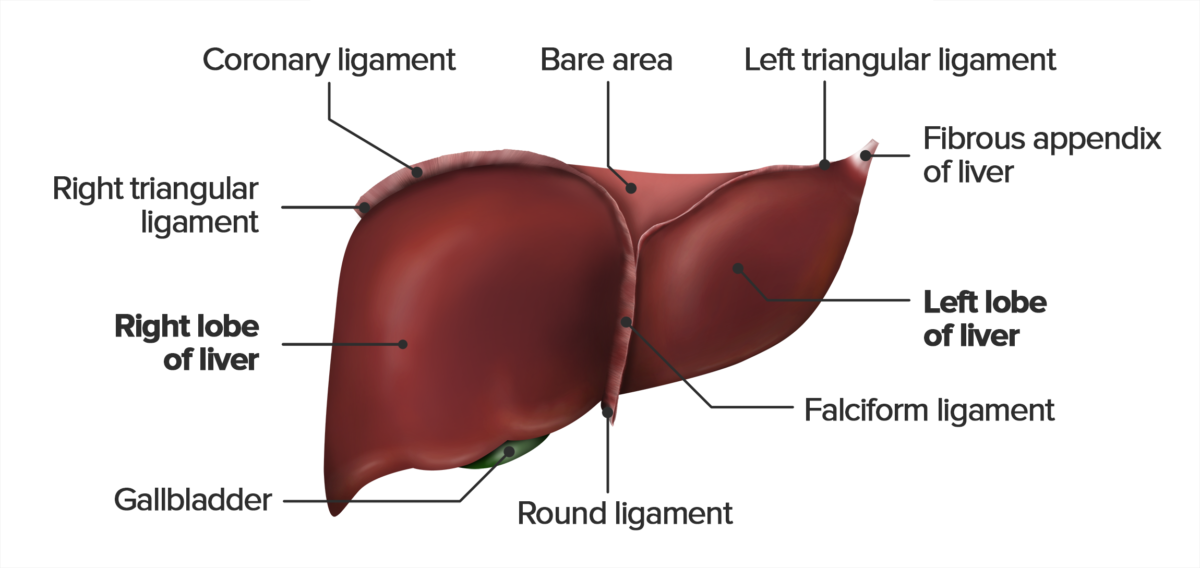
Anterior view of the diaphragmatic surface of the liver, featuring the falciform, triangular, round, and coronary ligaments. Note that the round ligament extends from the free edge of the falciform ligament.
Image by Lecturio.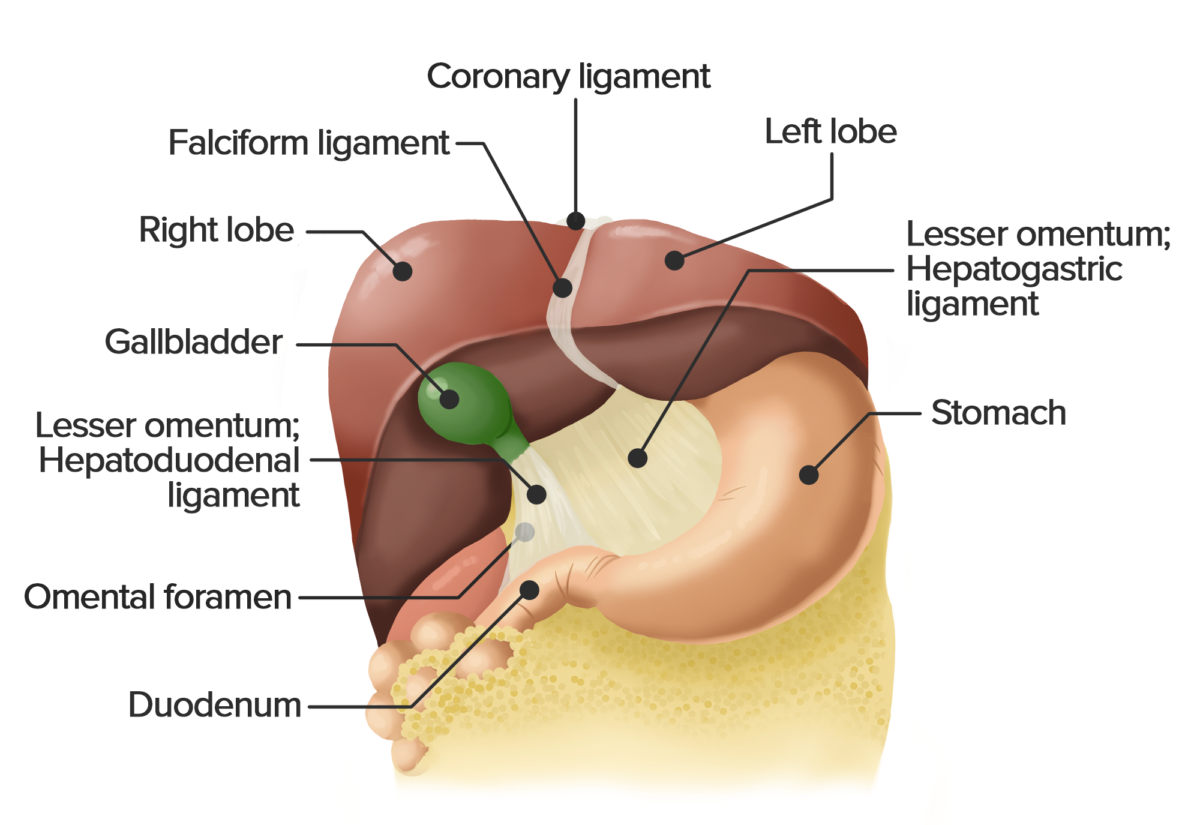
Anterior view of the liver. The liver has been lifted to show the lesser omentum, which consists of the hepatogastric and hepatoduodenal ligament. This double layer of peritoneum connects the liver with the lesser curvature of the stomach and the duodenum.
Image by Lecturio.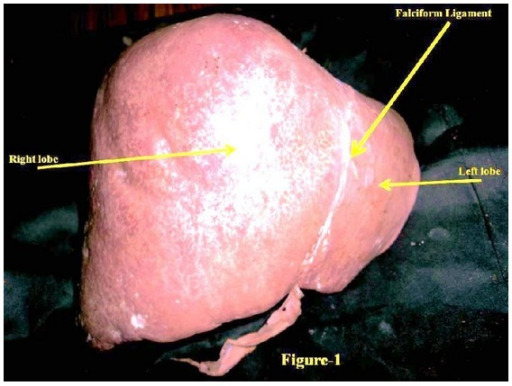
Anterosuperior view of a human liver
Image: “Hypoplastic left lobe of liver with accessory caudate lobe.” by Department of Anatomy, AIIMS, Rishikesh, Uttarakhand 249201, India. License: CC BY 3.0
Posteroinferior view of a liver
Image: “Hypoplastic left lobe of liver with accessory caudate lobe.” by Department of Anatomy, AIIMS, Rishikesh, Uttarakhand 249201, India. License: CC BY 3.0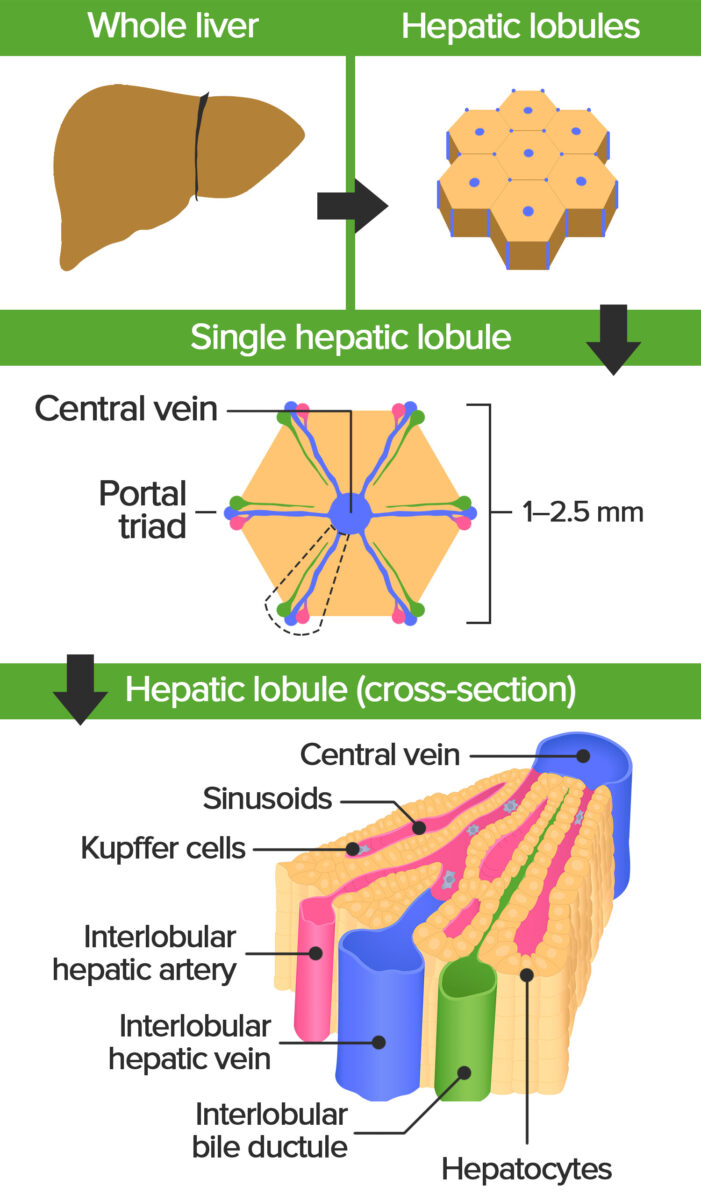
Schematic diagram of the architecture of the liver, featuring the hepatic lobule. The portal triads at the corners consist of branches of the portal vein, hepatic artery proper, and a bile duct. The branch of the portal vein carries nutrient-rich, but deoxygenated blood from the small intestine, the branch of the hepatic artery supplies the hepatocytes with oxygenated blood. The bile duct drains bile from the hepatocytes towards larger ducts and the gall bladder.
Image by Lecturio.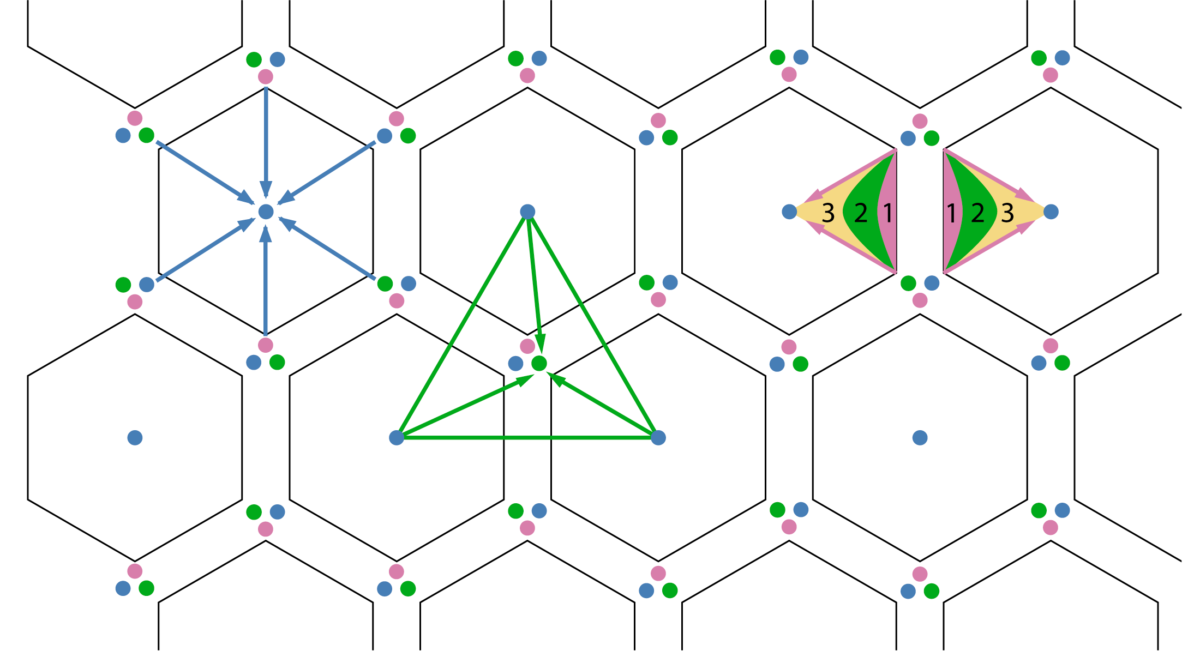
Schematic diagram of the 3 types of hepatic units. Note the portal triads located at the vertices of the hexagonal units and the 3 histological zones within the hepatic acinus.
Image by Lecturio.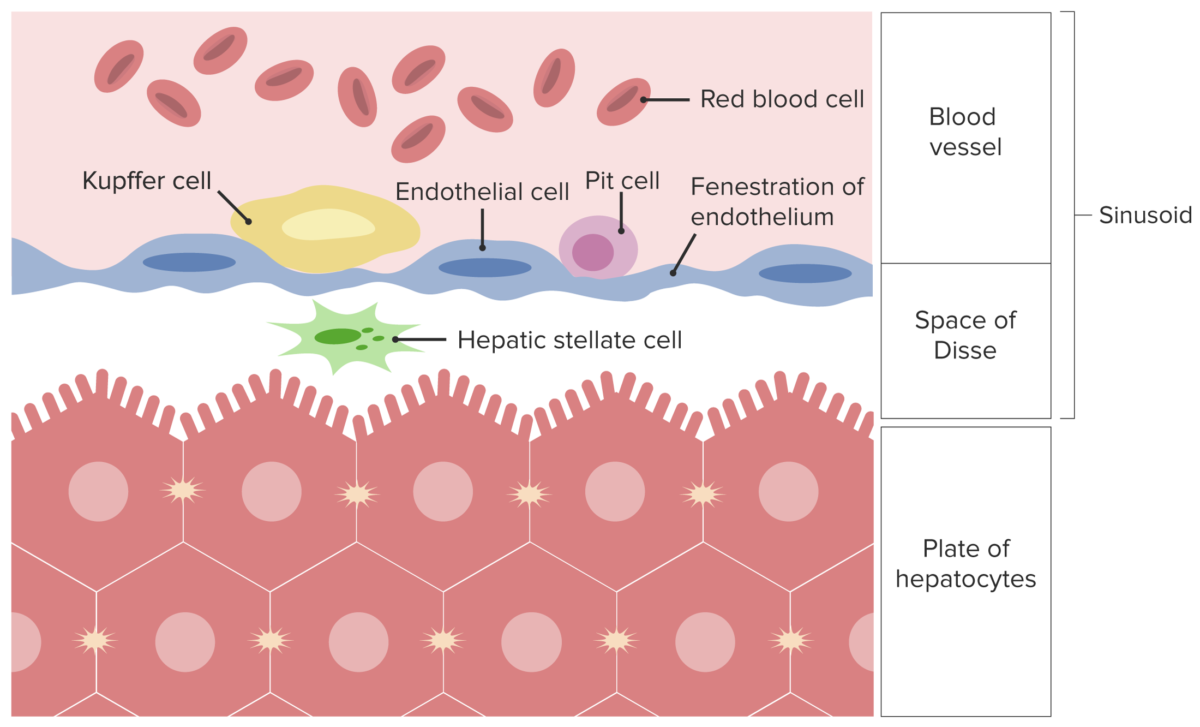
Schematic representation of a sinusoid and plate of hepatocytes separated by the space of Disse. Note the specialized cells of the liver: Kupffer, Pit, and Stellate cells.
Image by Lecturio.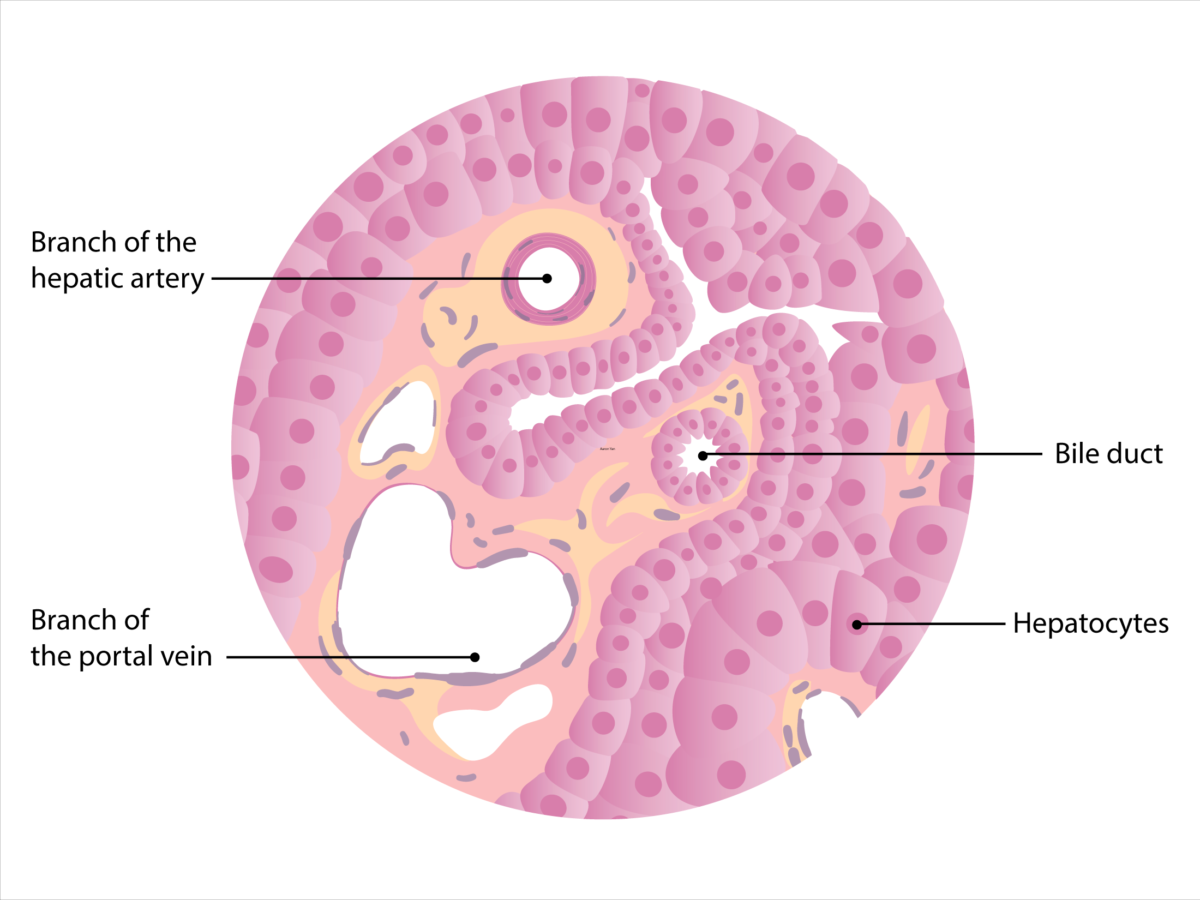
Schematic diagram of the histology of the liver. Note that the branch of the portal vein can be identified by the wide lumen and thin wall of smooth muscle cells. The branch of the hepatic artery has a smaller caliber surrounded by a thicker layer of smooth muscle. The walls of the bile duct contain cuboid-shaped epithelial cells (cholangiocytes), which distinguish it from the hepatic artery.
Image by Lecturio.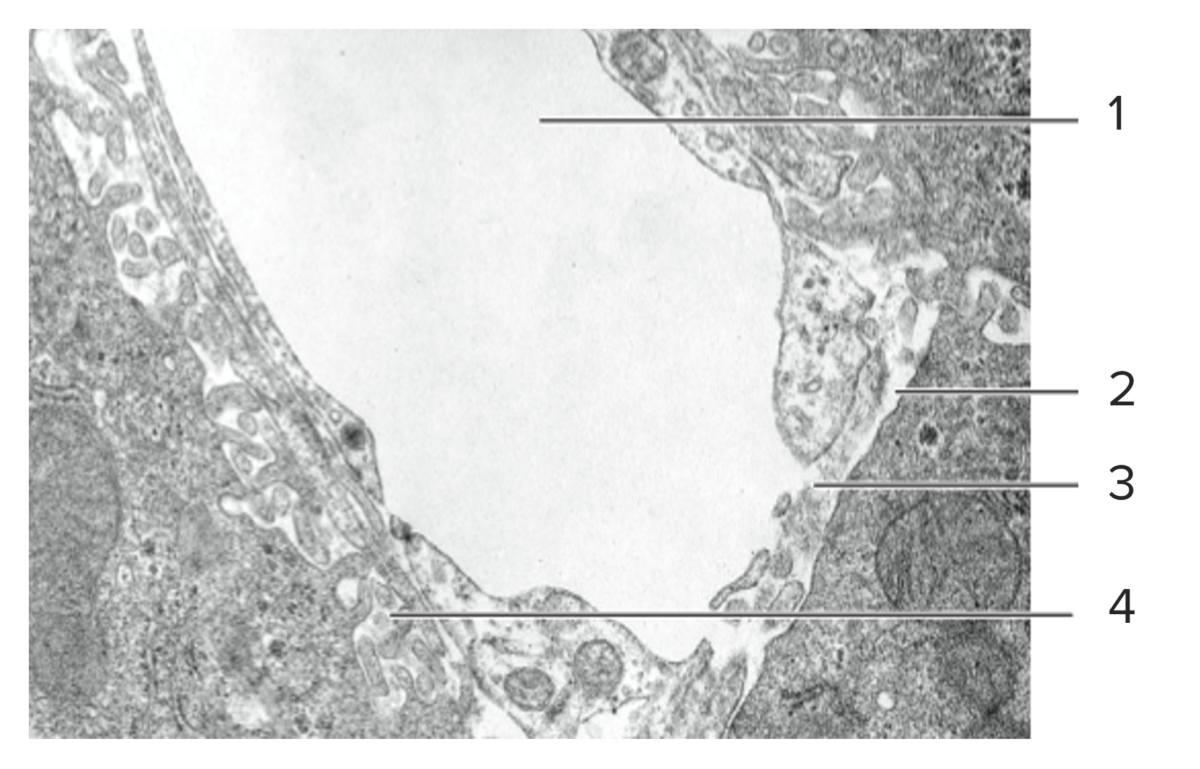
Histological cut of hepatic tissue, featuring a sinusoid (1), its discontinuous basal lamina (2), fenestrated endothelium (3), and the perisinusoidal space of Disse (4).
Image by Lecturio.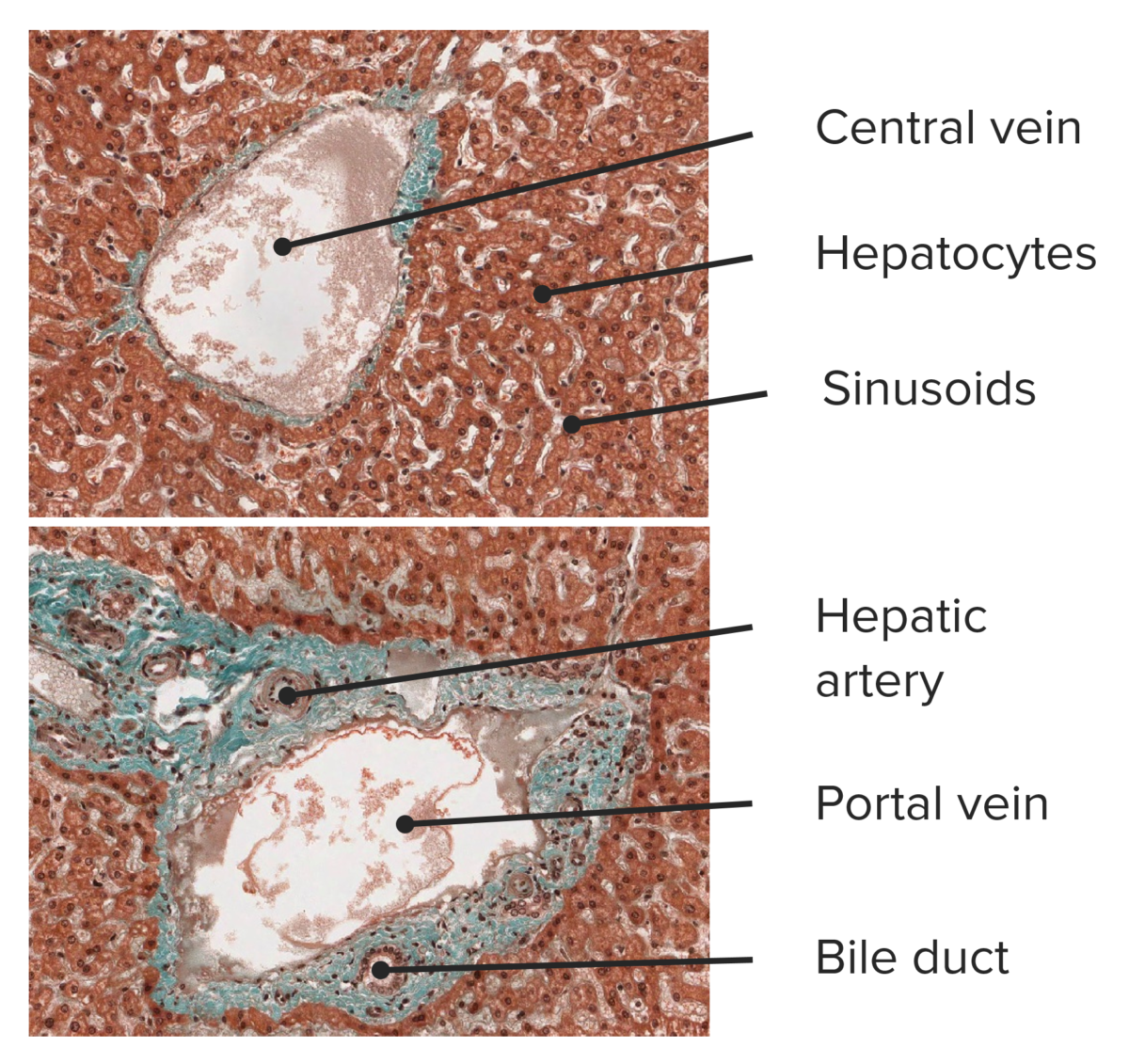
Histological cut of hepatic tissue, featuring a central vein (top) and a portal triad (bottom).
Image by Lecturio.The liver has a special dual blood supply that provides a mix of oxygenated, deoxygenated, and nutrient-rich blood.
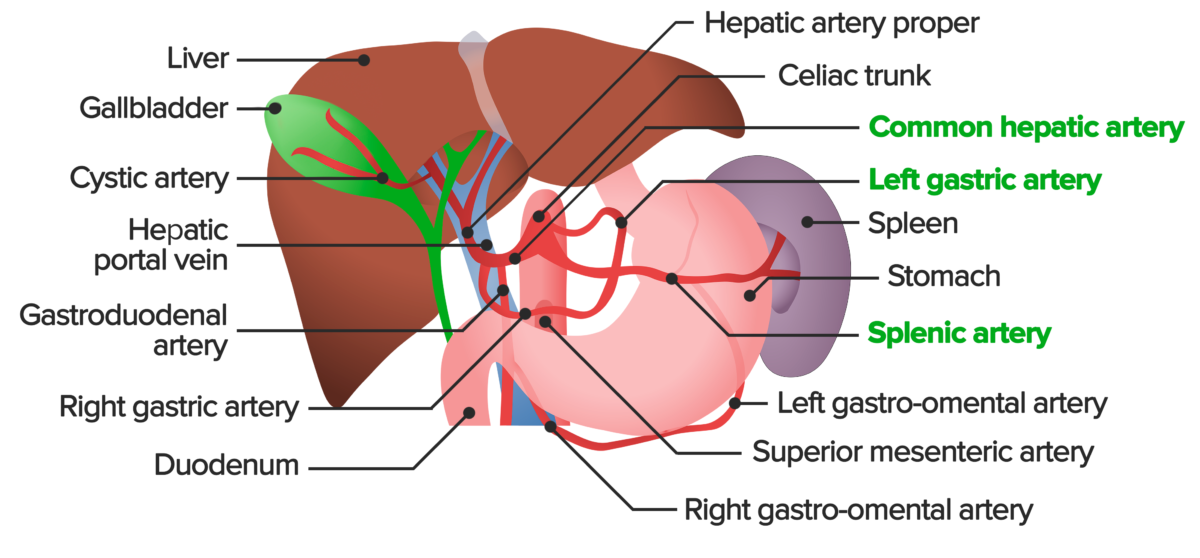
Overview of the abdominal arterial blood supply. The celiac trunk is the 1st major branch of the abdominal aorta. It supplies the liver, stomach, spleen, pancreas, and parts of the esophagus and duodenum with oxygenated blood. The celiac trunk gives off the left gastric artery, splenic artery, and the common hepatic artery. The common hepatic artery divides into the hepatic artery proper, gastroduodenal artery, and right gastric artery, all of which can be seen here.
Image by Lecturio.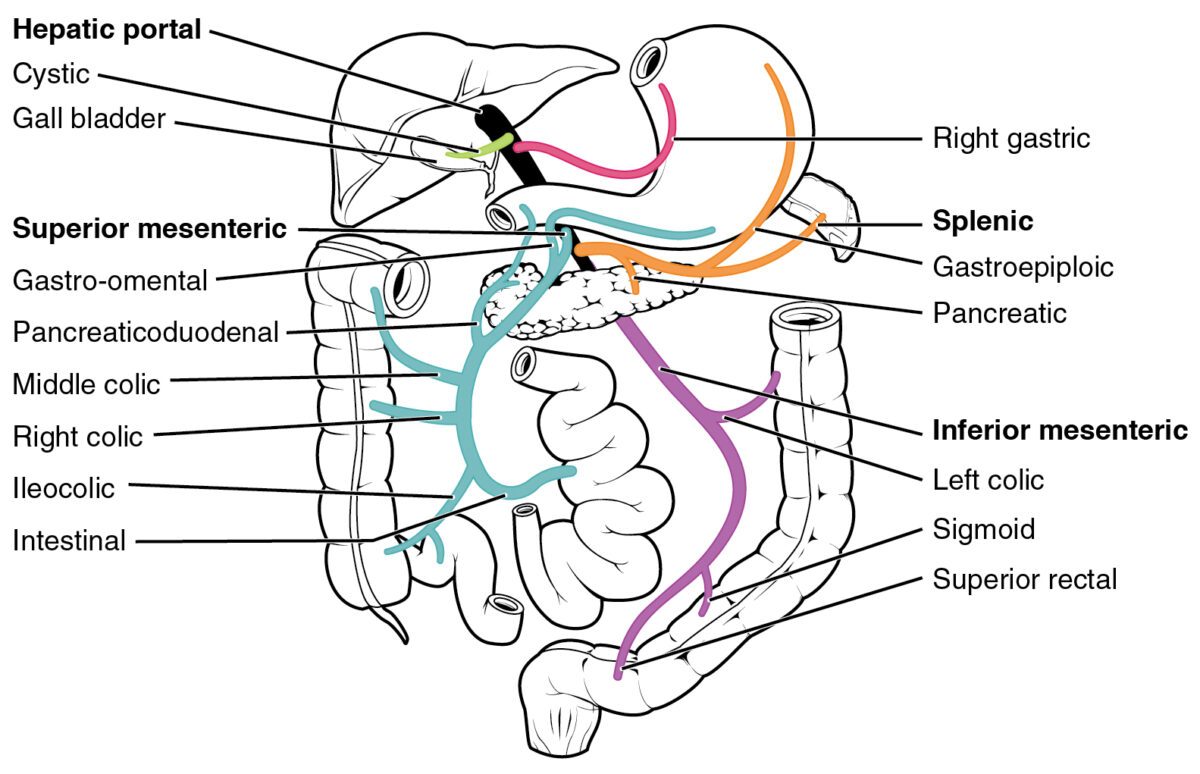
Diagram of the venous portal system. The hepatic portal vein is formed most commonly by the union of the splenic vein and superior mesenteric veins. Other tributaries include the inferior mesenteric, cystic, and the left and right gastric veins. As a whole, the portal system collects the venous drainage of the spleen, stomach, gallbladder, small and large intestines, and pancreas.
Image: “Hepatic Portal Vein System” by OpenStax College. License: CC BY 3.0Hepatic lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy: located around the porta hepatis → celiac cluster of lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy → cisterna chyli (dilated sac that receives lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs from the gastrointestinal [GI] trunk and 2 lumbar lymphatic trunks) → thoracic duct Thoracic Duct The largest lymphatic vessel that passes through the chest and drains into the subclavian vein. Lymphatic Drainage System: Anatomy
Bile canaliculi Bile Canaliculi Minute intercellular channels that occur between liver cells and carry bile towards interlobar bile ducts. Also called bile capillaries. Gallbladder and Biliary Tract: Anatomy → intrahepatic bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy ducts → left and right hepatic ducts → common hepatic duct → common bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy duct → duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy
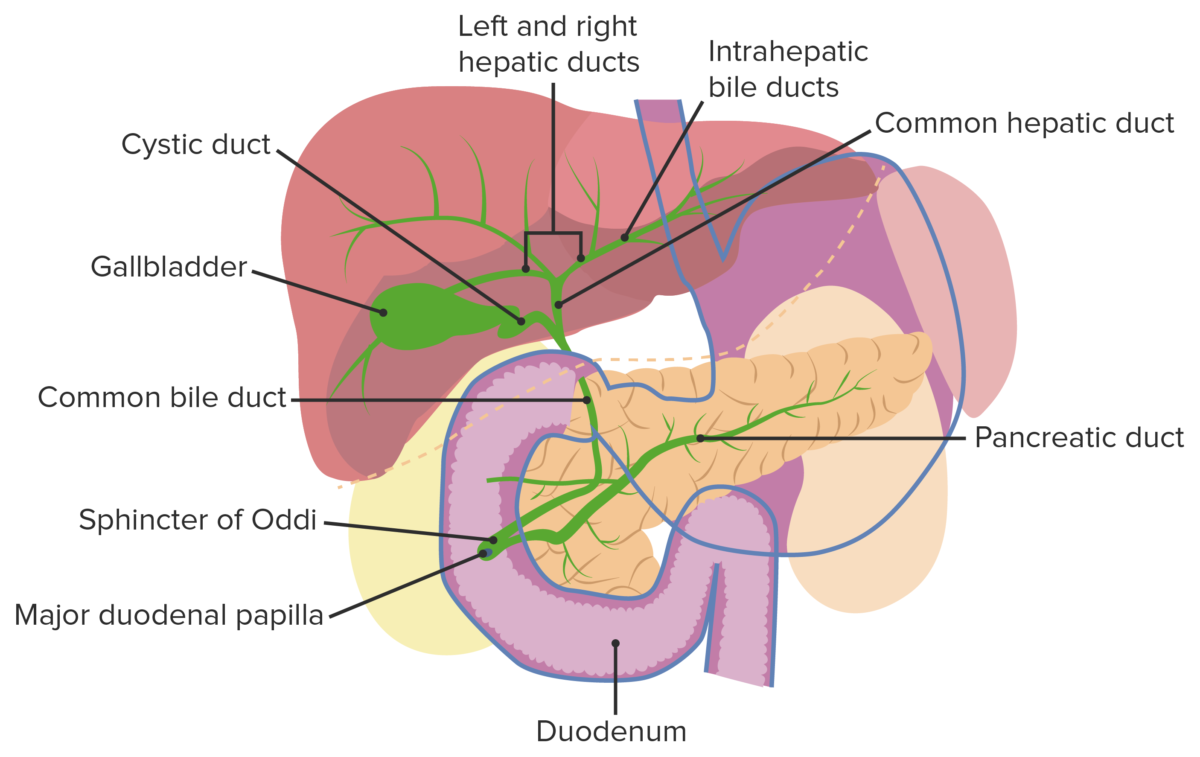
Gallbladder and biliary tract
Image by Lecturio.The liver eliminates degradation products obtained via resorption from the GI tract. It makes fat-soluble substances water-soluble through enzymatic modification. This allows for excretion via biliary tracts or through urine.
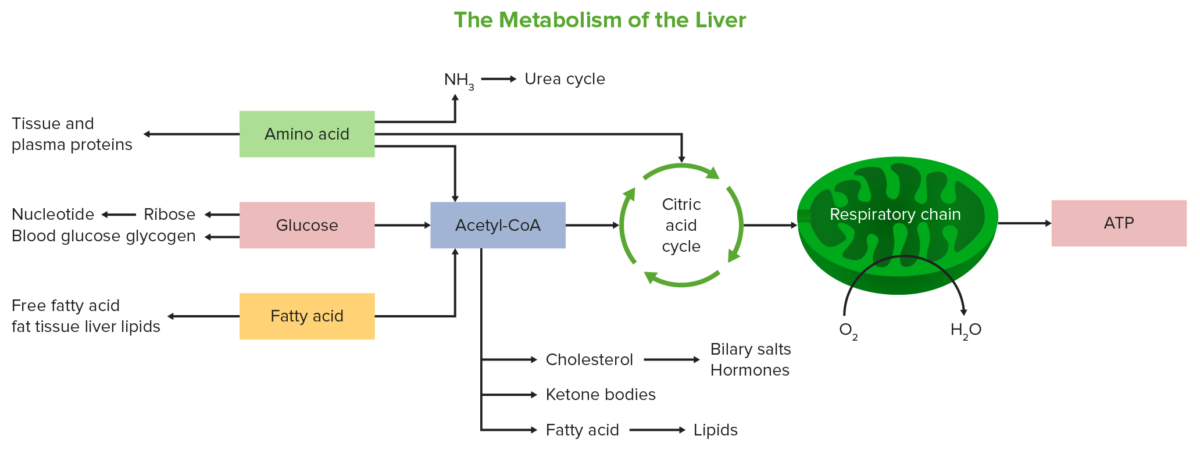
Schematic diagram showing the various metabolic pathways the liver is involved in
Image by Lecturio.Neoplasms Neoplasms New abnormal growth of tissue. Malignant neoplasms show a greater degree of anaplasia and have the properties of invasion and metastasis, compared to benign neoplasms. Benign Bone Tumors
Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease
Inflammatory disorders
Hereditary disorders
Miscellaneous disorders