Hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension (HTN) is one of the most common chronic medical conditions in the world, affecting one-third to one-half of the population, depending on the definition used for HTN. The current definition of HTN in the USA is a systolic blood pressure ( SBP SBP Ascites) of ≥130 mm Hg and/or a diastolic blood pressure (DBP) of ≥80 mm Hg, [1][2] but most countries continue to use ≥140/90 mm Hg as the definition for reasons discussed later.[3] The prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of HTN increases with age and sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria (men > women). Most people with HTN do not have adequate blood pressure control, even in high-income countries,[4] but this is particularly evident in low and middle-income countries, where BP control is often very low, and many hypertensives remain undiagnosed. Hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is a major risk factor for multiple diseases, including strokes, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease, and acute and chronic kidney disease Chronic Kidney Disease Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease. It is considered to be a major public health failure that many millions of people in the world with hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension are not receiving the treatment that they need, since the condition is easy to diagnose and can be treated with low-cost drugs. Three large studies in lower income countries have shown a dramatic decrease in cardiovascular disease by providing a combination pill (a “polypill,” including atorvastatin Atorvastatin A pyrrole and heptanoic acid derivative, hydroxymethylglutaryl-CoA reductase inhibitor (statin), and anticholesteremic agent that is used to reduce serum levels of ldl-cholesterol; apolipoprotein b; and triglycerides. It is used to increase serum levels of hdl-cholesterol in the treatment of hyperlipidemias, and for the prevention of cardiovascular diseases in patients with multiple risk factors. Statins, hydrochlorothiazide Hydrochlorothiazide A thiazide diuretic often considered the prototypical member of this class. It reduces the reabsorption of electrolytes from the renal tubules. This results in increased excretion of water and electrolytes, including sodium, potassium, chloride, and magnesium. It is used in the treatment of several disorders including edema, hypertension, diabetes insipidus, and hypoparathyroidism. Thiazide Diuretics, either enalapril Enalapril An angiotensin-converting enzyme inhibitor that is used to treat hypertension and heart failure. Hypertension Drugs or valsartan Valsartan A tetrazole derivative and angiotensin II type 1 receptor blocker that is used to treat hypertension. Hypertension Drugs, and with or without aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs)) to those over 50 years of age (in the PolyIran study), regardless of cardiovascular risk factors.[5-7] In the United States, hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension management is one of the most common reasons for medical office visits.[8]. TIP FOR THE USMLE: This is a high-yield topic because it has the four key elements of a high-yield disease or condition: it is common, serious, diagnosable, and treatable. For further review of this topic, including links to lectures by specialists in the field, follow this link: https://www.lecturio.com/concepts/hypertension/
Last updated: Sep 12, 2024
Authors: Ahmed Elsherif 1 ; Michelle Wyatt 2
Peer Reviewers: Stanley Oiseth 3 ; Joseph Alpert 4
Affiliations: 1 Suez Canal University; 2 Medical Editor at Lecturio; 3 Chief Medical Editor at Lecturio; 4 Tucson University, Arizona
This article is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition.
A person who has an actual measured high blood pressure and/or is taking antihypertensive medication is considered to have HTN.[1] In 2019, a global study using ≥140/90 mm Hg as the definition of HTN found that the prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of HTN in adults aged 30–79 years was 32% in women and 34% in men, which was similar to the 1990 levels. These percentages would have increased to an average of approximately 45% if the 2017 ACC/AHA lower cutoff level of ≥130/80 had been used, signifying a global burden of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension of at least 1.8 billion people.[2] The prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of HTN increases with age (70% of adults ≥65 years have hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension[13] and body weight. In the United States, the prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency is higher in Blacks than in Whites or Hispanics, and also higher in rural than in urban environments. Most people with HTN do not have adequate blood pressure control, even in high-income countries, but this is particularly pronounced in low and middle-income countries, where BP control is often very low, and many hypertensives remain undiagnosed. In high-income countries, only 37% of men and 43% of women have their HTN under control, while these percentages drop to 9% for men and 13% for women in sub-Saharan Africa and Oceania.
Systemic arterial hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension (HTN) is divided into two types: primary hypertension Primary hypertension Hypertension that occurs without known cause, or preexisting renal disease. Associated polymorphisms for a number of genes have been identified, including agt, gnb3, and ece1. Hypertension (also known as “essential hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension” because at one time it was believed the high pressure was necessary to keep the vital organs perfused); and secondary hypertension Secondary hypertension Hypertension.[14-16]
This is hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension of unknown cause. Depending on the diagnostic method used, approximately 80–95% of hypertensive patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship have PH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance, which is really the final manifestation of different underlying pathophysiologies. 60–70% of PH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance in adults has been attributed to being overweight or obese. Peripheral vascular resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing (PVR) is increased, and cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics is normal or decreased in most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with long-standing PH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance; however, in younger patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, the PVR may be normal, with increased cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics. Plasma renin activity Plasma renin activity Renal Artery Stenosis ( PRA PRA Purine and Pyrimidine Metabolism) is increased in approximately 10–15% of individuals with PH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance (called “vasoconstrictor type” of HTN), while PRA PRA Purine and Pyrimidine Metabolism is decreased in ~ 25% (called “volume-dependent” or “low-renin hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension;” which is more common in African Americans). These underlying mechanisms help explain why not all PH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship have the same response to the same medication: a person with high-renin HTN would likely respond to a vasodilator, and a low-renin HTN patient would likely respond to an aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia antagonist like spironolactone Spironolactone A potassium sparing diuretic that acts by antagonism of aldosterone in the distal renal tubules. It is used mainly in the treatment of refractory edema in patients with congestive heart failure, nephrotic syndrome, or hepatic cirrhosis. Its effects on the endocrine system are utilized in the treatments of hirsutism and acne but they can lead to adverse effects. Potassium-sparing Diuretics since aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia tends to be elevated in low-renin conditions.
The risk factors associated with primary hypertension Primary hypertension Hypertension that occurs without known cause, or preexisting renal disease. Associated polymorphisms for a number of genes have been identified, including agt, gnb3, and ece1. Hypertension are:[17]
The mechanism of renovascular hypertension Renovascular hypertension Hypertension due to renal artery obstruction or compression. Renal Artery Stenosis is mainly due to renal ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage. Renal artery Renal artery A branch of the abdominal aorta which supplies the kidneys, adrenal glands and ureters. Glomerular Filtration stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) results in an increased level of renin Renin A highly specific (leu-leu) endopeptidase that generates angiotensin I from its precursor angiotensinogen, leading to a cascade of reactions which elevate blood pressure and increase sodium retention by the kidney in the renin-angiotensin system. Renal Sodium and Water Regulation and angiotensin I and II. These are associated with increased vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure, hence, hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension and an increased sympathetic tone. Aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia production is also increased in these patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship which results in increased retention of sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia. The increased retention of sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia is associated with increased water retention and can lead to extracellular blood volume. The interplay between these 2 mechanisms is the main cause of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension in this group of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.

Patient with Cushing syndrome due to hypercortisolism showing moon face
Image: “Patient’s facial appearance” by Ozlem Celik et al. License: CC BY 2.5 , edited by Lecturio
Digital subtraction angiogram in a 35-year-old woman with uncontrolled hypertension demonstrates contiguous relative stenoses alternating with fusiform aneurysmal dilatation of the right renal artery due to fibromuscular dysplasia resembling a string of beads (inset). Fibromuscular dysplasia is characterized by fibrous or muscular hyperplasia in one or more layers of the renal artery wall, producing this appearance.
Image: “Fig. 15” by Bryan Buckley et al. License: CC BY 4.0Another type of arterial hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is hypertensive disease of pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care. Risk factors include increasing maternal age and multifetal pregnancies.
Hypertensive disorders of pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care are divided into:
Blood is delivered to the tissues and flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure occurs because of the pressure difference established by the pumping action of the heart. This relation between the pressure difference and the flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure can be described by the important equation: MAP = CO x PVR, where MAP = mean arterial pressure Mean Arterial Pressure Mean arterial pressure (MAP) is the average systemic arterial pressure and is directly related to cardiac output (CO) and systemic vascular resistance (SVR). The SVR and MAP are affected by the vascular anatomy as well as a number of local and neurohumoral factors. Vascular Resistance, Flow, and Mean Arterial Pressure (= diastolic pressure + ⅓ [systolic pressure – diastolic pressure]), CO = cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics (= stroke volume Stroke volume The amount of blood pumped out of the heart per beat, not to be confused with cardiac output (volume/time). It is calculated as the difference between the end-diastolic volume and the end-systolic volume. Cardiac Cycle x heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology), and PVR = total peripheral resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing. At its basic level, this equation emphasizes that an elevation of mean blood pressure can only occur if there is an increase in cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics (CO), an increase in total peripheral vascular resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing (PVR), or a combination of both. The main factors which determine blood pressure are the sympathetic nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification, the renin-angiotensin-aldosterone system Renin-angiotensin-aldosterone system A blood pressure regulating system of interacting components that include renin; angiotensinogen; angiotensin converting enzyme; angiotensin i; angiotensin ii; and angiotensinase. Renin, an enzyme produced in the kidney, acts on angiotensinogen, an alpha-2 globulin produced by the liver, forming angiotensin I. Angiotensin-converting enzyme, contained in the lung, acts on angiotensin I in the plasma converting it to angiotensin II, an extremely powerful vasoconstrictor. Angiotensin II causes contraction of the arteriolar and renal vascular smooth muscle, leading to retention of salt and water in the kidney and increased arterial blood pressure. In addition, angiotensin II stimulates the release of aldosterone from the adrenal cortex, which in turn also increases salt and water retention in the kidney. Angiotensin-converting enzyme also breaks down bradykinin, a powerful vasodilator and component of the kallikrein-kinin system. Adrenal Hormones, and the plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products volume, which is mostly regulated by the kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy. Increased peripheral vascular resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing (PVR) is the hallmark of established hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, but altered cardiac function also probably contributes to the raised blood pressure.[18] An increase in calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes intake slightly reduces both systolic and diastolic blood pressure in normotensive people, indicating a possible role in the prevention of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension.[19] The underlying pathogenesis of primary hypertension Primary hypertension Hypertension that occurs without known cause, or preexisting renal disease. Associated polymorphisms for a number of genes have been identified, including agt, gnb3, and ece1. Hypertension is not well-understood, but many genetic and environmental factors are involved.
Most people with hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension have no signs or symptoms, even with severe HTN; that is why it is often called “the silent killer.” Some people with severe HTN may have non-specific signs and symptoms, including headaches, shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, nosebleeds Nosebleeds Bleeding from the nose. Granulomatosis with Polyangiitis, fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia, confusion, vision Vision Ophthalmic Exam alterations, chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, palpitations Palpitations Ebstein’s Anomaly, or hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma.
Special forms of arterial hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension are isolated office hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension and isolated ambulatory hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension.[1]
1. White-coat hypertension White-coat hypertension Phenomenon where blood pressure readings are elevated only when taken in clinical settings. Hypertension (“White-coat effect”)
2. Isolated systolic hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension:
3. Masked hypertension Masked hypertension Phenomenon where increased blood pressure readings taken in non-clinical settings (e.g., home blood pressure monitoring) do not replicate in clinical settings. Hypertension: This is BP that is consistently elevated by out-of-office measurements but normal at the office.
Gathering a patient’s medical history is essential because it helps to discover risk factors, previous blood pressure measurements, and symptoms referable to hypertensive-related target organ damage, including ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease, cerebrovascular disease, and chronic kidney disease Chronic Kidney Disease Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease. It is very important to ask patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship about their current medications, previous illnesses, and family history Family History Adult Health Maintenance.
The patient’s physical examination should include checking the radial and the femoral pulses and performing abdominal auscultation Abdominal Auscultation Abdominal Examination which may help identify a bruit associated with renal artery Renal artery A branch of the abdominal aorta which supplies the kidneys, adrenal glands and ureters. Glomerular Filtration stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), although this is not a sensitive test for RAS RAS Renal artery stenosis (RAS) is the narrowing of one or both renal arteries, usually caused by atherosclerotic disease or by fibromuscular dysplasia. If the stenosis is severe enough, the stenosis causes decreased renal blood flow, which activates the renin-angiotensin-aldosterone system (RAAS) and leads to renovascular hypertension (RVH). Renal Artery Stenosis.
Furthermore, it is essential to look for signs of heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) and left ventricular hypertrophy Ventricular Hypertrophy Tetralogy of Fallot. The fundi of the eyes should be examined as well to evaluate for possible hypertensive retinopathy Retinopathy Degenerative changes to the retina due to hypertension. Alport Syndrome, which will show progressively severe changes ranging from mild arteriolar narrowing → focal arteriovenous nicking Arteriovenous Nicking Hypertensive Retinopathy → retinal hemorrhages and exudates → papilledema Papilledema Swelling of the optic disk, usually in association with increased intracranial pressure, characterized by hyperemia, blurring of the disk margins, microhemorrhages, blind spot enlargement, and engorgement of retinal veins. Chronic papilledema may cause optic atrophy and visual loss. Idiopathic Intracranial Hypertension (grade IV hypertensive retinopathy Retinopathy Degenerative changes to the retina due to hypertension. Alport Syndrome).
Except for diagnostic severe hypertension Severe hypertension A confirmed blood pressure ≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic. Uncontrolled Hypertension ( SBP SBP Ascites ≥180 mm Hg and/or DBP ≥120 mm) or asymptomatic Stage 2 hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who have an elevated office blood pressure should have out-of-office blood pressure measurements for confirmation of the presence of true HTN. Automated and validated oscillometric BP monitors are preferred to stethoscope-based manual methods, both in the office and at home. For home measurements, the patient measures their BP once in the morning and once in the evening for 7 days. The first day of readings and the remaining 12 measurements are averaged. Hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is diagnosed if the mean home BP is ≥130 mm Hg systolic or ≥80 mm Hg diastolic. 24-hour ambulatory blood pressure monitoring (ABPM) is an alternative if adequate home blood pressures cannot be obtained or if there is doubt about the validity Validity Validity refers to how accurate a test or research finding is. Causality, Validity, and Reliability of home readings.
All individuals 18 years or older should be screened for HTN, with annual evaluation for those > 40 years old or those with risk factors for HTN. Younger adults with no risk factors should be evaluated every 3–5 years.
All patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with a new diagnosis of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension should have the following tests:
Extensive evaluation for secondary causes of HTN is not justifiable for all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with primary hypertension Primary hypertension Hypertension that occurs without known cause, or preexisting renal disease. Associated polymorphisms for a number of genes have been identified, including agt, gnb3, and ece1. Hypertension, but rather only a targeted approach is recommended if there is an atypical presentation or there is a clinical clue that a secondary cause may be present.
Non-pharmacological treatment (lifestyle modifications): alone or with antihypertensive drug therapy:
Blood pressure targets are based upon the patient’s risk for having a future cardiovascular event. In general, more aggressive blood pressure goals are indicated for higher-risk patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Treatment approach depends on the blood pressure stage and cardiovascular risk. For most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with stage 2 hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension (≥140/90 mmHg), initial combination therapy with 2 agents is recommended, preferably as single-pill combinations. Initial monotherapy is appropriate for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with stage 1 Stage 1 Trypanosoma brucei/African trypanosomiasis hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension who have cardiovascular risk factors or for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship at higher risk for adverse drug effects.
First-line medications include:
While the above medications are considered as primary antihypertensives Antihypertensives The 1st-line medication classes for hypertension include thiazide-like diuretics, angiotensin-converting enzyme inhibitors (ACEis), angiotensin II receptor blockers (ARBs), and calcium channel blockers (CCBS). Contraindications, adverse effects, and drug-to-drug interactions are agent specific. Hypertension Drugs, they can still be combined.
Preferred Drug Combinations: When combination therapy is indicated, the preferred combination is an ACE inhibitor or ARB with a dihydropyridine Dihydropyridine Pyridine moieties which are partially saturated by the addition of two hydrogen atoms in any position. Class 4 Antiarrhythmic Drugs (Calcium Channel Blockers) calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blocker. An alternative is an ACE inhibitor or ARB with a thiazide-like diuretic ( chlorthalidone Chlorthalidone A benzenesulfonamide-phthalimidine that tautomerizes to a benzophenones form. It is considered a thiazide-like diuretic. Thiazide Diuretics or indapamide Indapamide A benzamide-sulfonamide-indole derived diuretic that functions by inhibiting sodium chloride symporters. Hypertension Drugs preferred over hydrochlorothiazide Hydrochlorothiazide A thiazide diuretic often considered the prototypical member of this class. It reduces the reabsorption of electrolytes from the renal tubules. This results in increased excretion of water and electrolytes, including sodium, potassium, chloride, and magnesium. It is used in the treatment of several disorders including edema, hypertension, diabetes insipidus, and hypoparathyroidism. Thiazide Diuretics).
Secondary antihypertensives Antihypertensives The 1st-line medication classes for hypertension include thiazide-like diuretics, angiotensin-converting enzyme inhibitors (ACEis), angiotensin II receptor blockers (ARBs), and calcium channel blockers (CCBS). Contraindications, adverse effects, and drug-to-drug interactions are agent specific. Hypertension Drugs are used when primary medications do not work or when there are special indications such as in hypertensive patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who also have ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease.
Secondary antihypertensives Antihypertensives The 1st-line medication classes for hypertension include thiazide-like diuretics, angiotensin-converting enzyme inhibitors (ACEis), angiotensin II receptor blockers (ARBs), and calcium channel blockers (CCBS). Contraindications, adverse effects, and drug-to-drug interactions are agent specific. Hypertension Drugs include:
Primary sites of action [20]
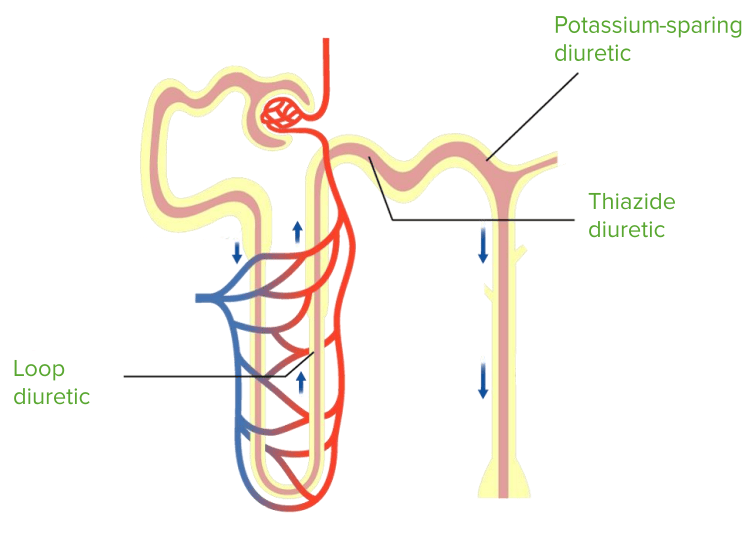
Sites of action of common diuretics used in the treatment of hypertension.
Image by Lecturio.Thiazide Thiazide Heterocyclic compounds with sulfur and nitrogen in the ring. This term commonly refers to the benzothiadiazines that inhibit sodium-potassium-chloride symporters and are used as diuretics. Hyponatremia Diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication
Adverse effects (AEs) of thiazide Thiazide Heterocyclic compounds with sulfur and nitrogen in the ring. This term commonly refers to the benzothiadiazines that inhibit sodium-potassium-chloride symporters and are used as diuretics. Hyponatremia diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication:
Loop Diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication
Adverse effects of loop diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication:
Antihypertensive Drugs: Hemodynamic Mechanism of BP Reduction
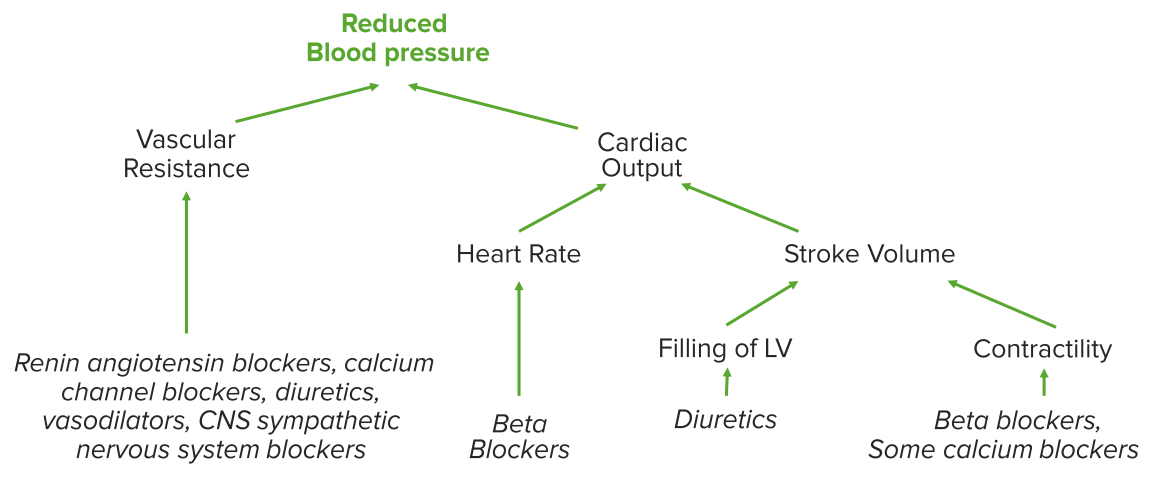
Mechanisms of action of various anti-hypertensive drugs. Different classes of medications decrease blood pressure by decreasing the influence of one or more of the different factors that contribute to maintain arterial pressure. Cardiac output and peripheral vascular resistance the two determinants of arterial pressure. Cardiac output = stroke volume x heart rate, and stroke volume depends on myocardial contractility and the volume of the vascular compartment. Peripheral resistance is determined by the functional and anatomic changes in small arteries (lumen diameters of 100-400 μm) and arterioles. With reference to the diagram above, for example, angiotensin converting enzyme (ACE) blocks the conversion of angiotensin I to angiotensin II (a powerful vasoconstrictor), so peripheral vascular resistance is decreased. Beta blockers decrease heart rate (and myocardial contractility), thereby decreasing the stroke volume and the cardiac output. Diuretics decrease the vascular volume, at least in the short term, which decreases LV filling (so the stroke volume is decreased), and some (e.g., hydrochlorothiazide) may also act as vasodilators in the long term. Some calcium channel blockers decrease contractility, which decreases stroke volume.
Image by Lecturio.Renin-angiotensin Aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia System
The kidney is central to blood pressure control through the juxtaglomerular apparatus. Baroreceptors Baroreceptors Receptors in the vascular system, particularly the aorta and carotid sinus, which are sensitive to stretch of the vessel walls. Arginine Vasopressin Disorders (Diabetes Insipidus) in the arterial system inform the central nervous system Central nervous system The main information-processing organs of the nervous system, consisting of the brain, spinal cord, and meninges. Nervous System: Anatomy, Structure, and Classification about the level of blood pressure. The signals from baroreceptors Baroreceptors Receptors in the vascular system, particularly the aorta and carotid sinus, which are sensitive to stretch of the vessel walls. Arginine Vasopressin Disorders (Diabetes Insipidus) lead to changes in autonomic nervous system Autonomic nervous system The ANS is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ANS consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy activity. Renin Renin A highly specific (leu-leu) endopeptidase that generates angiotensin I from its precursor angiotensinogen, leading to a cascade of reactions which elevate blood pressure and increase sodium retention by the kidney in the renin-angiotensin system. Renal Sodium and Water Regulation initiates a biochemical sequence that eventually converts angiotensinogen produced in the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy into angiotensin, a strong vasoconstrictor. Angiotensin stimulates release of aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia from the adrenal gland which causes the kidney to retain salt (NaCl) and water. Angiotensin stimulates the release of antidiuretic hormone Antidiuretic hormone Antidiuretic hormones released by the neurohypophysis of all vertebrates (structure varies with species) to regulate water balance and osmolarity. In general, vasopressin is a nonapeptide consisting of a six-amino-acid ring with a cysteine 1 to cysteine 6 disulfide bridge or an octapeptide containing a cystine. All mammals have arginine vasopressin except the pig with a lysine at position 8. Vasopressin, a vasoconstrictor, acts on the kidney collecting ducts to increase water reabsorption, increase blood volume and blood pressure. Hypernatremia from the pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland which causes the kidney to retain water.
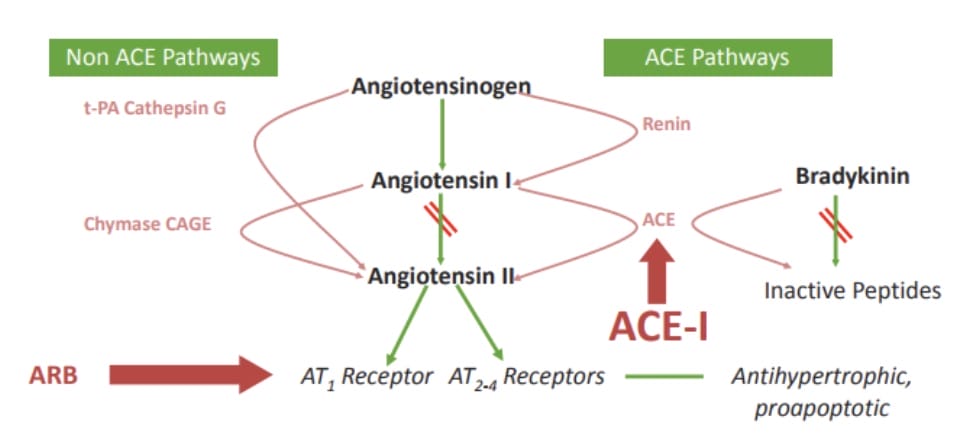
Diagram showing the renin-angiotensin system and related molecules. Many molecules are involved. Angiotensin-converting enzyme inhibitors (ACEIs) inhibit the conversion of angiotensin I to angiotensin II, which can still be produced by enzymes in the non-ACE pathway, such as tissue plasminogen activator (t-PA), cathepsin G, chymase, and chymostatin-sensitive angiotensin II-generating enzyme (CAGE). ACEIs also raise the levels of bradykinin, which provides potent and important cardioprotective benefits, by inhibiting its degradation. One disadvantage of ACEIs is that the presence of non-ACE pathways results in continued low-level production of angiotensin II, despite the inhibition of ACE. Angiotensin II type 1 receptor blockers (ARBs) are selective ligands of AT1 receptors; these drugs can bypass the limitations of ACE escape phenomena and non-ACE sources of angiotensin II formation.
Image by Lecturio.This system is part of the body’s defenses against dehydration Dehydration The condition that results from excessive loss of water from a living organism. Volume Depletion and Dehydration and/or blood loss. The purpose is to restore blood volume to normal as quickly as possible.
Angiotensin-converting enzyme inhibitors Angiotensin-converting enzyme inhibitors A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Renin-Angiotensin-Aldosterone System Inhibitors ( ACEis ACEIs A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Heart Failure and Chronic Coronary Syndrome Medication) and angiotensin receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blockers ( ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Chronic Coronary Syndrome Medication) include:
AE’s with ACEis ACEIs A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Heart Failure and Chronic Coronary Syndrome Medication and ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Chronic Coronary Syndrome Medication — 1st line Rx
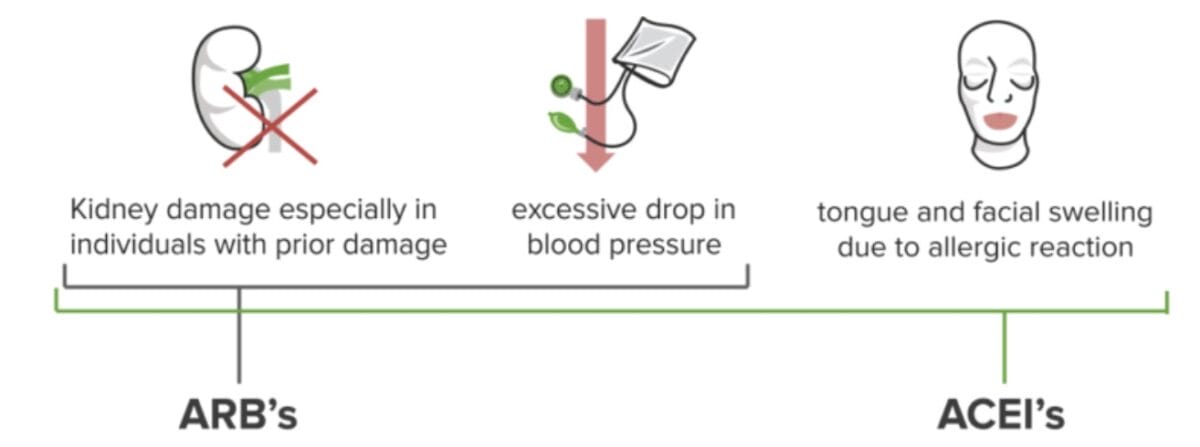
Possible adverse effects of ACE inhibitors and ARBs
Image by Lecturio.Aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia Inhibitors: Spironolactone Spironolactone A potassium sparing diuretic that acts by antagonism of aldosterone in the distal renal tubules. It is used mainly in the treatment of refractory edema in patients with congestive heart failure, nephrotic syndrome, or hepatic cirrhosis. Its effects on the endocrine system are utilized in the treatments of hirsutism and acne but they can lead to adverse effects. Potassium-sparing Diuretics and Eplerenone Eplerenone A spironolactone derivative and selective aldosterone receptor antagonist that is used in the management of hypertension and congestive heart failure, post-myocardial infarction. Potassium-sparing Diuretics
Spironolactone Spironolactone A potassium sparing diuretic that acts by antagonism of aldosterone in the distal renal tubules. It is used mainly in the treatment of refractory edema in patients with congestive heart failure, nephrotic syndrome, or hepatic cirrhosis. Its effects on the endocrine system are utilized in the treatments of hirsutism and acne but they can lead to adverse effects. Potassium-sparing Diuretics. However, eplerenone Eplerenone A spironolactone derivative and selective aldosterone receptor antagonist that is used in the management of hypertension and congestive heart failure, post-myocardial infarction. Potassium-sparing Diuretics is less potent and often requires twice-daily dosing (at 50 to 100 mg) to be as effective for blood pressure lowering. An eplerenone Eplerenone A spironolactone derivative and selective aldosterone receptor antagonist that is used in the management of hypertension and congestive heart failure, post-myocardial infarction. Potassium-sparing Diuretics dose of 50 mg once daily can be prescribed as an initial trial, with dose and frequency escalations undertaken as needed to achieve blood pressure control.
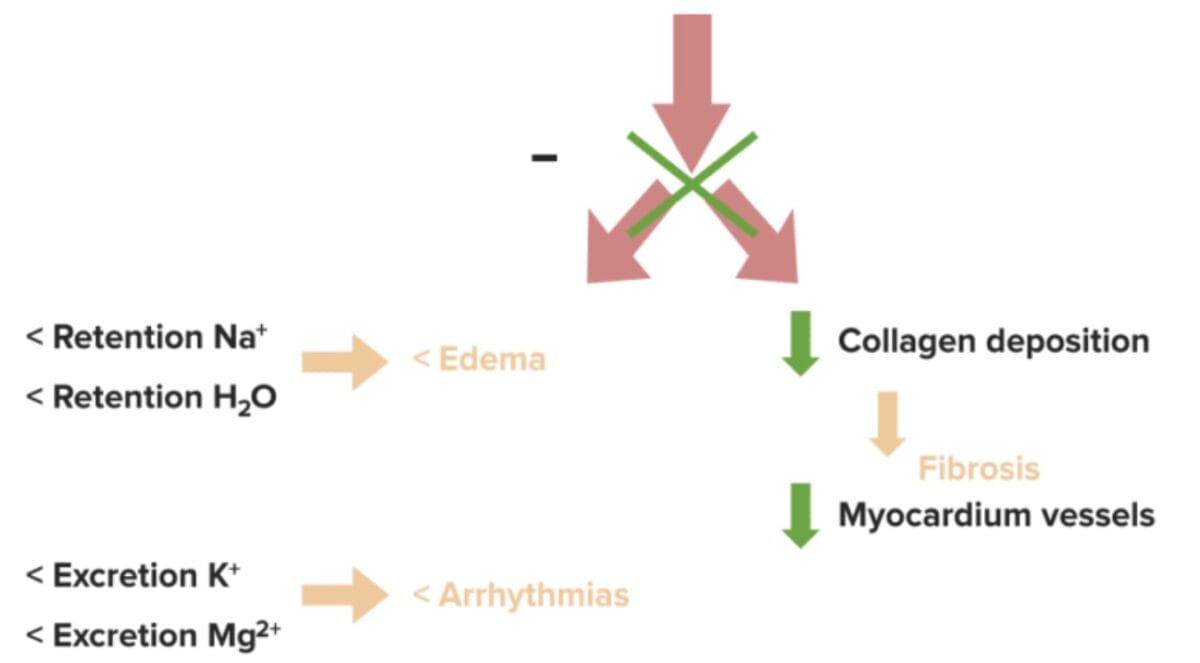
Diagram showing the cardioprotective effects of aldosterone inhibitors. The red arrow at the top represents inhibited aldosterone, and the green “X” at the tip of the arrow represents its inhibition, which leads to (in the left column) decreased retention of sodium and water, and therefore less edema, and decreased excretion of potassium and magnesium, thereby reducing the risk of arrhythmias. The right column shows that there is less collagen (i.e., less fibrosis) and pathologic remodeling of the myocardium and vessels in the presence of an aldosterone inhibitor because aldosterone is a potent inducer of inflammation and oxidative stress which lead to fibrosis (the final manifestation of inflammation).
Image by Lecturio.Adverse effects of aldosterone antagonists Aldosterone antagonists Drugs that bind to and block the activation of mineralocorticoid receptors by mineralocorticoids such as aldosterone. Heart Failure and Chronic Coronary Syndrome Medication
Beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) reduce cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics and decrease renin Renin A highly specific (leu-leu) endopeptidase that generates angiotensin I from its precursor angiotensinogen, leading to a cascade of reactions which elevate blood pressure and increase sodium retention by the kidney in the renin-angiotensin system. Renal Sodium and Water Regulation release by the kidney. They are considered as second-line antihypertensive agents, especially in people > 60 years of age, and include:
Adverse effects:
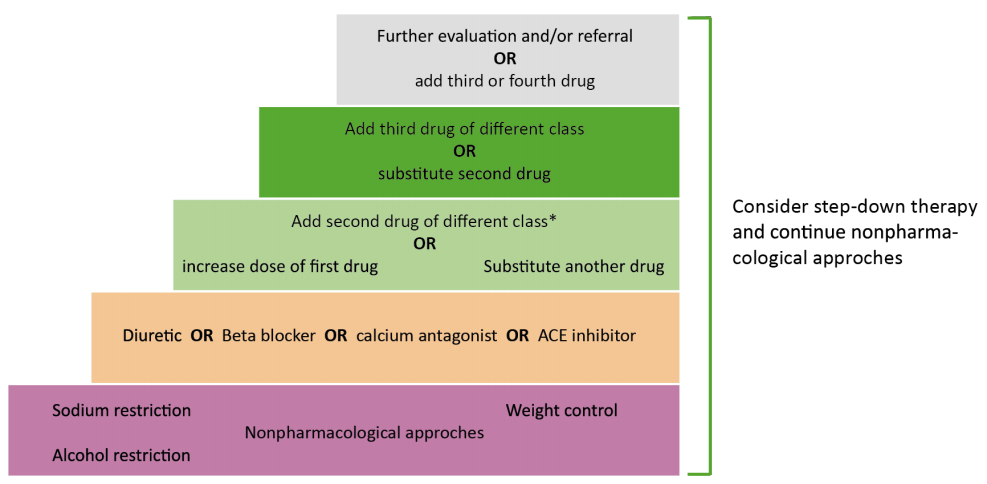
Other therapy in hypertension
Image by Lecturio.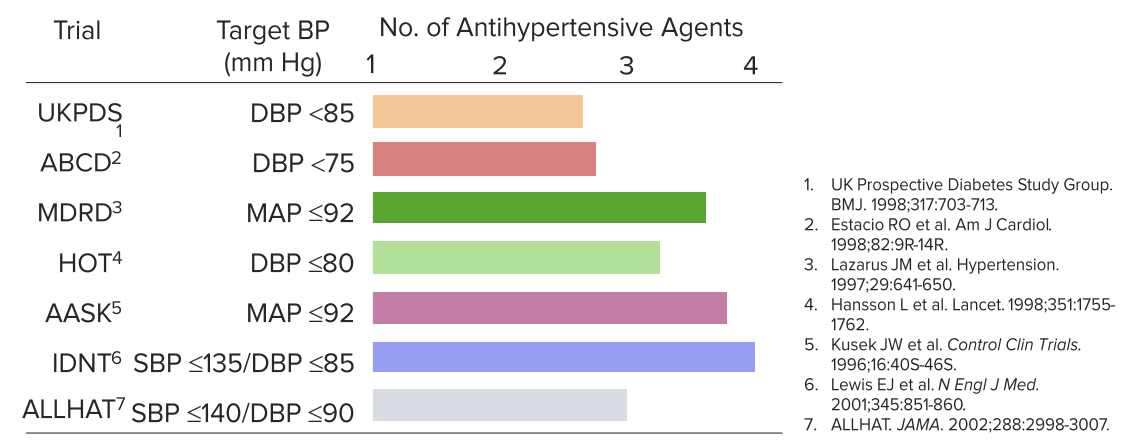
Average number of antihypertensive agents used to achieve target blood pressure
Image by Lecturio.Possible Drug Combinations
Double combination options consist of administering a diuretic in combination with a beta-blocker, a long-acting calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blocker, ACE inhibitors ACE inhibitors Truncus Arteriosus, or ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Chronic Coronary Syndrome Medication.
An alternative is the combination of a calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blocker with a beta-blocker, ACE inhibitors ACE inhibitors Truncus Arteriosus (OR ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Chronic Coronary Syndrome Medication). Never use an ACE inhibitor ( ACEI ACEi A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Renin-Angiotensin-Aldosterone System Inhibitors) and an angiotensin receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blocker (ARB) together because their mechanisms target the same pathway, leading to overlapping effects. Both ACEIs ACEIs A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Heart Failure and Chronic Coronary Syndrome Medication and ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Chronic Coronary Syndrome Medication interfere with the renin-angiotensin-aldosterone system Renin-angiotensin-aldosterone system A blood pressure regulating system of interacting components that include renin; angiotensinogen; angiotensin converting enzyme; angiotensin i; angiotensin ii; and angiotensinase. Renin, an enzyme produced in the kidney, acts on angiotensinogen, an alpha-2 globulin produced by the liver, forming angiotensin I. Angiotensin-converting enzyme, contained in the lung, acts on angiotensin I in the plasma converting it to angiotensin II, an extremely powerful vasoconstrictor. Angiotensin II causes contraction of the arteriolar and renal vascular smooth muscle, leading to retention of salt and water in the kidney and increased arterial blood pressure. In addition, angiotensin II stimulates the release of aldosterone from the adrenal cortex, which in turn also increases salt and water retention in the kidney. Angiotensin-converting enzyme also breaks down bradykinin, a powerful vasodilator and component of the kallikrein-kinin system. Adrenal Hormones ( RAAS RAAS A blood pressure regulating system of interacting components that include renin; angiotensinogen; angiotensin converting enzyme; angiotensin i; angiotensin ii; and angiotensinase. Renin, an enzyme produced in the kidney, acts on angiotensinogen, an alpha-2 globulin produced by the liver, forming angiotensin I. Angiotensin-converting enzyme, contained in the lung, acts on angiotensin I in the plasma converting it to angiotensin II, an extremely powerful vasoconstrictor. Angiotensin II causes contraction of the arteriolar and renal vascular smooth muscle, leading to retention of salt and water in the kidney and increased arterial blood pressure. In addition, angiotensin II stimulates the release of aldosterone from the adrenal cortex, which in turn also increases salt and water retention in the kidney. Angiotensin-converting enzyme also breaks down bradykinin, a powerful vasodilator and component of the kallikrein-kinin system. Adrenal Hormones), which regulates blood pressure and fluid balance. Because both classes of drugs aim to reduce the effects of angiotensin II Angiotensin II An octapeptide that is a potent but labile vasoconstrictor. It is produced from angiotensin I after the removal of two amino acids at the c-terminal by angiotensin converting enzyme. The amino acid in position 5 varies in different species. To block vasoconstriction and hypertension effect of angiotensin II, patients are often treated with ace inhibitors or with angiotensin II type 1 receptor blockers. Renal Sodium and Water Regulation, using them together does not provide additional benefits but rather increases the risk of adverse effects like hyperkalemia Hyperkalemia Hyperkalemia is defined as a serum potassium (K+) concentration >5.2 mEq/L. Homeostatic mechanisms maintain the serum K+ concentration between 3.5 and 5.2 mEq/L, despite marked variation in dietary intake. Hyperkalemia can be due to a variety of causes, which include transcellular shifts, tissue breakdown, inadequate renal excretion, and drugs. Hyperkalemia, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, and acute kidney injury Acute Kidney Injury Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury. [24]Investigators involved in three large randomized controlled studies In lower-income countries concluded that fixed-dose combination treatment strategies substantially reduce the incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency of myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, stroke, revascularization Revascularization Thromboangiitis Obliterans (Buerger Disease), and cardiovascular death in primary prevention of cardiovascular disease. These benefits were shown to be consistent irrespective of cardiometabolic risk factors. The combination pills, or polypills, included ≥2 blood pressure-lowering agents plus a statin, with or without aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs).[7] If applied to all the people who live in low and middle-income countries, there would be a dramatic decrease in cardiovascular-related morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and mortality Mortality All deaths reported in a given population. Measures of Health Status, since most people with undiagnosed or uncontrolled hypertension Uncontrolled hypertension Although hypertension is defined as a blood pressure of > 130/80 mm Hg, individuals can present with comorbidities of severe asymptomatic or “uncontrolled” hypertension (≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic) that carries with it a significant risk of morbidity and mortality. Uncontrolled Hypertension live in those countries.[2]
In a study involving nearly 600 hypertensive patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, a four-drug, single-pill combination containing low doses of irbesartan (an angiotensin II Angiotensin II An octapeptide that is a potent but labile vasoconstrictor. It is produced from angiotensin I after the removal of two amino acids at the c-terminal by angiotensin converting enzyme. The amino acid in position 5 varies in different species. To block vasoconstriction and hypertension effect of angiotensin II, patients are often treated with ace inhibitors or with angiotensin II type 1 receptor blockers. Renal Sodium and Water Regulation receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blocker), indapamide Indapamide A benzamide-sulfonamide-indole derived diuretic that functions by inhibiting sodium chloride symporters. Hypertension Drugs (a thiazide-like diuretic), amlodipine Amlodipine A long-acting dihydropyridine calcium channel blocker. It is effective in the treatment of angina pectoris and hypertension. Hypertension Drugs (a calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blocker), and bisoprolol Bisoprolol A cardioselective beta-1 adrenergic blocker. It is effective in the management of hypertension and angina pectoris. Class 2 Antiarrhythmic Drugs (Beta Blockers) (a beta-blocker) was found to reduce 24-hour systolic blood pressure more effectively than a full dose of irbesartan alone (18 mmHg reduction versus 10 mmHg). Additionally, the combination pill achieved higher blood pressure control rates (77% compared to 50%). The incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency of adverse effects was comparable between the two groups. Despite these promising results, the clinical experience with four-drug combination pills is still limited, and they are not yet recommended as an initial treatment option.[24]
Note: Calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blockers of the non-dihydropyridine Non-Dihydropyridine Pulmonary Hypertension Drugs variety must not be administered in combination with beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) as they may promote bradycardia Bradycardia Bradyarrhythmia is a rhythm in which the heart rate is less than 60/min. Bradyarrhythmia can be physiologic, without symptoms or hemodynamic change. Pathologic bradyarrhythmia results in reduced cardiac output and hemodynamic instability causing syncope, dizziness, or dyspnea. Bradyarrhythmias or an atrioventricular block Atrioventricular block Atrioventricular (AV) block is a bradyarrhythmia caused by delay, or interruption, in the electrical conduction between the atria and the ventricles. Atrioventricular block occurs due to either anatomic or functional impairment, and is classified into 3 types. Atrioventricular block (AV block) ( AV block AV block Atrioventricular (AV) block is a bradyarrhythmia caused by delay, or interruption, in the electrical conduction between the atria and the ventricles. Atrioventricular block occurs due to either anatomic or functional impairment, and is classified into 3 types. Atrioventricular block (AV block))!
Depending on the individual comorbidities Comorbidities The presence of co-existing or additional diseases with reference to an initial diagnosis or with reference to the index condition that is the subject of study. Comorbidity may affect the ability of affected individuals to function and also their survival; it may be used as a prognostic indicator for length of hospital stay, cost factors, and outcome or survival. St. Louis Encephalitis Virus, the respective medications may either gain or lose significance. A popular question in exams pertains to the following combinations: In case of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension combined with heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication are an option. ACE inhibitors ACE inhibitors Truncus Arteriosus may be used if there is heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), diabetic nephropathy Diabetic nephropathy Kidney injuries associated with diabetes mellitus and affecting kidney glomerulus; arterioles; kidney tubules; and the interstitium. Clinical signs include persistent proteinuria, from microalbuminuria progressing to albuminuria of greater than 300 mg/24 h, leading to reduced glomerular filtration rate and end-stage renal disease. Chronic Diabetic Complications. Beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) are also used for the treatment of heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR).
When choosing individual medications, side effects, individual tolerance Tolerance Pharmacokinetics and Pharmacodynamics, and interaction with other medications must be considered. If a two-drug combination is not effective, a third drug may be added.
Isolated systolic hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension should be treated the same way as systolic and diastolic hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension. However, since ISH occurs mostly in older patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, BP reduction should always be gradual (over 3–6 months) in these patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Ideally, maximal emphasis should be placed on nonpharmacologic therapy, particularly salt restriction and weight loss Weight loss Decrease in existing body weight. Bariatric Surgery in obese patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, because antihypertensive drugs commonly cause orthostatic (postural) and/or postprandial hypotension Postprandial hypotension Hypotension in older hypertensive patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.
High-yield fact:
Hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is considered the most common cause of ascending aortic aneurysm Ascending aortic aneurysm Thoracic Aortic Aneurysms. On the other hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy, atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis is considered the most common cause of descending aortic aneurysm Descending aortic aneurysm Thoracic Aortic Aneurysms.
Preventive approaches include the elimination Elimination The initial damage and destruction of tumor cells by innate and adaptive immunity. Completion of the phase means no cancer growth. Cancer Immunotherapy or reduction of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension risk factors.
Answers: 1-2, 2-3, 3-3
[1] Whelton, Paul K., Robert M. Carey, Wilbert S. Aronow, Donald E. Casey, Karen J. Collins, Cheryl Dennison Himmelfarb, Sondra M. DePalma, et al. “2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.” Hypertension (Dallas, Tex.: 1979) 71, no. 6 (June 2018): e13–115. https://doi.org/10.1161/HYP.0000000000000065.
[2] Zhou, Bin, Rodrigo M. Carrillo-Larco, Goodarz Danaei, Leanne M. Riley, Christopher J. Paciorek, Gretchen A. Stevens, Edward W. Gregg, et al. “Worldwide Trends in Hypertension Prevalence and Progress in Treatment and Control from 1990 to 2019: A Pooled Analysis of 1201 Population-Representative Studies with 104 Million Participants.” The Lancet 398, no. 10304 (September 11, 2021): 957–80. https://doi.org/10.1016/S0140-6736(21)01330-1.
[3] Arguedas JA, Leiva V, Wright JM. Blood pressure targets in adults with hypertension. Cochrane Database of Systematic Reviews 2020, Issue 12. Art. No.: CD004349. DOI: 10.1002/14651858.CD004349.pub3.]
[4] Muntner, Paul, Robert M. Carey, Samuel Gidding, Daniel W. Jones, Sandra J. Taler, Jackson T. Wright, and Paul K. Whelton. “Potential US Population Impact of the 2017 ACC/AHA High Blood Pressure Guideline.” Circulation 137, no. 2 (January 9, 2018): 109–18. https://doi.org/10.1161/CIRCULATIONAHA.117.032582.
[5] Roshandel, Gholamreza, Masoud Khoshnia, Hossein Poustchi, Karla Hemming, Farin Kamangar, Abdolsamad Gharavi, Mohammad Reza Ostovaneh, et al. “Effectiveness of Polypill for Primary and Secondary Prevention of Cardiovascular Diseases (PolyIran): A Pragmatic, Cluster-Randomised Trial.” The Lancet 394, no. 10199 (August 24, 2019): 672–83. https://doi.org/10.1016/S0140-6736(19)31791-X.}
[6] American College of Cardiology. “Polypills With and Without Aspirin for Primary Prevention of CVD.” https://www.acc.org/latest-in-cardiology/journal-scans/2021/09/06/22/25/http%3a%2f%2fwww.acc.org%2flatest-in-cardiology%2fjournal-scans%2f2021%2f09%2f06%2f22%2f25%2ffixed-dose-combination-therapies.
[7] Joseph, Philip, Gholamreza Roshandel, Peggy Gao, Prem Pais, Eva Lonn, Denis Xavier, Alvaro Avezum, et al. “Fixed-Dose Combination Therapies with and without Aspirin for Primary Prevention of Cardiovascular Disease: An Individual Participant Data Meta-Analysis.” The Lancet 398, no. 10306 (September 25, 2021): 1133–46. https://doi.org/10.1016/S0140-6736(21)01827-4.
[8] St. Sauver, Jennifer L., David O. Warner, Barbara P. Yawn, Debra J. Jacobson, Michaela E. Mc Gree, Joshua J. Pankratz, L. Joseph Melton, Véronique L. Roger, Jon O. Ebbert, and Walter A. Rocca. “Why Do Patients Visit Their Doctors? Assessing the Most Prevalent Conditions in a Defined US Population.” Mayo Clinic Proceedings. Mayo Clinic 88, no. 1 (January 2013): 56–67. https://doi.org/10.1016/j.mayocp.2012.08.020.
[9] Poulter, Neil R., Rafael Castillo, Fadi J. Charchar, Markus P. Schlaich, Aletta E. Schutte, Maciej Tomaszewski, Rhian M. Touyz, and Ji-Guang Wang. “Are the American Heart Association/American College of Cardiology High Blood Pressure Guidelines Fit for Global Purpose?: Thoughts From the International Society of Hypertension.” Hypertension (Dallas, Tex.: 1979) 72, no. 2 (August 2018): 260–62. https://doi.org/10.1161/HYPERTENSIONAHA.118.11452.
[10] Bell KJL, Doust J, Glasziou, P. Incremental Benefits and Harms of the 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. JAMA Intern Med. 2018. DOI: 10.1001/jamainternmed.2018.0310.
[11] Vaucher J, Marques-Videl P, Waeber G, Vollenweider P. Population impact of the 2017 ACC/AHA guidelines compared with the 2013 ESH/ESC guidelines for hypertension management. European Journal of Preventive Cardiology. 2018; 1:2047487318768938. DOI: 10.1177/2047487318768938.
[12] Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep 1;39(33):3021-3104. Doi: 10.1093/eurheartj/ehy339. Erratum in: Eur Heart J. 2019 Feb 1;40(5):475. PMID: 30165516.
[13] Mozaffarian, Dariush, Emelia J. Benjamin, Alan S. Go, Donna K. Arnett, Michael J. Blaha, Mary Cushman, Sarah de Ferranti, et al. “Heart Disease and Stroke Statistics–2015 Update: A Report from the American Heart Association.” Circulation 131, no. 4 (January 27, 2015): e29-322. https://doi.org/10.1161/CIR.0000000000000152.
[14] Bakris, George L., and Matthew Sorrentino, eds. Hypertension: A Companion to Braunwald’s Heart Disease E-Book. 3rd edition. Elsevier, 2017.
[15] Charles, Lesley, Jean Triscott, and Bonnie Dobbs. “Secondary Hypertension: Discovering the Underlying Cause.” American Family Physician 96, no. 7 (October 1, 2017): 453–61.]
[16] Oliveira-Paula, Gustavo H., Sherliane C. Pereira, Jose E. Tanus-Santos, and Riccardo Lacchini. “<p>Pharmacogenomics And Hypertension: Current Insights</P>.” Pharmacogenomics and Personalized Medicine (November 22, 2019): 341–59. https://doi.org/10.2147/PGPM.S230201.
[17] Centers for Disease Control and Prevention. (2024). High blood pressure risk factors. Centers for Disease Control and Prevention. https://www.cdc.gov/high-blood-pressure/risk-factors/index.html
[18] Hall, John, Hall, Michael. 2021. “Overview of the Circulation: Pressure, Flow, and Resistance.” In Guyton and Hall, Textbook of Medical Physiology,” 14th edition, 171-181. Philadelphia: Elsevier
[19] Cormick G, Ciapponi A, Cafferata ML, Cormick MS, Belizán JM. Calcium supplementation for prevention of primary hypertension. Cochrane Database of Systematic Reviews 2021, Issue 8. Art. No.: CD010037. DOI: 10.1002/14651858.CD010037.pub3.
[20] Ritter, James M.; Flower, Rod J.; Henderson, Graeme; Loke, Yoon Kong; MacEwan, David; Rang, Humphrey P. In “Drugs Acting on the Kidney” Rang & Dale’s Pharmacology E-Book, 388-394. Elsevier Health Sciences
[21] Williams, Bryan, Thomas M. MacDonald, Steve V. Morant, David J. Webb, Peter Sever, Gordon T. McInnes, Ian Ford, et al. “Endocrine and Haemodynamic Changes in Resistant Hypertension, and Blood Pressure Responses to Spironolactone or Amiloride: The PATHWAY-2 Mechanisms Substudies.” The Lancet Diabetes & Endocrinology 6, no. 6 (June 1, 2018): 464–75. https://doi.org/10.1016/S2213-8587(18)30071-8.
[22] Marshall, T. “How Many Antihypertensives Do Patients Need to Achieve a Target Blood Pressure?” Journal of Human Hypertension 19, no. 4 (April 2005): 317–19. https://doi.org/10.1038/sj.jhh.1001823.
[23] Misra, Shamita, and James J. Stevermer. “ACE Inhibitors and ARBs: One or the Other—Not Both—for High-Risk Patients.” The Journal of Family Practice, vol. 58, no. 1, Jan. 2009, pp. 24–27. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3183919/.
[24] Nolde, Janis M., et al. “Ambulatory Blood Pressure after 12 Weeks of Quadruple Combination of Quarter Doses of Blood Pressure Medication vs. Standard Medication.” Journal of Hypertension, vol. 42, no. 6, June 2024, pp. 1009–18. PubMed, https://doi.org/10.1097/HJH.0000000000003683.
[25] 2023 ESH Hypertension Guideline Update: Bringing Us Closer Together Across the Pond.” American College of Cardiology, https://www.acc.org/latest-in-cardiology/articles/2024/02/05/11/43/http%3a%2f%2fwww.acc.org%2flatest-in-cardiology%2farticles%2f2024%2f02%2f05%2f11%2f43%2f2023-esh-hypertension-guideline-update. Accessed 5 June 2024.