Appendicitis is the acute inflammation Acute Inflammation Inflammation of the vermiform appendix Appendix A worm-like blind tube extension from the cecum. Colon, Cecum, and Appendix: Anatomy and the most common abdominal surgical emergency Surgical Emergency Acute Abdomen globally. The condition has a lifetime risk of 8%. Characteristic features include periumbilical abdominal pain Abdominal Pain Acute Abdomen that migrates to the right lower quadrant Right lower quadrant Anterior Abdominal Wall: Anatomy, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, anorexia Anorexia The lack or loss of appetite accompanied by an aversion to food and the inability to eat. It is the defining characteristic of the disorder anorexia nervosa. Anorexia Nervosa, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia. The diagnosis can frequently be established clinically, but imaging is used in uncertain cases. Computed tomography (CT) scan provides the highest diagnostic accuracy. Perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis occurs in 13%–20% of cases and can present as localized ( abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease/phlegmon) or free perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis with generalized peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury. The standard treatment is appendectomy Appendectomy Appendectomy is an invasive surgical procedure performed with the goal of resecting and extracting the vermiform appendix through either an open or a laparoscopic approach. The most common indication is acute appendicitis. Appendectomy, but localized perforations are frequently managed non-operatively with antibiotics.
Last updated: May 17, 2024
Appendicitis is the inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the vermiform appendix Appendix A worm-like blind tube extension from the cecum. Colon, Cecum, and Appendix: Anatomy.
Early:
Late:
Perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis:
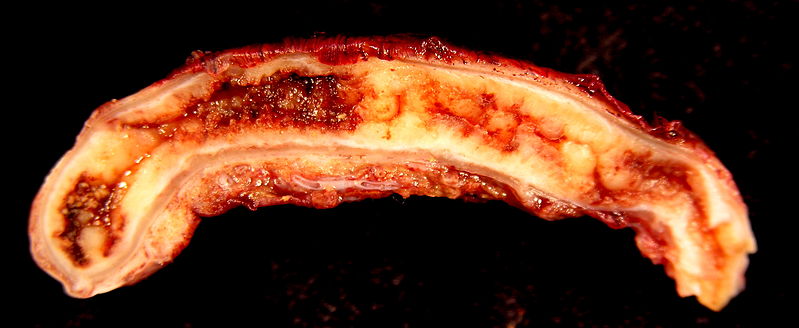
Acute appendicitis
Image: “Acute Appendicitis” by Ed Uthman. License: CC BY 2.0Classic:
Atypical:
Anatomic factors:
General:
Abdominal exam:
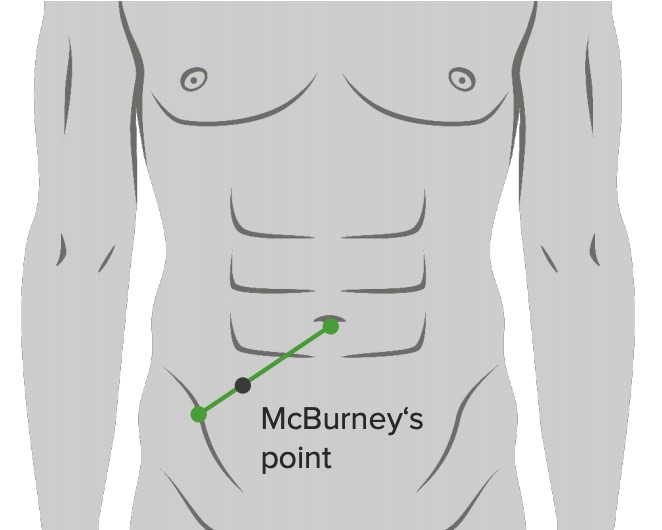
Location of the McBurney’s point: 2/3 from umbilicus on a straight line from the umbilicus to ASIS (anterior superior iliac spine)
Image by Lecturio.
Location of the McBurney’s point: 2/3 from umbilicus on a straight line from the umbilicus to ASIS (anterior superior iliac spine)
Image: “McBurney’s point” by Department of Basic Sciences, School of Medicine. Universidad de Caldas. Manizales, Colombia. License: CC BY 2.5Rectal exam:
Pelvic exam:
| Symptoms | Migratory pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in the right iliac fossa | 1 |
|---|---|---|
| Anorexia | 1 | |
| Nausea and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia | 1 | |
| Signs | Tenderness in the right iliac fossa | 2 |
| Rebound tenderness | 1 | |
| Elevated temperature | 1 | |
| Laboratory findings | Leukocytosis | 2 |
| Shift to left | 1 | |
| Total | 10 |
Imaging is not required for diagnosis if the Alvarado score is very low (< 3) or high (> 7).
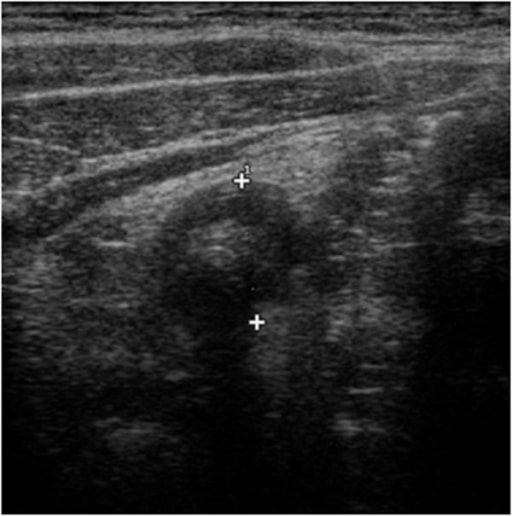
Ultrasound features of appendicitis: “target sign” characterized by a fluid-filled center and surrounded by an echogenic mucosa and submucosa and hypo-echoic muscularis
Image: “Ultrasound features of appendicitis” by Second University of Naples, Department of Clinical and Experimental Internistic F, Magrassi, Naples, Italy. License: CC BY 2.0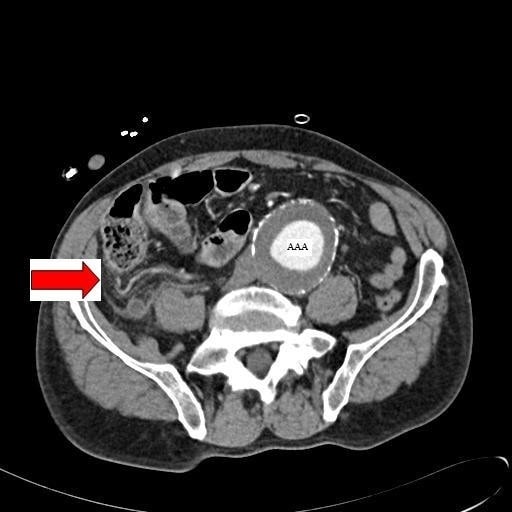
Abdominal CT image with contrast showing an inflamed appendix (marked by the red arrow) in a patient with a concomitant abdominal aortic aneurysm (AAA)
Image: “Abdominal CT” by Department of General Surgery, Queen Elizabeth Hospital, Queen Elizabeth Avenue, Sheriff Hill, Gateshead, Tyne & Wear, NE9 6SX, UK. License: CC BY 2.0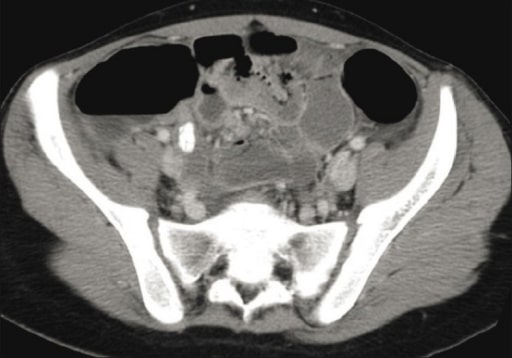
Pelvic CT image showing an inflamed appendix with an appendicolith
Image: “CT scan” by Department of Radiology, King Khalid University Hospital, King Saud University, Saudi Arabia. License: CC BY 2.0Definition: acute appendicitis without clinical or radiographic signs of perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis
Non-operative management (NOM):
Appendectomy Appendectomy Appendectomy is an invasive surgical procedure performed with the goal of resecting and extracting the vermiform appendix through either an open or a laparoscopic approach. The most common indication is acute appendicitis. Appendectomy:
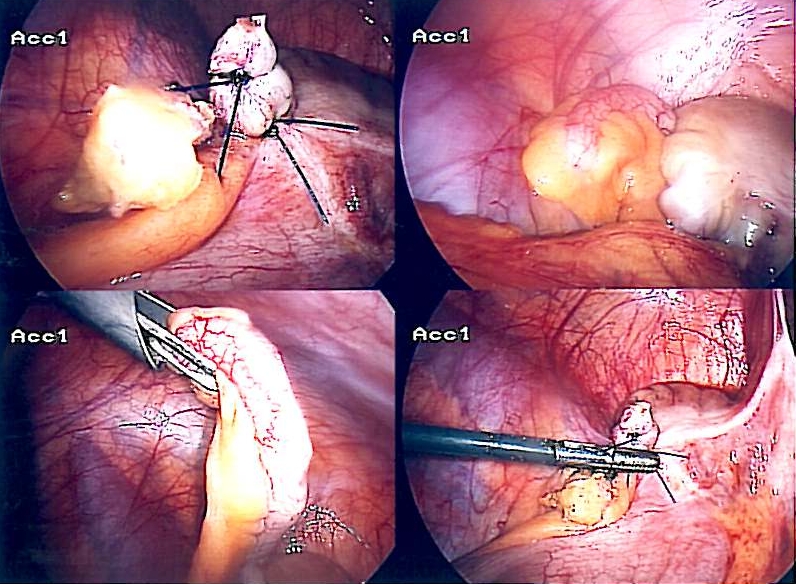
Laparoscopic appendectomy
Image: “Appendix-Entfernung” by Life-of-hannes.de. License: Public DomainDefinition: appendiceal rupture with or without phlegmon or abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease formation
Initial non-operative management:
Interval appendectomy Appendectomy Appendectomy is an invasive surgical procedure performed with the goal of resecting and extracting the vermiform appendix through either an open or a laparoscopic approach. The most common indication is acute appendicitis. Appendectomy:
Immediate appendectomy Appendectomy Appendectomy is an invasive surgical procedure performed with the goal of resecting and extracting the vermiform appendix through either an open or a laparoscopic approach. The most common indication is acute appendicitis. Appendectomy: