Hypertension is defined as a blood pressure (BP) of ≥130/80 mm Hg. Significantly elevated BP (≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic) carries a substantial risk of morbidity and mortality. Despite the prolonged presence of hypertension, there may be no signs or symptoms of end-organ damage (e.g., brain, eyes, heart, kidneys) until function becomes decompensated or severely impaired. Individuals may present with clinical symptoms such as chest pain due to MI or focal neurologic changes associated with a cerebral infarction or intracranial hemorrhage. Diagnosis is made using serial blood pressure measurements and testing for end-organ damage. Management includes lowering the blood pressure and treating specific organ damage.
Last updated: Dec 15, 2025
Regardless of the manifestation of severe hypertension Severe hypertension A confirmed blood pressure ≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic. Uncontrolled Hypertension, by definition, the individual will have a blood pressure ≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic.
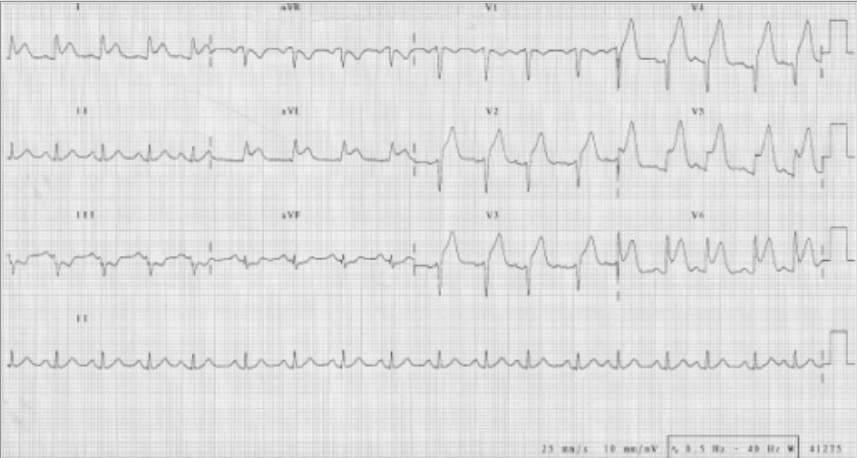
ECG indicating an anterior MI with ST-segment elevations seen in leads V2‒V6, I, and aVL:
Also note the reciprocal ST depressions in III and aVF.

Subarachnoid hemorrhage:
CT scan showing intracranial bleeding
During the initial assessment of an individual with severe hypertension Severe hypertension A confirmed blood pressure ≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic. Uncontrolled Hypertension, it is imperative to exclude chronic target-organ damage. Severe elevations in blood pressure should be quickly confirmed with repeat measurement.
Particular focus on risk factors for end-organ vascular events:
Symptoms of end-organ dysfunction:
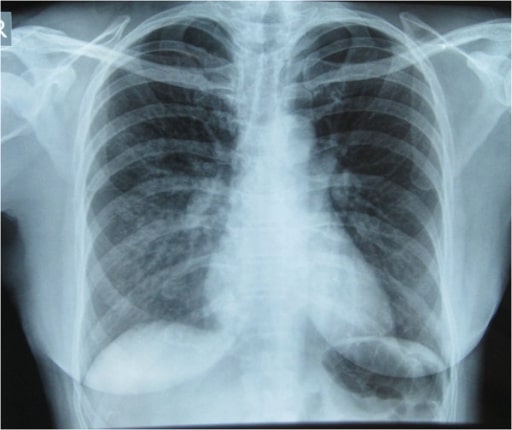
Chest X-ray showing pulmonary infiltrates in the right lung, especially in the right middle and lower lung zones, which are indicative of pulmonary edema
Image: “Initial Chest x-ray” by Nepal International Clinic, Travel and Mountain Medicine, Kathmandu, Nepal. License: CC BY 2.0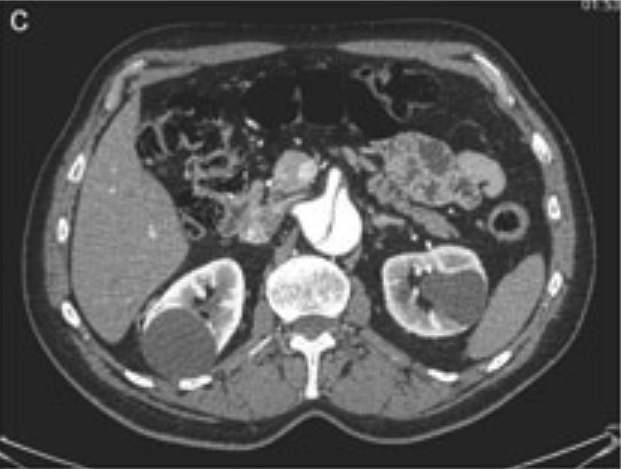
CT scan showing abdominal aortic dissection
Image: “Aortic dissection identified in the contrast-enhanced CT scan” by Department of Medical, Surgical and Neuro Sciences, Section of Radiological Sciences, Siena, Italy. License: CC BY 2.0, cropped by Lecturio.Management can be location-specific. The following are based on US and UK medical society recommendations.
Outpatient management:
ED management:
Admit individual to ICU ICU Hospital units providing continuous surveillance and care to acutely ill patients. West Nile Virus:
In general, rapid lowering of BP is not advised:
Exceptions:
Appropriate specialist consultation:
Therapeutic IV blood pressure agents:[5,9]
Specific hypertensive conditions and treatment:
| Conditions | Treatment goals | Preferred medications* | Notes |
|---|---|---|---|
| Intracerebral hemorrhage Intracerebral Hemorrhage Intracerebral hemorrhage (ICH) refers to a spontaneous or traumatic bleed into the brain parenchyma and is the 2nd-most common cause of cerebrovascular accidents (CVAs), commonly known as stroke, after ischemic CVAs. Intracerebral Hemorrhage (onset < 6 hours) | If increased intracranial pressure Intracranial Pressure Idiopathic Intracranial Hypertension, avoid fenoldopam and nitroprusside Nitroprusside A powerful vasodilator used in emergencies to lower blood pressure or to improve cardiac function. It is also an indicator for free sulfhydryl groups in proteins. Nitrates. | ||
| Acute ischemic stroke Ischemic Stroke An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke (< 72 hours after symptom onset) | If initiating IV thrombolysis therapy:
|
||
| Acute heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) | Avoid medications that reduce contractility (e.g., beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers)) | ||
| Acute coronary syndrome | |||
| Acute aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection | Reduce SBP SBP Ascites to < 120 mm Hg in the 1st hour | Start with beta-blockade before initiating vasodilators Vasodilators Drugs used to cause dilation of the blood vessels. Thromboangiitis Obliterans (Buerger Disease) | |
| Pre-eclampsia or eclampsia Eclampsia Onset of hyperreflexia; seizures; or coma in a previously diagnosed pre-eclamptic patient (pre-eclampsia). Hypertensive Pregnancy Disorders | Reduce SBP SBP Ascites to < 140 mm Hg in the 1st hour | Avoid most other antihypertensive drugs, when possible | |
| Pheochromocytoma Pheochromocytoma Pheochromocytoma is a catecholamine-secreting tumor derived from chromaffin cells. The majority of tumors originate in the adrenal medulla, but they may also arise from sympathetic ganglia (also referred to as paraganglioma). Symptoms are associated with excessive catecholamine production and commonly include hypertension, tachycardia, headache, and sweating. Pheochromocytoma | Reduce SBP SBP Ascites to < 140 mm Hg in the 1st hour | For hypertensive urgency Hypertensive urgency Asymptomatic, or relative asymptomatic, severe hypertension without end-organ damage. Uncontrolled Hypertension, start with alpha-adrenergic blockade, followed by beta-blocker |
After 8–24 hours of stable blood pressure control:
Diagnosis Codes:
These codes are used for
hypertensive crisis
Hypertensive Crisis
Oxazolidinones, a severe and acute elevation in blood pressure. They differentiate between
hypertensive urgency
Hypertensive urgency
Asymptomatic, or relative asymptomatic, severe hypertension without end-organ damage.
Uncontrolled Hypertension (no end-organ damage) and
hypertensive emergency
Hypertensive emergency
A condition of markedly elevated blood pressure with diastolic pressure usually greater than 120 mm hg. Malignant hypertension is characterized by widespread vascular damage, papilledema, retinopathy, hypertensive encephalopathy, and renal dysfunction.
Uncontrolled Hypertension (with acute end-organ damage).
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | I16.0 | Hypertensive urgency Hypertensive urgency Asymptomatic, or relative asymptomatic, severe hypertension without end-organ damage. Uncontrolled Hypertension |
| ICD-10-CM | I16.1 | Hypertensive emergency Hypertensive emergency A condition of markedly elevated blood pressure with diastolic pressure usually greater than 120 mm hg. Malignant hypertension is characterized by widespread vascular damage, papilledema, retinopathy, hypertensive encephalopathy, and renal dysfunction. Uncontrolled Hypertension |
| ICD-10-CM | I16.9 | Hypertensive crisis Hypertensive Crisis Oxazolidinones, unspecified |
Medications:
These codes are for intravenous antihypertensive medications used in a
hypertensive emergency
Hypertensive emergency
A condition of markedly elevated blood pressure with diastolic pressure usually greater than 120 mm hg. Malignant hypertension is characterized by widespread vascular damage, papilledema, retinopathy, hypertensive encephalopathy, and renal dysfunction.
Uncontrolled Hypertension to carefully lower blood pressure.
Labetalol
Labetalol
A salicylamide derivative that is a non-cardioselective blocker of beta-adrenergic receptors and alpha-1 adrenergic receptors.
Subarachnoid Hemorrhage and
nicardipine
Nicardipine
A potent calcium channel blockader with marked vasodilator action. It has antihypertensive properties and is effective in the treatment of angina and coronary spasms without showing cardiodepressant effects. It has also been used in the treatment of asthma and enhances the action of specific antineoplastic agents.
Class 4 Antiarrhythmic Drugs (Calcium Channel Blockers) are common choices.
| Coding System | Code | Description |
|---|---|---|
| RxNorm | 6135 | Labetalol Labetalol A salicylamide derivative that is a non-cardioselective blocker of beta-adrenergic receptors and alpha-1 adrenergic receptors. Subarachnoid Hemorrhage (ingredient) |
| RxNorm | 7394 | Nicardipine Nicardipine A potent calcium channel blockader with marked vasodilator action. It has antihypertensive properties and is effective in the treatment of angina and coronary spasms without showing cardiodepressant effects. It has also been used in the treatment of asthma and enhances the action of specific antineoplastic agents. Class 4 Antiarrhythmic Drugs (Calcium Channel Blockers) (ingredient) |
Complications:
These codes are for the acute end-organ damage that defines a
hypertensive emergency
Hypertensive emergency
A condition of markedly elevated blood pressure with diastolic pressure usually greater than 120 mm hg. Malignant hypertension is characterized by widespread vascular damage, papilledema, retinopathy, hypertensive encephalopathy, and renal dysfunction.
Uncontrolled Hypertension, such as
acute kidney injury
Acute Kidney Injury
Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine.
Acute Kidney Injury, acute
heart failure
Heart Failure
A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction.
Total Anomalous Pulmonary Venous Return (TAPVR), or an
intracerebral hemorrhage
Intracerebral Hemorrhage
Intracerebral hemorrhage (ICH) refers to a spontaneous or traumatic bleed into the brain parenchyma and is the 2nd-most common cause of cerebrovascular accidents (CVAs), commonly known as stroke, after ischemic CVAs.
Intracerebral Hemorrhage.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | N17.9 | Acute kidney failure, unspecified |
| ICD-10-CM | I50.21 | Acute systolic (congestive) heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) |
| ICD-10-CM | I61.9 | Nontraumatic intracerebral hemorrhage Intracerebral Hemorrhage Intracerebral hemorrhage (ICH) refers to a spontaneous or traumatic bleed into the brain parenchyma and is the 2nd-most common cause of cerebrovascular accidents (CVAs), commonly known as stroke, after ischemic CVAs. Intracerebral Hemorrhage, unspecified |