Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. To perform this function, the lungs need to be able to capture as much O2 as possible, a task that is easily achieved owing to their elastic Elastic Connective Tissue: Histology morphology. Each lung is enclosed within the visceral pleura Visceral pleura Pleura: Anatomy and completely fills 1 of the non-symmetrical pleural cavities, which are situated on the left and right sides of the mediastinum Mediastinum The mediastinum is the thoracic area between the 2 pleural cavities. The mediastinum contains vital structures of the circulatory, respiratory, digestive, and nervous systems including the heart and esophagus, and major thoracic vessels. Mediastinum and Great Vessels: Anatomy. The lungs encase the bronchial tree Bronchial tree The collective term "bronchial tree" refers to the bronchi and all of their subsequent branches. The bronchi are the airways of the lower respiratory tract. At the level of the 3rd or 4th thoracic vertebra, the trachea bifurcates into the left and right main bronchi. Both of these bronchi continue to divide into secondary or lobar bronchi that bifurcate further and further. Bronchial Tree: Anatomy and are divided functionally and anatomically into lobes.
Last updated: Jan 11, 2024
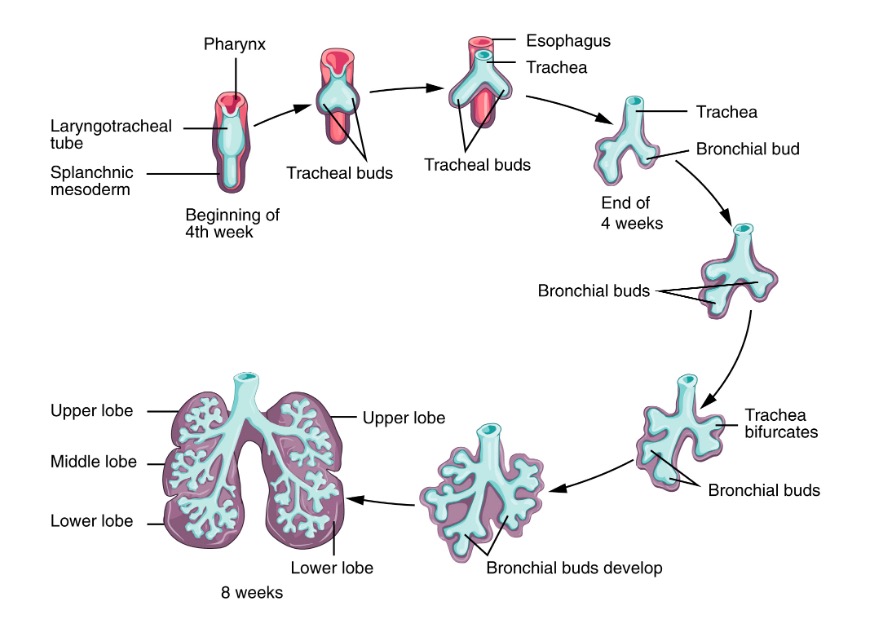
Development of the tracheobronchial tree and lungs occurs in 5 stages. The tracheobronchial tree originates from the foregut Foregut Development of the Abdominal Organs of the embryonic gut tube, beginning at week 4 of gestation and ending in childhood.
| Stage | Description | Clinical relevance |
|---|---|---|
| Embryonic period |
|
Defects:
|
| Pseudoglandular period |
|
|
| Canalicular period |
|
|
| Saccular period |
|
Infants born after 32 weeks or more have a higher survival rate. |
| Alveolar period |
|
|
Early stage of lung development:
During the early (embryonic and pseudoglandular) stages of lung development, the lung bud gradually transforms into the trachea and then bifurcates, forming the 2 mainstem bronchi. These bronchi further divide, giving rise to lobar and segmental bronchi.
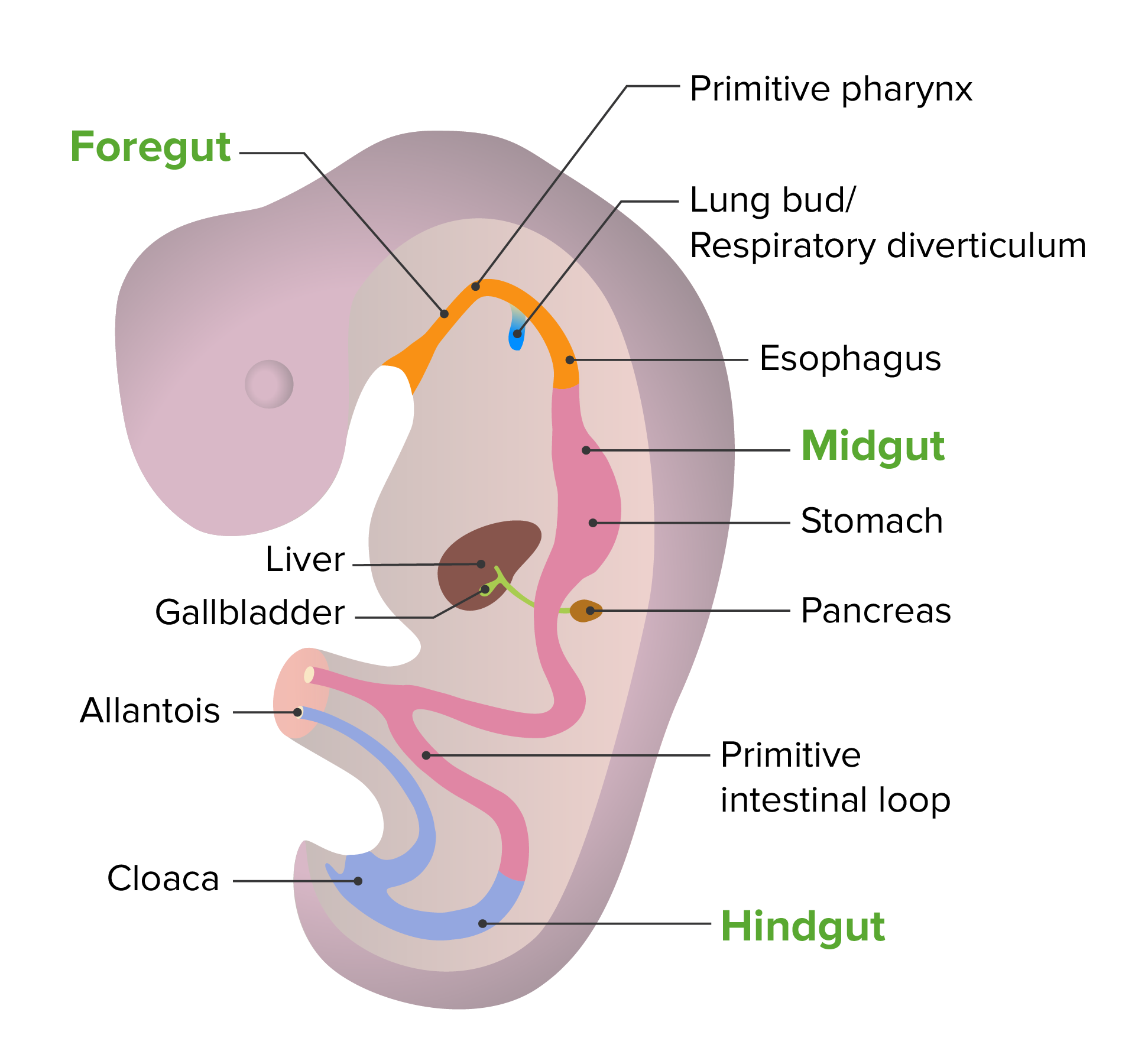
Embryonic development of the gut tube
Image by Lecturio. License: CC BY-NC-SA 4.0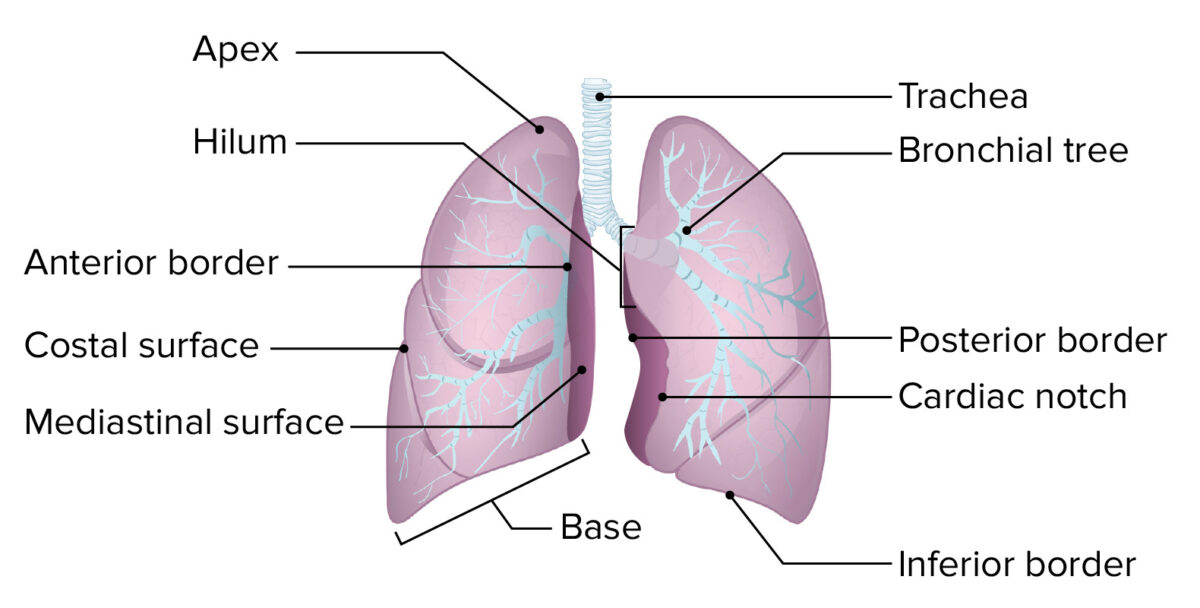
The basic structure of the lung:
The lung is composed of an apex, a base, 3 borders (inferior, anterior, and posterior), and 2 surfaces (mediastinal and costal).
The 2 lungs are not symmetrical Symmetrical Dermatologic Examination and vary both in weight and morphology. This difference is due to the size and location of the heart in the left hemithorax.
Right lung:
Left lung:
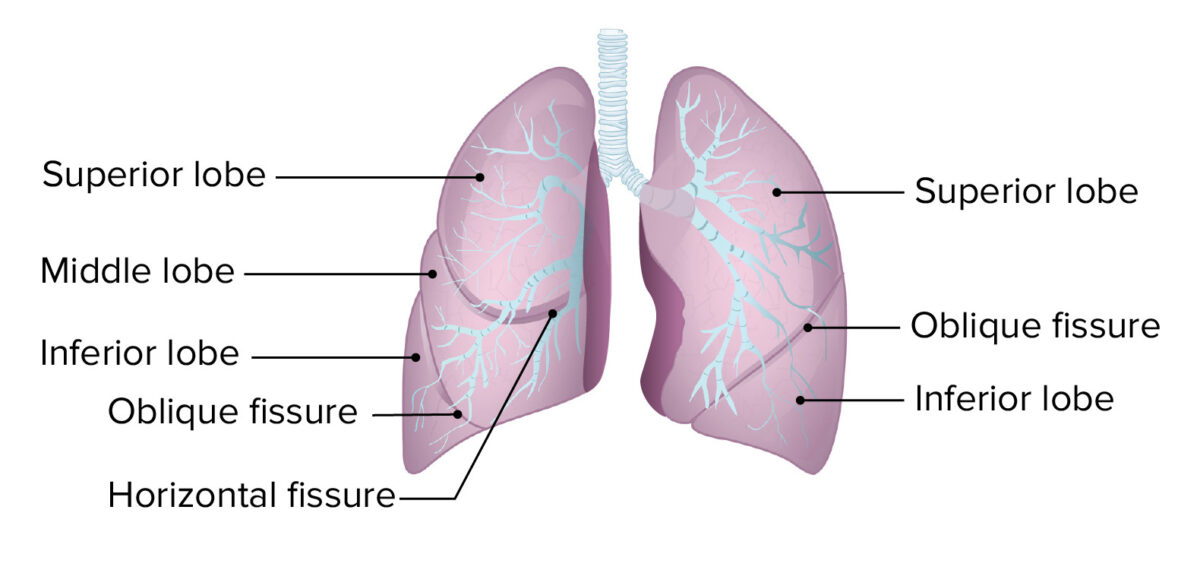
Lobes and fissures of the lungs
Image by Lecturio. License: CC BY-NC-SA 4.0Beyond the lobes and following the branching of the bronchial tree Bronchial tree The collective term “bronchial tree” refers to the bronchi and all of their subsequent branches. The bronchi are the airways of the lower respiratory tract. At the level of the 3rd or 4th thoracic vertebra, the trachea bifurcates into the left and right main bronchi. Both of these bronchi continue to divide into secondary or lobar bronchi that bifurcate further and further. Bronchial Tree: Anatomy, the lungs are divided into bronchopulmonary segments, which are the largest functional divisions of the pulmonary lobes.
| Left lung | Right lung |
|---|---|
Superior lobe:
|
Superior lobe:
|
Middle lobe:
|
|
Inferior lobe:
|
Inferior lobe:
|
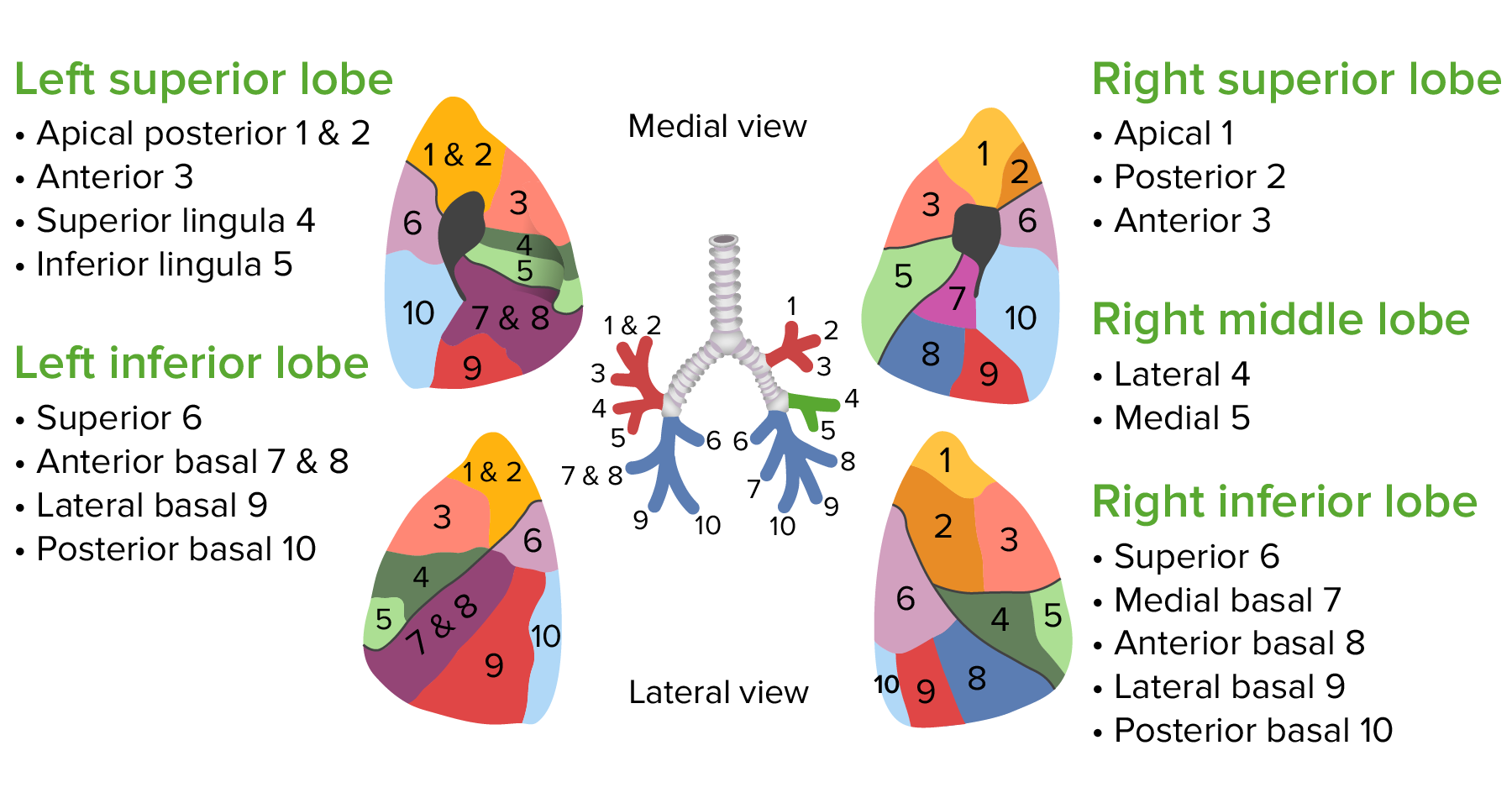
The bronchopulmonary segments of the lungs
Image by Lecturio. License: CC BY-NC-SA 4.0The microscopic anatomy of the bronchial tree Bronchial tree The collective term “bronchial tree” refers to the bronchi and all of their subsequent branches. The bronchi are the airways of the lower respiratory tract. At the level of the 3rd or 4th thoracic vertebra, the trachea bifurcates into the left and right main bronchi. Both of these bronchi continue to divide into secondary or lobar bronchi that bifurcate further and further. Bronchial Tree: Anatomy varies as the airways ramify. In general, the respiratory tract becomes smaller in diameter and has thinner walls with every ramification.
| Bronchi Bronchi The larger air passages of the lungs arising from the terminal bifurcation of the trachea. They include the largest two primary bronchi which branch out into secondary bronchi, and tertiary bronchi which extend into bronchioles and pulmonary alveoli. Bronchial Tree: Anatomy | Bronchioles Bronchioles The small airways branching off the tertiary bronchi. Terminal bronchioles lead into several orders of respiratory bronchioles which in turn lead into alveolar ducts and then into pulmonary alveoli. Bronchial Tree: Anatomy | Respiratory bronchioles Bronchioles The small airways branching off the tertiary bronchi. Terminal bronchioles lead into several orders of respiratory bronchioles which in turn lead into alveolar ducts and then into pulmonary alveoli. Bronchial Tree: Anatomy | Alveoli Alveoli Small polyhedral outpouchings along the walls of the alveolar sacs, alveolar ducts and terminal bronchioles through the walls of which gas exchange between alveolar air and pulmonary capillary blood takes place. Acute Respiratory Distress Syndrome (ARDS) | |
|---|---|---|---|---|
| Epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology | Pseudostratified ciliated columnar epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology | Ciliated columnar to cuboidal epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology | Non-ciliated simple cuboidal epithelium Simple cuboidal epithelium Surface Epithelium: Histology | Simple squamous epithelium Simple squamous epithelium Surface Epithelium: Histology |
| Special cells | Goblet cells Goblet cells A glandular epithelial cell or a unicellular gland. Goblet cells secrete mucus. They are scattered in the epithelial linings of many organs, especially the small intestine and the respiratory tract. Glandular Epithelium: Histology (mucus) | Club (a component of surfactant Surfactant Substances and drugs that lower the surface tension of the mucoid layer lining the pulmonary alveoli. Acute Respiratory Distress Syndrome (ARDS)) | Club (a component of surfactant Surfactant Substances and drugs that lower the surface tension of the mucoid layer lining the pulmonary alveoli. Acute Respiratory Distress Syndrome (ARDS)) | Type I and II pneumocytes |
| Smooth muscle | ✓ | ✓ | ✓ | X |
| Cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology | ✓ | X | X | X |
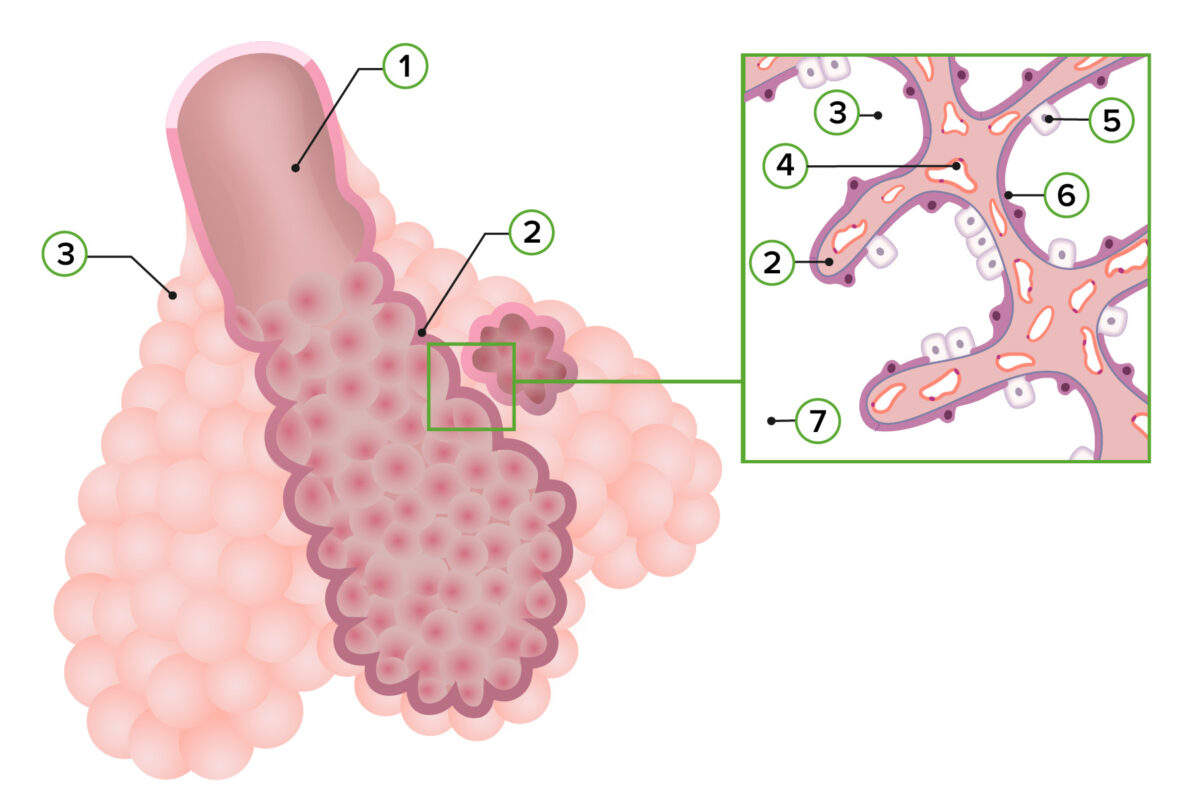
Representation of pulmonary histology in the alveolar stage:
1: Respiratory bronchiole
2: Primary septum
3: Alveolar sac
4: Capillaries
5: Type II pneumocyte
6: Type I pneumocyte
7: Alveolar duct
The lung receives mixed innervation from the pulmonary plexus containing the parasympathetic, sympathetic, and visceral afferent Afferent Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology fibers.
The main role of the lungs is to oxygenate the body and rid it of CO₂.
Ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing:
Respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal) or gas exchange Gas exchange Human cells are primarily reliant on aerobic metabolism. The respiratory system is involved in pulmonary ventilation and external respiration, while the circulatory system is responsible for transport and internal respiration. Pulmonary ventilation (breathing) represents movement of air into and out of the lungs. External respiration, or gas exchange, is represented by the O2 and CO2 exchange between the lungs and the blood. Gas Exchange:
Respiratory regulation Respiratory regulation Human cells are reliant on aerobic metabolism. Chemoreceptors in the lungs and tissues sense changes in the concentration of respiratory gasses and send messages to the CNS, which, in turn, modifies breathing parameters such as the respiratory rate or tidal volume to compensate for any imbalance. Disruption of this control mechanism can be caused by severe disease and also result in severe disease. Respiratory Regulation:
The following conditions of various origins can affect the lungs: