Diabetic ketoacidosis Ketoacidosis A life-threatening complication of diabetes mellitus, primarily of type 1 diabetes mellitus with severe insulin deficiency and extreme hyperglycemia. It is characterized by ketosis; dehydration; and depressed consciousness leading to coma. Metabolic Acidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are serious, acute complications of diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus. Diabetic ketoacidosis Ketoacidosis A life-threatening complication of diabetes mellitus, primarily of type 1 diabetes mellitus with severe insulin deficiency and extreme hyperglycemia. It is characterized by ketosis; dehydration; and depressed consciousness leading to coma. Metabolic Acidosis is characterized by hyperglycemia Hyperglycemia Abnormally high blood glucose level. Diabetes Mellitus and ketoacidosis Ketoacidosis A life-threatening complication of diabetes mellitus, primarily of type 1 diabetes mellitus with severe insulin deficiency and extreme hyperglycemia. It is characterized by ketosis; dehydration; and depressed consciousness leading to coma. Metabolic Acidosis due to an absolute insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin deficiency. Hyperosmolar hyperglycemic state occurs due to a relative deficiency of insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin or insulin resistance Insulin resistance Diminished effectiveness of insulin in lowering blood sugar levels: requiring the use of 200 units or more of insulin per day to prevent hyperglycemia or ketosis. Diabetes Mellitus, leading to severe hyperglycemia Hyperglycemia Abnormally high blood glucose level. Diabetes Mellitus and elevated serum osmolality Osmolality Plasma osmolality refers to the combined concentration of all solutes in the blood. Renal Sodium and Water Regulation. Triggering factors include inadequate insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin therapy, underlying infection, concurrent medical illness, or drug side effects. Diabetic ketoacidosis Ketoacidosis A life-threatening complication of diabetes mellitus, primarily of type 1 diabetes mellitus with severe insulin deficiency and extreme hyperglycemia. It is characterized by ketosis; dehydration; and depressed consciousness leading to coma. Metabolic Acidosis patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship tend to be younger, with type 1 Type 1 Spinal Muscular Atrophy diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, who present with acute symptoms, including abdominal pain Abdominal Pain Acute Abdomen, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia. On the other hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy, HHS patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are generally older, with type 2 diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, and will have gradual onset of symptoms, including altered mental status Altered Mental Status Sepsis in Children and neurologic changes. Both sets of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will have polyuria Polyuria Urination of a large volume of urine with an increase in urinary frequency, commonly seen in diabetes. Renal Potassium Regulation, polydipsia Polydipsia Excessive thirst manifested by excessive fluid intake. It is characteristic of many diseases such as diabetes mellitus; diabetes insipidus; and nephrogenic diabetes insipidus. The condition may be psychogenic in origin. Arginine Vasopressin Disorders (Diabetes Insipidus), and evidence of severe dehydration Severe Dehydration Fluid Replacement Therapy in Children. Diagnosis is based on laboratory values demonstrating hyperglycemia Hyperglycemia Abnormally high blood glucose level. Diabetes Mellitus with ketoacidosis Ketoacidosis A life-threatening complication of diabetes mellitus, primarily of type 1 diabetes mellitus with severe insulin deficiency and extreme hyperglycemia. It is characterized by ketosis; dehydration; and depressed consciousness leading to coma. Metabolic Acidosis or hyperosmolality. Management involves aggressive fluid rehydration Rehydration Dengue Virus, insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin therapy, and correction of electrolyte abnormalities.
Last updated: May 20, 2025
Diabetic ketoacidosis Ketoacidosis A life-threatening complication of diabetes mellitus, primarily of type 1 diabetes mellitus with severe insulin deficiency and extreme hyperglycemia. It is characterized by ketosis; dehydration; and depressed consciousness leading to coma. Metabolic Acidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are serious, acute complications of diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus.
The normal response to increased serum glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance involves the release of insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin by pancreatic beta cells. This leads to:
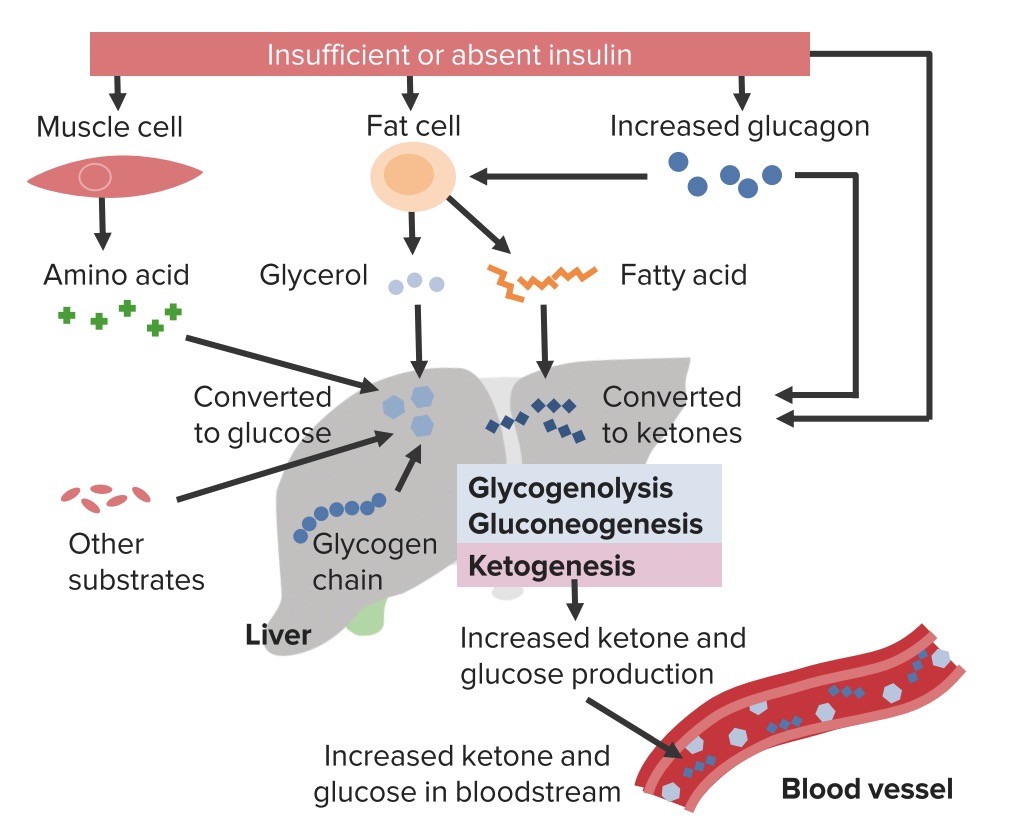
Pathophysiology of diabetic ketoacidosis
Image by Lecturio.| Laboratory test | Diabetic ketoacidosis Ketoacidosis A life-threatening complication of diabetes mellitus, primarily of type 1 diabetes mellitus with severe insulin deficiency and extreme hyperglycemia. It is characterized by ketosis; dehydration; and depressed consciousness leading to coma. Metabolic Acidosis | Hyperosmolar hyperglycemic state |
|---|---|---|
| Serum glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance | > 250 mg/dL | > 600 mg/dL |
| Serum bicarbonate Bicarbonate Inorganic salts that contain the -HCO3 radical. They are an important factor in determining the ph of the blood and the concentration of bicarbonate ions is regulated by the kidney. Levels in the blood are an index of the alkali reserve or buffering capacity. Electrolytes | ↓↓ | > 18 mEq/L |
| Anion gap Anion gap Metabolic Acidosis | ↑ | Generally normal |
| Serum osmolality Osmolality Plasma osmolality refers to the combined concentration of all solutes in the blood. Renal Sodium and Water Regulation | Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables | > 320 mOsm/kg |
| Serum ketones Ketones Organic compounds containing a carbonyl group =C=O bonded to two hydrocarbon groups. Basics of Carbohydrates ( beta-hydroxybutyrate Beta-hydroxybutyrate Butyric acid substituted in the beta or 3 position. It is one of the ketone bodies produced in the liver. Ketone Body Metabolism, acetone Acetone A colorless liquid used as a solvent and an antiseptic. It is one of the ketone bodies produced during ketoacidosis. Ketone Body Metabolism) | Positive | Small or negative |
| Urine ketones Ketones Organic compounds containing a carbonyl group =C=O bonded to two hydrocarbon groups. Basics of Carbohydrates | Positive | Small or negative |
| Arterial blood gas Arterial blood gas Respiratory Alkalosis |
|
pH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance: > 7.3 |
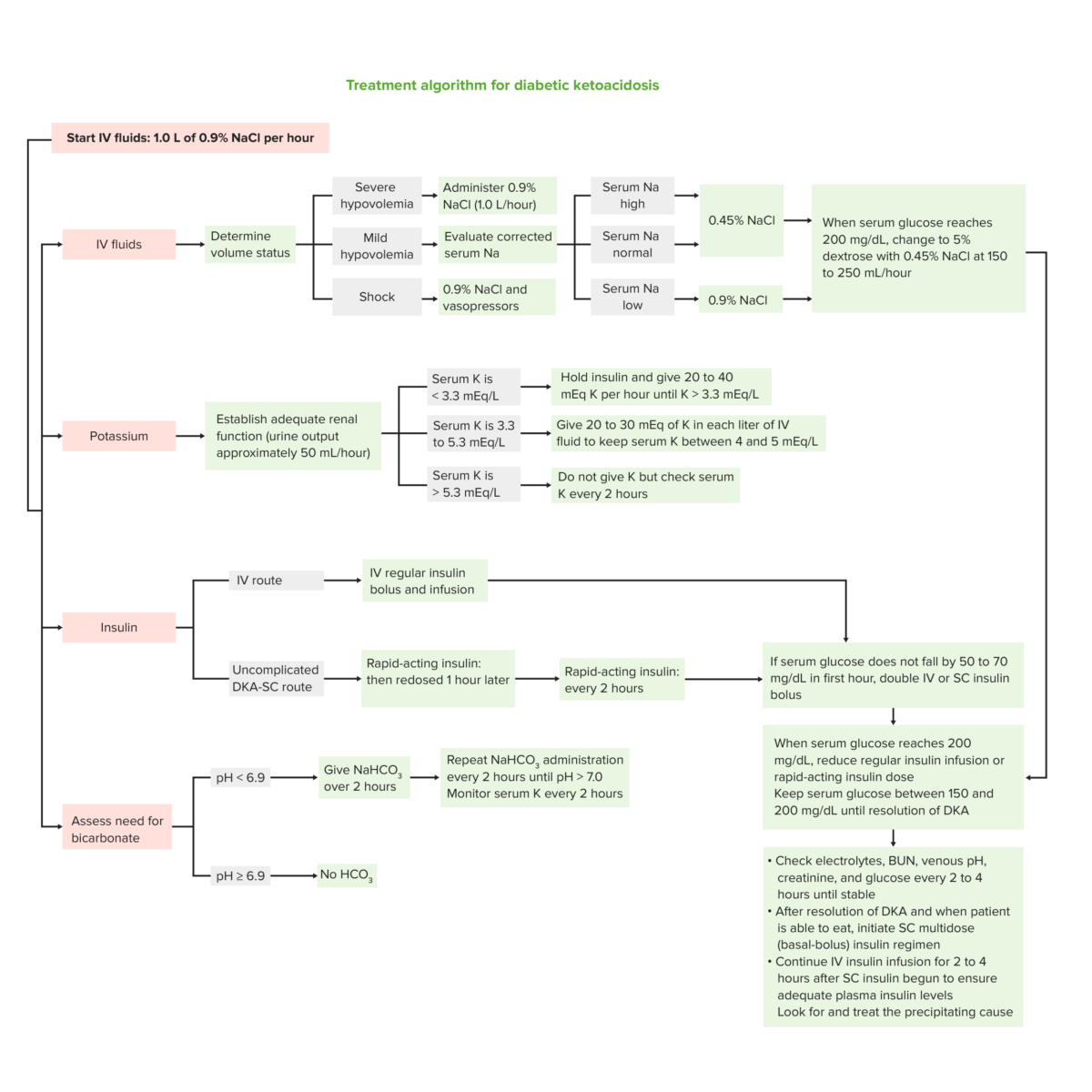
Treatment algorithm for diabetic ketoacidosis
Image by Lecturio.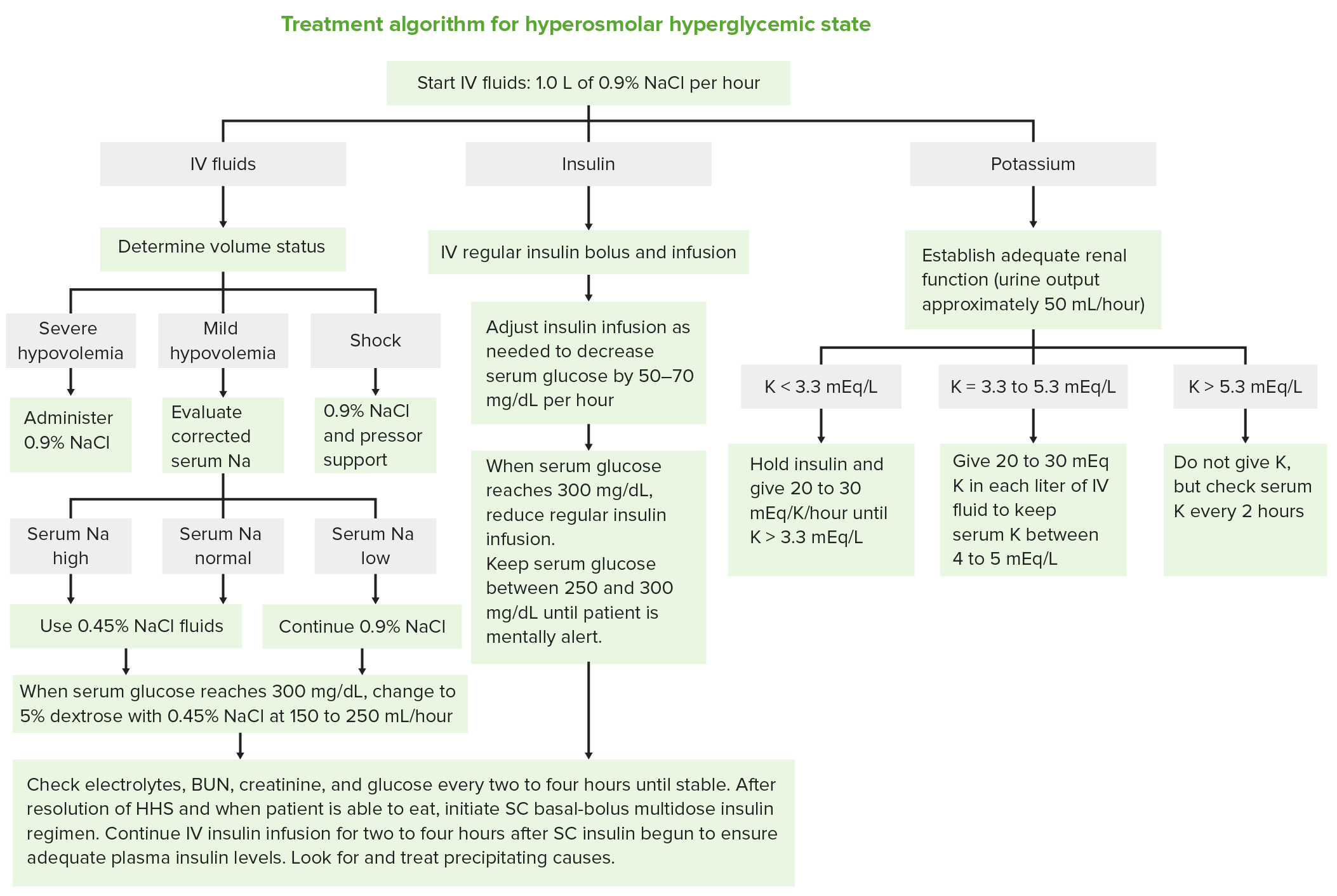
Treatment algorithm hyperosmolar hyperglycemic state
Image by Lecturio.