Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychologic exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). The medical history and physical exam of a patient presenting with dyspnea should be used to rule out certain conditions or suggest the most likely cause of the respiratory discomfort. Management focuses on treating the underlying condition.
Last updated: Dec 15, 2025
Dyspnea is the subjective sensation of breathing discomfort that derives from interactions among multiple physiologic, psychologic, social, and environmental factors.
There are 5 basic categories of causes that can lead to dyspnea. The causes can present individually or as a combination:
| Etiology | Clinical presentation | Associated conditions |
|---|---|---|
| Obstructive lung disease |
Characterized by air trapping in the
lungs
Lungs
Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2.
Lungs: Anatomy:
|
|
| Restrictive lung disease |
Characterized by decreased lung
compliance
Compliance
Distensibility measure of a chamber such as the lungs (lung compliance) or bladder. Compliance is expressed as a change in volume per unit change in pressure.
Veins: Histology:
|
Poor breathing mechanics:
ILDs:
|
| Upper airway obstruction Upper Airway Obstruction Airway Obstruction |
Findings:
|
|
| Others | Clinical presentation and findings vary with the cause. |
|
| Etiology | Clinical presentation | Associated conditions |
|---|---|---|
| Cardiac |
Often a complication of left-sided
heart failure
Heart Failure
A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction.
Total Anomalous Pulmonary Venous Return (TAPVR) Findings:
|
|
| Anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types |
Due to impaired tissue oxygenation Findings:
|
|
| Psychogenic |
Hyperventilation
Hyperventilation
A pulmonary ventilation rate faster than is metabolically necessary for the exchange of gases. It is the result of an increased frequency of breathing, an increased tidal volume, or a combination of both. It causes an excess intake of oxygen and the blowing off of carbon dioxide.
Respiratory Alkalosis may lead to
acute respiratory alkalosis
Acute respiratory alkalosis
Respiratory Alkalosis manifested as:
|
|
| Endocrine |
Changes in
pH
pH
The quantitative measurement of the acidity or basicity of a solution.
Acid-Base Balance and PaCO₂ stimulate the brainstem:
|
Metabolic
acidosis
Acidosis
A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up.
Respiratory Acidosis:
|
| Central dyspnea | Clinical presentation and findings vary with the cause. |
Neuromuscular disease
|
Common causes per affected organ system:
The 5 most common causes:
Pulmonary causes of chronic dyspnea can originate from disturbances in any of the following:
Extrapulmonary causes of chronic dyspnea:
| Elements of the physical exam | Important signs | Red-flag signs |
|---|---|---|
| Vital signs |
|
Red-flag vital signs:
|
| Pulmonary |
|
Red-flag exam findings:
|
| Cardiovascular |
|
|
| Abdominal |
|
|
| Musculoskeletal |
|
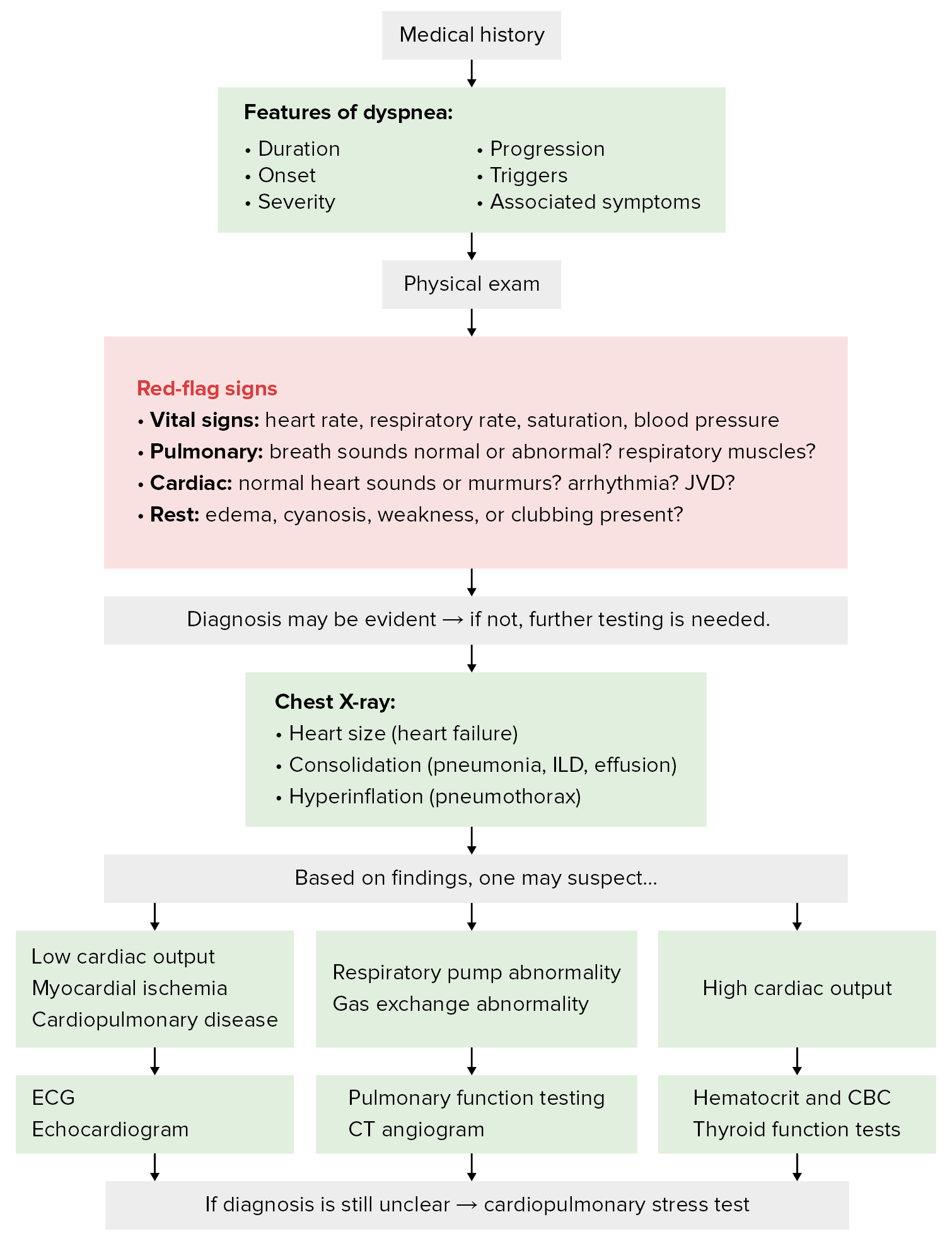
Diagnostic algorithm for dyspnea
Image by Lecturio.The following conditions are the most common causes of dyspnea by organ system: