Splenomegaly is pathologic enlargement of the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy that is attributable to numerous causes, including infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, hemoglobinopathies Hemoglobinopathies A group of inherited disorders characterized by structural alterations within the hemoglobin molecule. Anemia: Overview and Types, infiltrative processes, and outflow obstruction of the portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy. Aside from risks associated with the underlying pathology, enlargement of the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy puts affected individuals at increased risk of splenic rupture Splenic rupture Splenic rupture is a medical emergency that carries a significant risk of hypovolemic shock and death. Injury to the spleen accounts for nearly half of all injuries to intra-abdominal organs. The most common reason for a rupture of the spleen is blunt abdominal trauma, specifically, motor vehicle accidents. Rupture of the Spleen, a potentially fatal medical emergency that can result in hypovolemic shock Hypovolemic Shock Types of Shock.
Last updated: Dec 15, 2025
The spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy is not considered a vital organ, since the body can survive without it. However, the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy is the largest lymphoid organ and has an important role in immunity and blood filtration.
A spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy is considered enlarged when it can be palpated 2 cm below the costal margin or when imaging shows that its size is above the upper limits of normal for age.
Main functions:
Blood enters the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy via the splenic artery branching into central arterioles Arterioles The smallest divisions of the arteries located between the muscular arteries and the capillaries. Arteries: Histology:
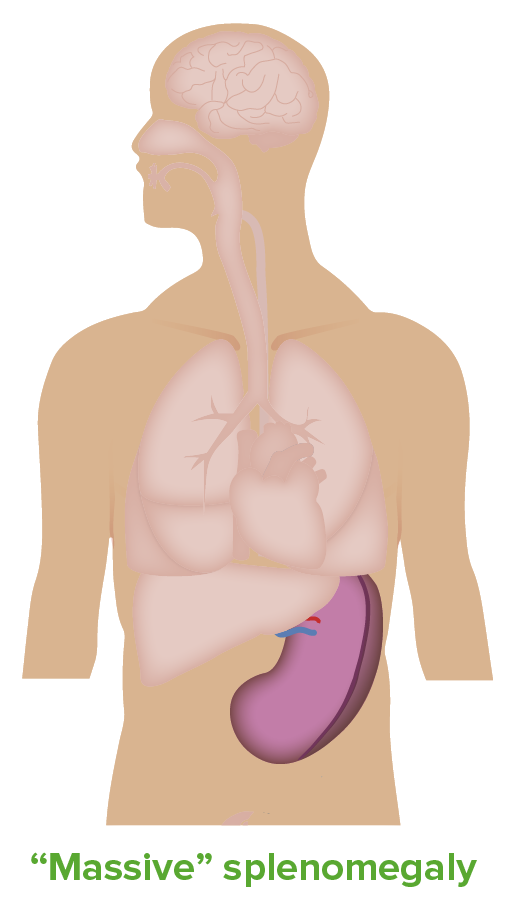
Splenomegaly:
An enlarged spleen can be identified through palpation or can seen with advanced imaging methods.
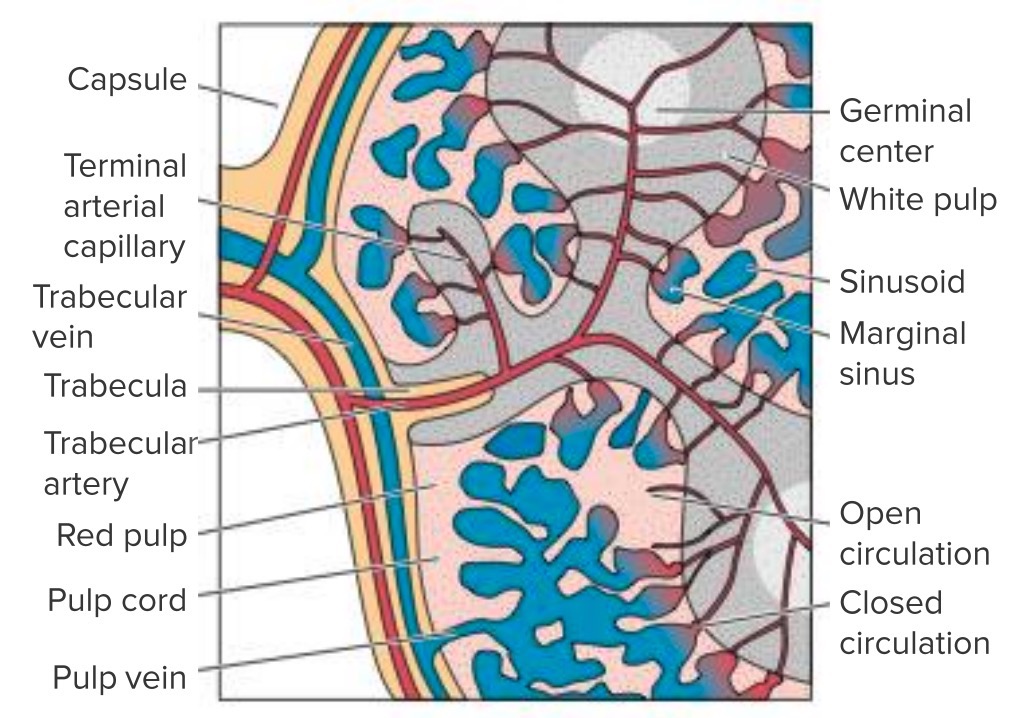
Internal structure of the spleen:
Note the flow of blood from the splenic artery to the white pulp and then to the red pulp and ultimately out of the spleen via the splenic vein. Dysfunction or obstruction in any of these regions can lead to splenomegaly.
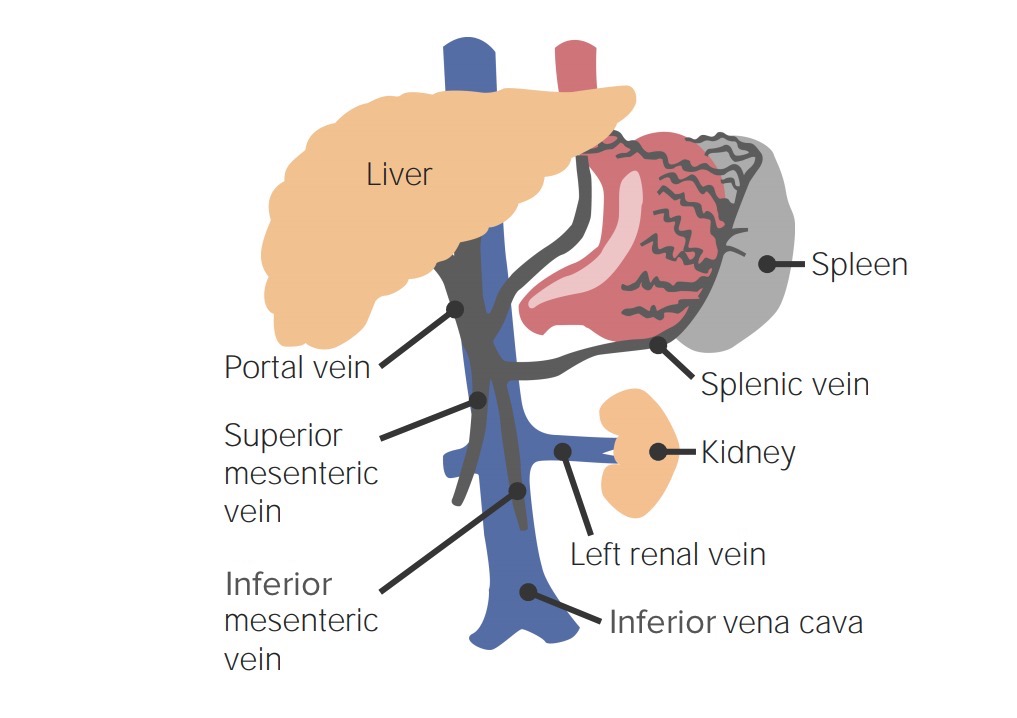
Hepatic portal drainage:
Note the splenic vein coming together with the superior mesenteric and inferior mesenteric veins. Outflow obstruction or congestion in this system can lead to a backup in the spleen and to splenomegaly.
The degree of splenomegaly is graded from 0 to 5, according to Hackett’s grading Grading Methods which attempt to express in replicable terms the level of cell differentiation in neoplasms as increasing anaplasia correlates with the aggressiveness of the neoplasm. Grading, Staging, and Metastasis system:
The differential diagnosis may be categorized on the basis of the degree of splenic enlargement.
| Category | Spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy size | Common causes |
|---|---|---|
| Massive | > 8 cm below LCM |
|
| Moderate | 5–8 cm below LCM |
|
| Mild | < 5 cm below LCM | Same as moderate |
Splenomegaly is a clinical sign associated with multiple causes rather than a diagnosis. When splenomegaly is present, patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship should be properly evaluated to identify the underlying cause.
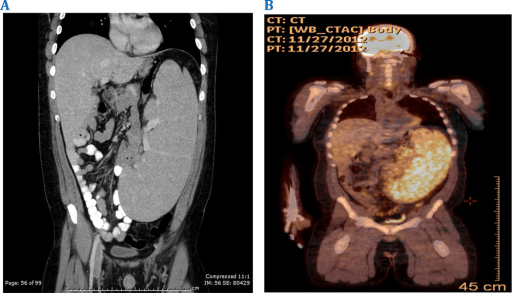
Symptomatic massive splenomegaly in persistent polyclonal B-cell lymphocytosis requiring splenectomy: CT and PET imaging reveal massive splenomegaly.
Image: “F2: CT and PET imaging reveal massive splenomegaly.” by Shanel B. Bhagwandin, Elliot S. Weisenberg, Howard Ozer, and Ajay V. Maker. License: CC BY 4.0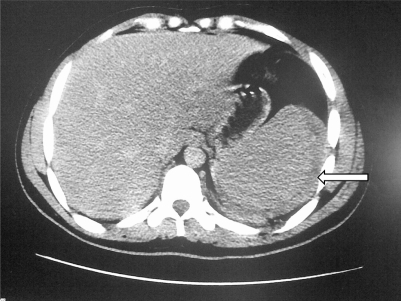
Abdominal CT of an individual with malaria:
Free fluid surrounds the enlarged spleen (arrow).
Management is based on the underlying cause and clinical status of the patient.