Atopic dermatitis, also known as eczema, is a chronic, relapsing, pruritic, inflammatory skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions disease that occurs more frequently in children, although adults can also be affected. The condition is often associated with elevated serum levels of IgE IgE An immunoglobulin associated with mast cells. Overexpression has been associated with allergic hypersensitivity. Immunoglobulins: Types and Functions and a personal or family history Family History Adult Health Maintenance of atopy. Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions dryness, erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion, oozing, crusting, and lichenification are present. Pruritus is a cardinal symptom. Diagnosis is established clinically. The mainstays of management are avoidance of triggers Triggers Hereditary Angioedema (C1 Esterase Inhibitor Deficiency), emollients Emollients Oleaginous substances used topically to soothe, soften or protect skin or mucous membranes. They are used also as vehicles for other dermatologic agents. Pityriasis Rosea, and topical corticosteroids Corticosteroids Chorioretinitis.
Last updated: Sep 5, 2022
Atopic dermatitis (also known as eczema) is a disorder of altered skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions barrier integrity and immune dysregulation that presents as a chronic relapsing inflammatory skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions disease.
Atopic dermatitis:
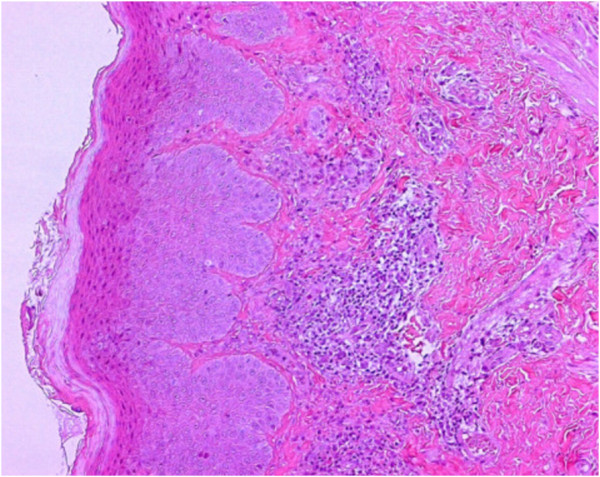
Histological image of the epidermal layer with a mild lymphohistiocytic and granulocytic infiltrate, predominantly eosinophilic

Erythema and lichenification in the kneefolds of a patient with atopic dermatitis
Image: “Role of the skin microbiome in atopic dermatitis” by Salava A, Lauerma A. License: CC BY 4.0
Atopic dermatitis
Image: “Atopic dermatitis” by Leonardi S, Filippelli M, Costanzo V, Rotolo N, La Rosa M. License: CC BY 2.0Patient education:
Elimination Elimination The initial damage and destruction of tumor cells by innate and adaptive immunity. Completion of the phase means no cancer growth. Cancer Immunotherapy of exacerbating factors:
Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions hydration (mainstay of treatment to reduce itching and episodes of inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation):
Topical treatments:
Oral antihistamines Antihistamines Antihistamines are drugs that target histamine receptors, particularly H1 and H2 receptors. H1 antagonists are competitive and reversible inhibitors of H1 receptors. First-generation antihistamines cross the blood-brain barrier and can cause sedation. Antihistamines:
Oral immunosuppressants Immunosuppressants Immunosuppressants are a class of drugs widely used in the management of autoimmune conditions and organ transplant rejection. The general effect is dampening of the immune response. Immunosuppressants:
Human monoclonal antibody:
Phototherapy Phototherapy Treatment of disease by exposure to light, especially by variously concentrated light rays or specific wavelengths. Hyperbilirubinemia of the Newborn: