Hypopituitarism is a condition characterized by pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types hormone deficiency. This condition primarily results from a disease of the pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland, but it may arise from hypothalamic dysfunction. Pituitary tumors Pituitary tumors Neoplasms which arise from or metastasize to the pituitary gland. The majority of pituitary neoplasms are adenomas, which are divided into non-secreting and secreting forms. Hormone producing forms are further classified by the type of hormone they secrete. Pituitary adenomas may also be characterized by their staining properties. Pituitary tumors may compress adjacent structures, including the hypothalamus, several cranial nerves, and the optic chiasm. Chiasmal compression may result in bitemporal hemianopsia. Pituitary Adenomas are one of the most common causes. The majority of cases affect the anterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types lobe ( adenohypophysis Adenohypophysis The anterior glandular lobe of the pituitary gland, also known as the adenohypophysis. It secretes the adenohypophyseal hormones that regulate vital functions such as growth; metabolism; and reproduction. Pituitary Gland: Anatomy), which accounts for 80% of the gland. The hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types produced from this lobe are growth hormone, follicle-stimulating hormone, luteinizing hormone, thyroid-stimulating hormone Thyroid-stimulating hormone A glycoprotein hormone secreted by the adenohypophysis. Thyrotropin stimulates thyroid gland by increasing the iodide transport, synthesis and release of thyroid hormones (thyroxine and triiodothyronine). Thyroid Hormones (TSH), adrenocorticotropic hormone Adrenocorticotropic hormone An anterior pituitary hormone that stimulates the adrenal cortex and its production of corticosteroids. Acth is a 39-amino acid polypeptide of which the n-terminal 24-amino acid segment is identical in all species and contains the adrenocorticotropic activity. Upon further tissue-specific processing, acth can yield alpha-msh and corticotropin-like intermediate lobe peptide (clip). Adrenal Hormones, and prolactin Prolactin A lactogenic hormone secreted by the adenohypophysis. It is a polypeptide of approximately 23 kd. Besides its major action on lactation, in some species prolactin exerts effects on reproduction, maternal behavior, fat metabolism, immunomodulation and osmoregulation. Breasts: Anatomy. When the posterior lobe Posterior lobe Cerebellum: Anatomy ( neurohypophysis Neurohypophysis Neural tissue of the pituitary gland, also known as the neurohypophysis. It consists of the distal axons of neurons that produce vasopressin and oxytocin in the supraoptic nucleus and the paraventricular nucleus. These axons travel down through the median eminence, the hypothalamic infundibulum of the pituitary stalk, to the posterior lobe of the pituitary gland. Pituitary Gland: Anatomy) is also damaged, loss of antidiuretic hormone Antidiuretic hormone Antidiuretic hormones released by the neurohypophysis of all vertebrates (structure varies with species) to regulate water balance and osmolarity. In general, vasopressin is a nonapeptide consisting of a six-amino-acid ring with a cysteine 1 to cysteine 6 disulfide bridge or an octapeptide containing a cystine. All mammals have arginine vasopressin except the pig with a lysine at position 8. Vasopressin, a vasoconstrictor, acts on the kidney collecting ducts to increase water reabsorption, increase blood volume and blood pressure. Hypernatremia and oxytocin occurs. All of these hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types regulate the activities of different organs, and thus the effects of pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types hypofunction are multisystemic. The diagnosis is made through a combination of clinical findings, hormone levels, provocation tests, and brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification imaging. Treatment is hormone replacement and addressing the etiology.
Last updated: Dec 15, 2025
Hypopituitarism is the condition resulting from inadequate production of pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types:
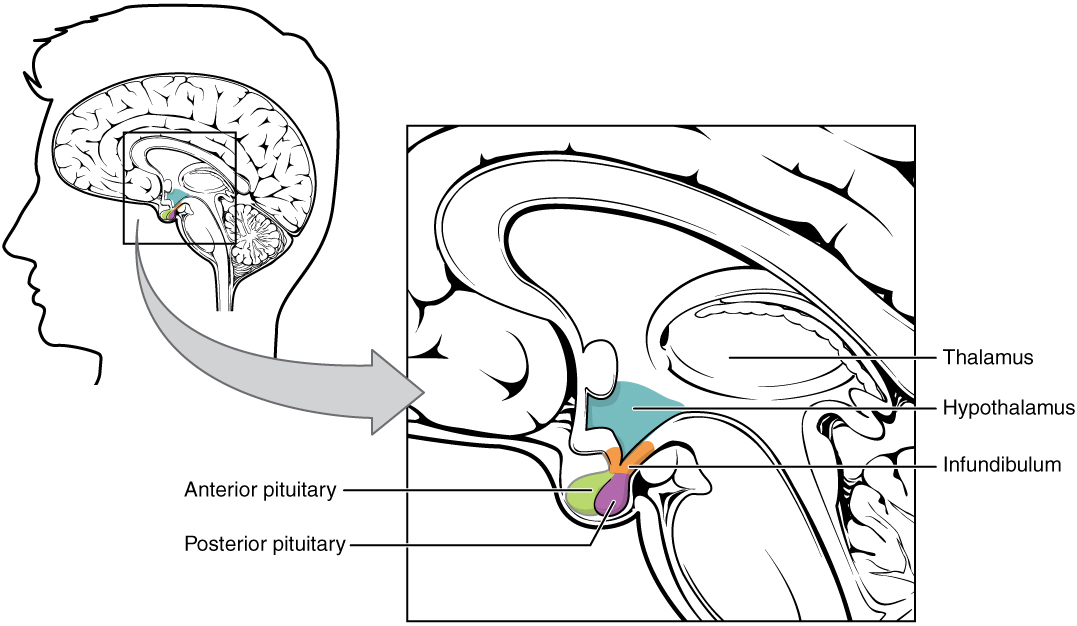
Hypothalamic–pituitary complex:
The image shows the pituitary gland, made up of the anterior and posterior lobes, in relation to the hypothalamus.
| Hormone | Pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types cell type | Target organ | Function | Decreased production |
|---|---|---|---|---|
| ACTH | Corticotroph | Adrenal cortex Adrenal Cortex The outer layer of the adrenal gland. It is derived from mesoderm and comprised of three zones (outer zona glomerulosa, middle zona fasciculata, and inner zona reticularis) with each producing various steroids preferentially, such as aldosterone; hydrocortisone; dehydroepiandrosterone; and androstenedione. Adrenal cortex function is regulated by pituitary adrenocorticotropin. Adrenal Glands: Anatomy | Stimulates:
|
Secondary adrenal insufficiency Secondary adrenal insufficiency Deficiency in pituitary adrenocorticotropic hormone (ACTH) secretion. Adrenal Insufficiency and Addison Disease |
| GH | Somatotroph | Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy and other tissues | Stimulates protein synthesis Synthesis Polymerase Chain Reaction (PCR) and overall growth of most cells and tissues |
|
| Prolactin Prolactin A lactogenic hormone secreted by the adenohypophysis. It is a polypeptide of approximately 23 kd. Besides its major action on lactation, in some species prolactin exerts effects on reproduction, maternal behavior, fat metabolism, immunomodulation and osmoregulation. Breasts: Anatomy | Lactotroph | Mammary glands |
|
Inability to produce milk (hypoprolactinemia) |
| TSH | Thyrotroph | Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland | Stimulates the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland to synthesize and secrete thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormone | Hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto’s disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism |
| LH LH A major gonadotropin secreted by the adenohypophysis. Luteinizing hormone regulates steroid production by the interstitial cells of the testis and the ovary. The preovulatory luteinizing hormone surge in females induces ovulation, and subsequent luteinization of the follicle. Luteinizing hormone consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle | Gonadotroph |
|
|
|
| FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle | Gonadotroph |
|
|
|
| Hormone | Pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types cell type | Target organ | Function | Decreased production |
|---|---|---|---|---|
| ADH | Supraoptic nuclei of hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus |
|
|
Diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus insipidus |
| Oxytocin | Paraventricular nuclei of hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus |
|
Stimulates:
|
Causes few symptoms, given limited effects |
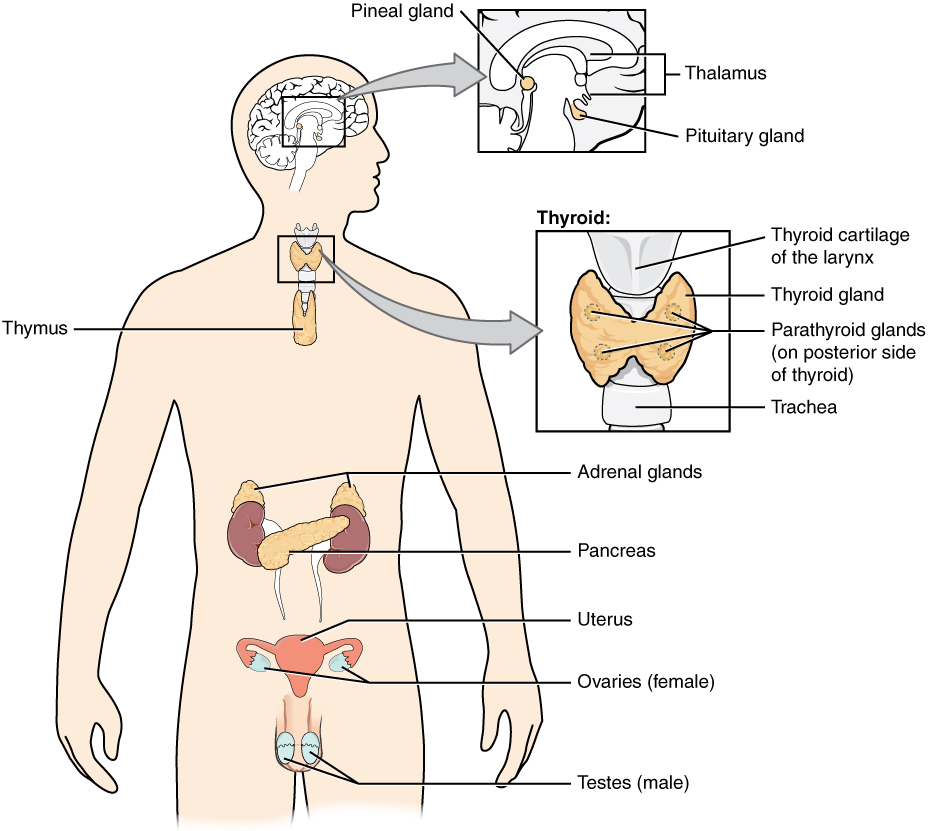
Pituitary gland and target organs:
The pituitary hormones help regulate the activity of endocrine glands throughout the body and play an important role in homeostasis.
Signs and symptoms are dependent on underlying pathology, speed of onset, and severity of hypopituitarism (partial or complete).
ACTH deficiency:
GH deficiency:
TSH deficiency:
LH LH A major gonadotropin secreted by the adenohypophysis. Luteinizing hormone regulates steroid production by the interstitial cells of the testis and the ovary. The preovulatory luteinizing hormone surge in females induces ovulation, and subsequent luteinization of the follicle. Luteinizing hormone consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle/ FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle deficiency:
ADH deficiency:
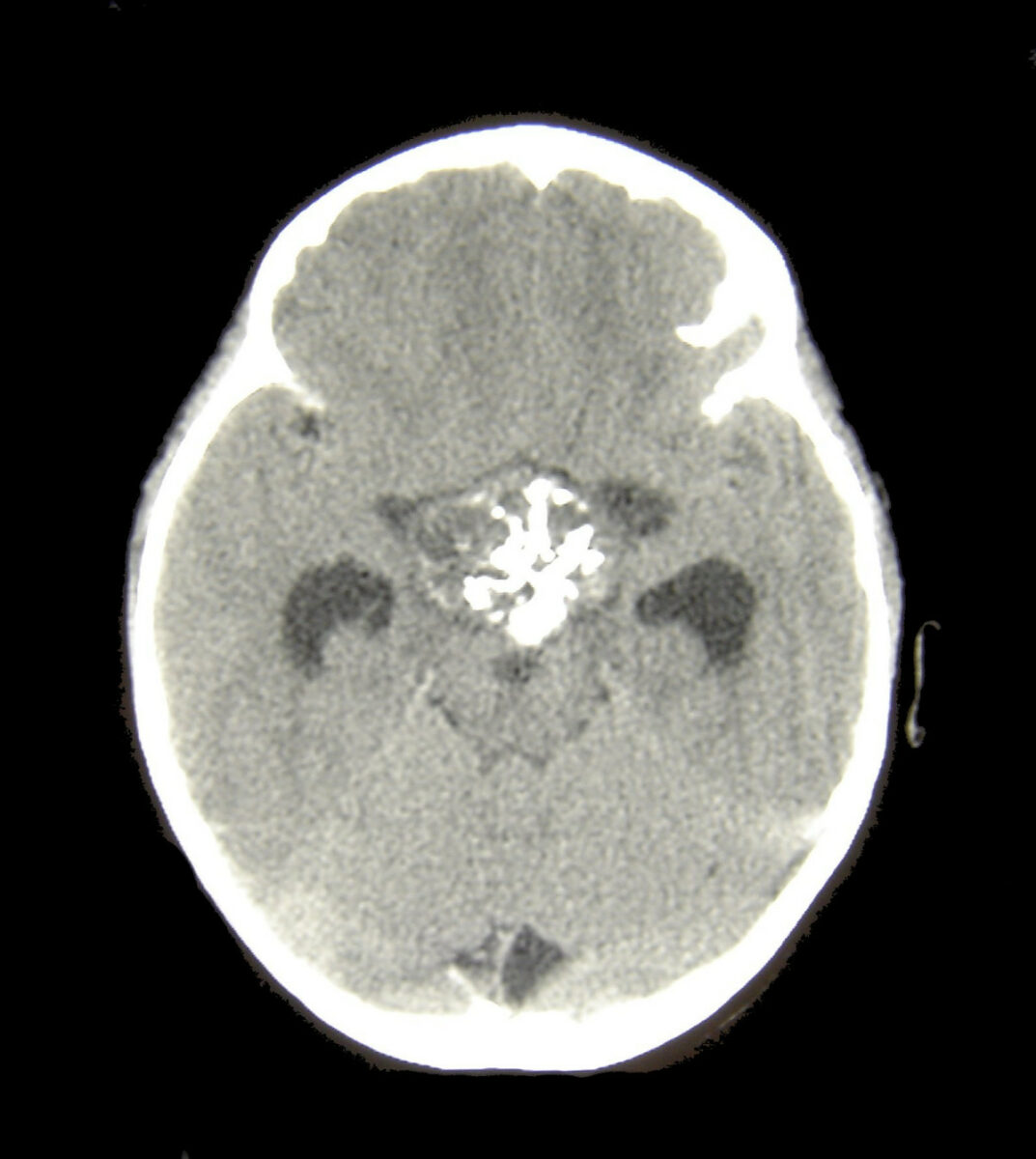
Head CT of a patient with a craniopharyngioma
Image: “Craniopharyngioma1” by Matthew R Garnett, Stéphanie Puget, Jacques Grill, Christian Sainte-Rose. License: CC BY 2.0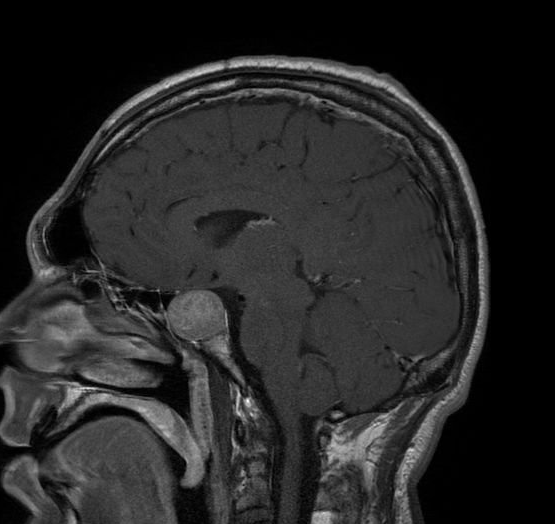
Magnetic resonance imaging scan of a patient with a large pituitary adenoma
Image: “Acromegaly” by Elgee. License: CC BY 3.0, edited by Lecturio.