Pulmonary embolism (PE) is a potentially fatal condition that occurs as a result of intraluminal obstruction of the main pulmonary artery or its branches. The causative factors include thrombi, air, amniotic fluid, and fat. In PE, gas exchange is impaired due to the decreased return of deoxygenated blood to the lungs. More than 90% of PEs are complications of a deep vein thrombosis (DVT) of the lower extremity. Some individuals are asymptomatic, but the most common presenting symptom is dyspnea. The symptoms can be acute or chronic, and diagnosis is usually based on radiographic findings, typically a CT pulmonary angiogram. Initial management is supportive and focuses on restoring oxygenation and hemodynamic stability. Both medical (systemic anticoagulants and/or thrombolytics) and interventional therapies (catheter-based thrombolysis, surgery) are used to reestablish vessel patency. Note: The following page will focus on thrombotic PE. See Nonthrombotic embolism for information on air, amniotic fluid, and fat emboli.
Last updated: May 26, 2023
Pulmonary embolism (PE) is the intraluminal obstruction of a main pulmonary artery Pulmonary artery The short wide vessel arising from the conus arteriosus of the right ventricle and conveying unaerated blood to the lungs. Lungs: Anatomy or any of its branches by a thrombus, air, amniotic fluid Amniotic fluid A clear, yellowish liquid that envelopes the fetus inside the sac of amnion. In the first trimester, it is likely a transudate of maternal or fetal plasma. In the second trimester, amniotic fluid derives primarily from fetal lung and kidney. Cells or substances in this fluid can be removed for prenatal diagnostic tests (amniocentesis). Placenta, Umbilical Cord, and Amniotic Cavity, or fat. When thrombotic PE is considered together with DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis, the condition is known as venous thromboembolic ( VTE VTE Obstruction of a vein or veins (embolism) by a blood clot (thrombus) in the bloodstream. Hypercoagulable States) disease.
The 3 primary factors that contribute to VTE VTE Obstruction of a vein or veins (embolism) by a blood clot (thrombus) in the bloodstream. Hypercoagulable States (known as Virchow’s triad Virchow’s triad Deep Vein Thrombosis) include venous stasis, hypercoagulability Hypercoagulability Hypercoagulable States, and vascular endothelial damage. Any condition that worsens 1 (or more) of the 3 factors increases the risk of DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis formation and, thus, PE.
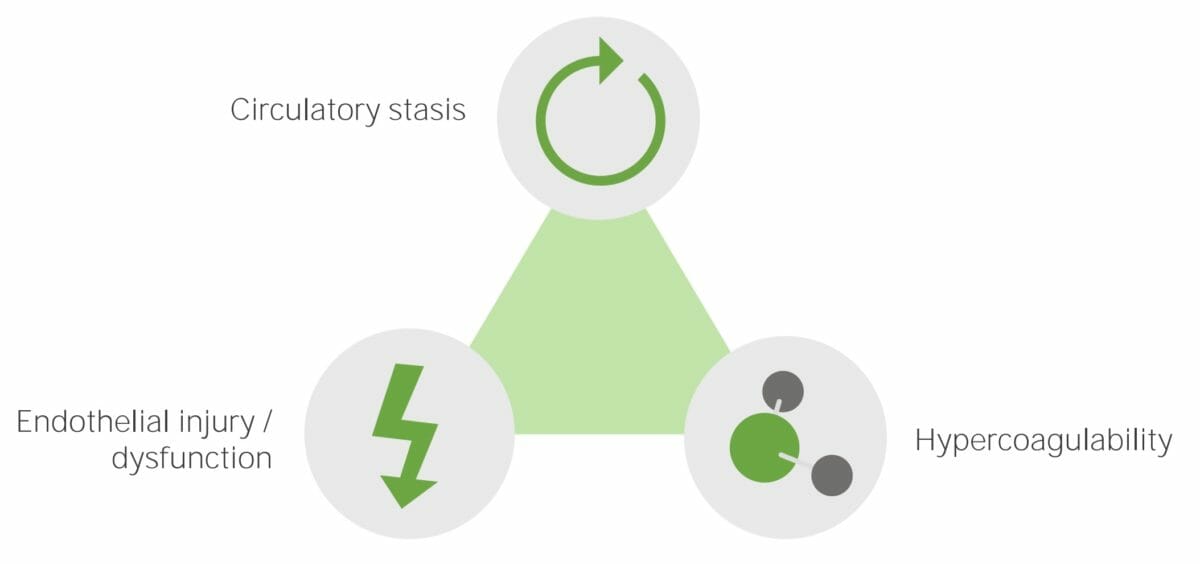
Virchow’s triad:
Circulatory stasis, endothelial injury or dysfunction, and hypercoagulability are the primary etiologic factors that cause venous thromboembolic disease.
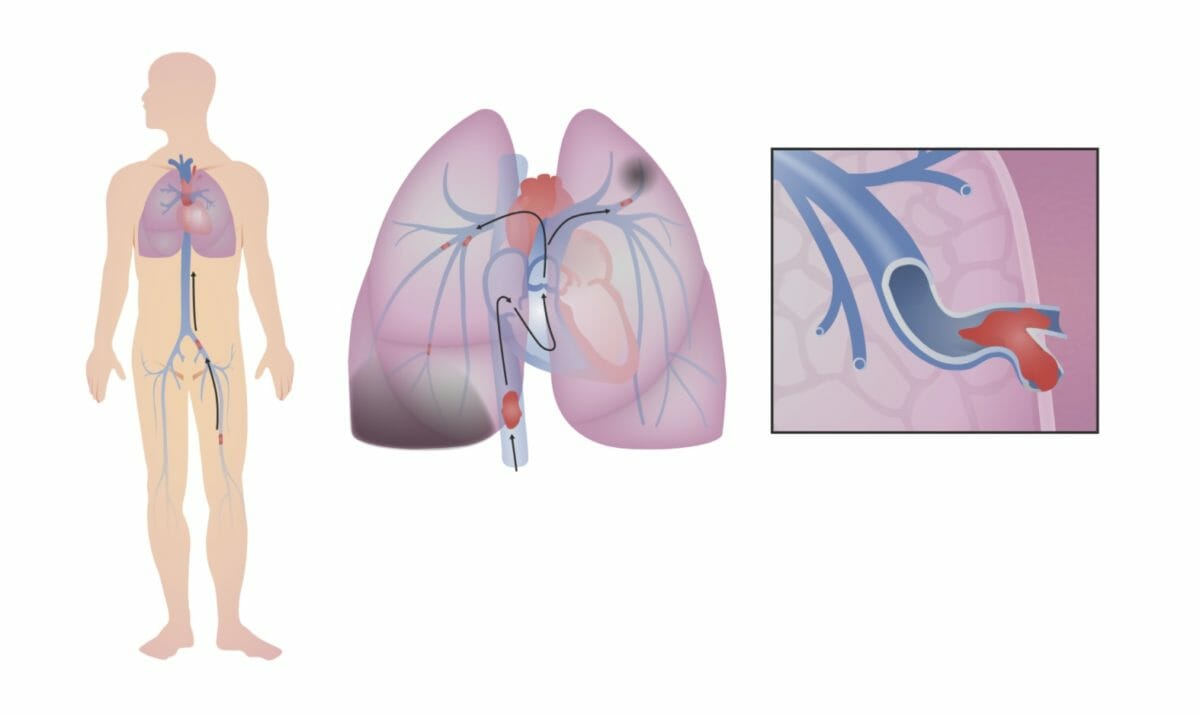
Venous thromboembolism:
A deep vein thrombosis (DVT) becomes dislodged in the leg (in this image, the thrombus forms in the left femoral vein). The DVT travels up the inferior vena cava (IVC) and through the right side of the heart. In this case, the DVT breaks into smaller fragments, which become lodged in smaller branches of the pulmonary arteries. The obstruction in blood flow through the lungs decreases the ability of the lungs to oxygenate the blood and, if large enough, puts strain on the right side of the heart.
Ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing/perfusion (V/Q) mismatch:
Hemodynamic instability:
Pulmonary infarction:
Presentation varies significantly. High suspicion must be maintained given the risks of complications and mortality Mortality All deaths reported in a given population. Measures of Health Status.
Diagnosis is primarily via imaging. The decision to obtain imaging is based on clinical suspicion, pretest probability Probability Probability is a mathematical tool used to study randomness and provide predictions about the likelihood of something happening. There are several basic rules of probability that can be used to help determine the probability of multiple events happening together, separately, or sequentially. Basics of Probability assessment (typically using the Modified Wells criteria), and D-dimer D-dimer Deep Vein Thrombosis levels.
| Major criteria | Score |
|---|---|
| Signs/symptoms of DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis | 3.0 |
| PE clinically more likely than other diagnoses | 3.0 |
| Tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children | 1.5 |
| Prolonged immobilization Immobilization Delirium (≥ 3 days) or recent surgery (within the last 30 days) | 1.5 |
| History of PE or DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis | 1.5 |
| Hemoptysis Hemoptysis Hemoptysis is defined as the expectoration of blood originating in the lower respiratory tract. Hemoptysis is a consequence of another disease process and can be classified as either life threatening or non-life threatening. Hemoptysis can result in significant morbidity and mortality due to both drowning (reduced gas exchange as the lungs fill with blood) and hemorrhagic shock. Hemoptysis | 1.0 |
| Malignancy Malignancy Hemothorax | 1.0 |
Chest radiography:
Chest CT pulmonary angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery ( CTPA CTPA Pulmonary Function Tests) with contrast or spiral Spiral Computed tomography where there is continuous x-ray exposure to the patient while being transported in a spiral or helical pattern through the beam of irradiation. This provides improved three-dimensional contrast and spatial resolution compared to conventional computed tomography, where data is obtained and computed from individual sequential exposures. Computed Tomography (CT) CT:
Ventilation-perfusion (V/Q) scan
Tests in hemodynamically unstable individuals: Bedside imaging can be used to make a presumptive diagnosis of PE, which justifies the initiation of treatment.
Pulmonary angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery:
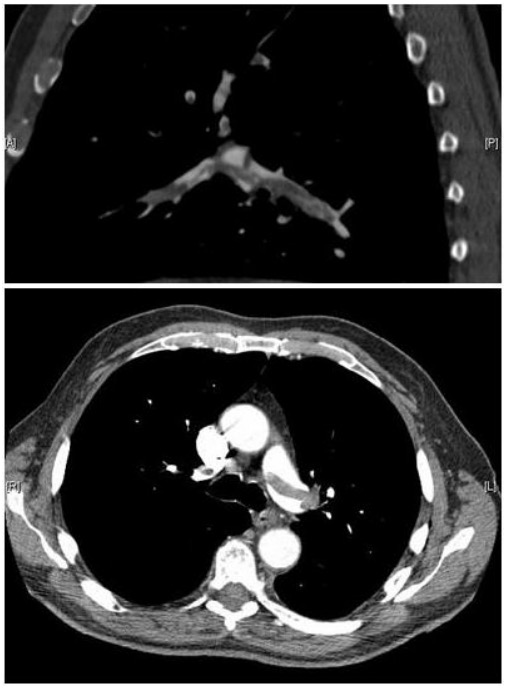
CT pulmonary angiography images confirming the presence of a saddle embolus and substantial thrombus burden in the lobar branches of both main pulmonary arteries
Image: “Pulmonary embolism CTPA” by Aung Myat and Arif Ahsan. License: CC BY 2.0
CT angiography demonstrating lobar and segmental pulmonary emboli (arrow) in the right lower lobe
Image: “CT angiography” by Thomas Jefferson University, 1025 Walnut Street, Philadelphia, PA 19107, USA. License: CC BY 3.0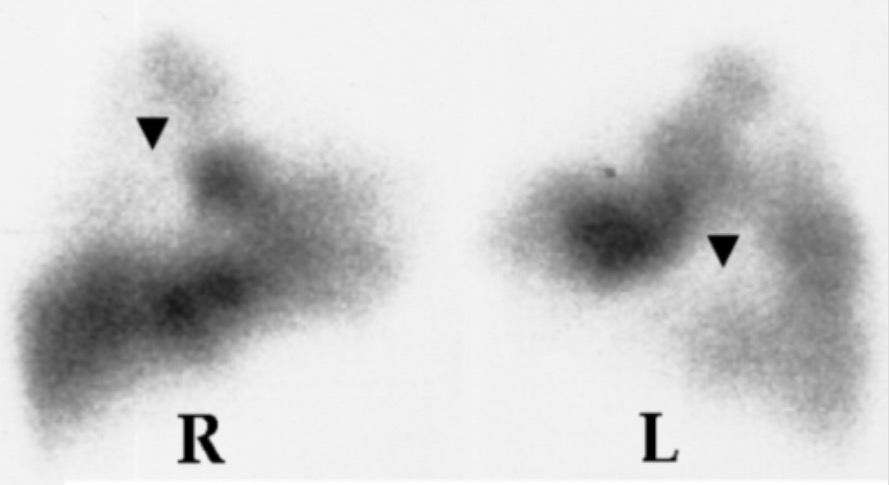
V/Q scan showing perfusion defects (arrows) in the right (R) and left (L) lungs
Image: “Lung scan” by Department of Cardiology, Sotiria Chest Diseases Hospital, Athens, Greece. License: CC BY 2.5Assess and treat any hemodynamic instability. A majority of individuals will either present in stable condition, or respond to initial resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome efforts.
Anticoagulation Anticoagulation Pulmonary Hypertension Drugs: secondary prevention of VTE VTE Obstruction of a vein or veins (embolism) by a blood clot (thrombus) in the bloodstream. Hypercoagulable States
IVC filter IVC filter Mechanical devices inserted in the inferior vena cava that prevent the migration of blood clots from deep venous thrombosis of the leg. Hypercoagulable States
Lifestyle/other options