Acute abdomen, which is in many cases a surgical emergency, is the sudden onset of abdominal pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways that may be caused by inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, infection, perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis, ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, or obstruction. The location of the pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, its characteristics, and associated symptoms (e.g., jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice) are important tools that help narrow the differential diagnosis. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will typically have severe tenderness with associated rigidity Rigidity Continuous involuntary sustained muscle contraction which is often a manifestation of basal ganglia diseases. When an affected muscle is passively stretched, the degree of resistance remains constant regardless of the rate at which the muscle is stretched. This feature helps to distinguish rigidity from muscle spasticity. Megacolon and rebound tenderness. Laboratory evaluation will demonstrate leukocytosis Leukocytosis A transient increase in the number of leukocytes in a body fluid. West Nile Virus, acidosis Acidosis A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up. Respiratory Acidosis, and in some cases, abnormal hepatic function tests. Imaging helps narrow the differential diagnosis; first-line imaging is always an upright chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests to evaluate for pneumoperitoneum Pneumoperitoneum A condition with trapped gas or air in the peritoneal cavity, usually secondary to perforation of the internal organs such as the lung and the gastrointestinal tract, or to recent surgery. Pneumoperitoneum may be purposely introduced to aid radiological examination. Perforated Viscus. The treatment and prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas of acute abdomen strongly depend on the underlying cause, but the vast majority of these cases constitute a surgical emergency with associated morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and mortality Mortality All deaths reported in a given population. Measures of Health Status.
Last updated: May 17, 2024
Acute abdomen is the constellation of signs and symptoms associated with severe abdominal pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury that frequently requires emergency surgical intervention.
Nonsurgical causes of acute abdomen:
Surgical causes of acute abdomen:
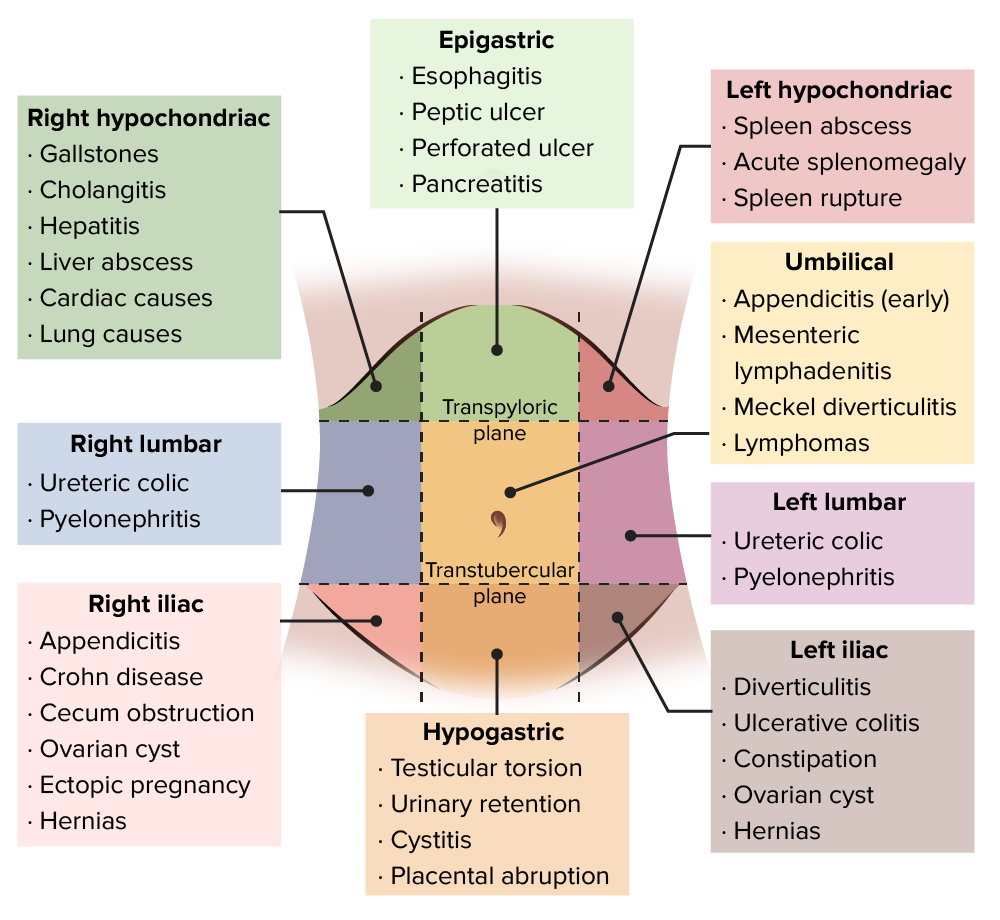
Differential diagnosis of acute abdominal pain
Image by Lecturio.For descriptive purposes, the abdomen can be divided into 4 quadrants or 9 regions.
Quadrants:
Divided into 4 quadrants by 2 perpendicular lines crossing at the umbilicus:
Right upper quadrant
Right upper quadrant
Anterior Abdominal Wall: Anatomy (RUQ):
|
Left upper quadrant
Left upper quadrant
Anterior Abdominal Wall: Anatomy (LUQ):
|
Right lower quadrant
Right lower quadrant
Anterior Abdominal Wall: Anatomy (RLQ):
|
Left lower quadrant
Left Lower quadrant
Anterior Abdominal Wall: Anatomy (LLQ):
|
Regions:
The abdomen can be divided into regions with 4 lines:
| Right hypochondriac region | Epigastric region Epigastric region Anterior Abdominal Wall: Anatomy | Left hypochondriac region |
| Right lumbar region Lumbar region Spinal Cord: Anatomy | Umbilical region Umbilical Region Surgical Anatomy of the Abdomen | Left lumbar region Lumbar region Spinal Cord: Anatomy |
| Right iliac region | Hypogastric region | Left iliac region |
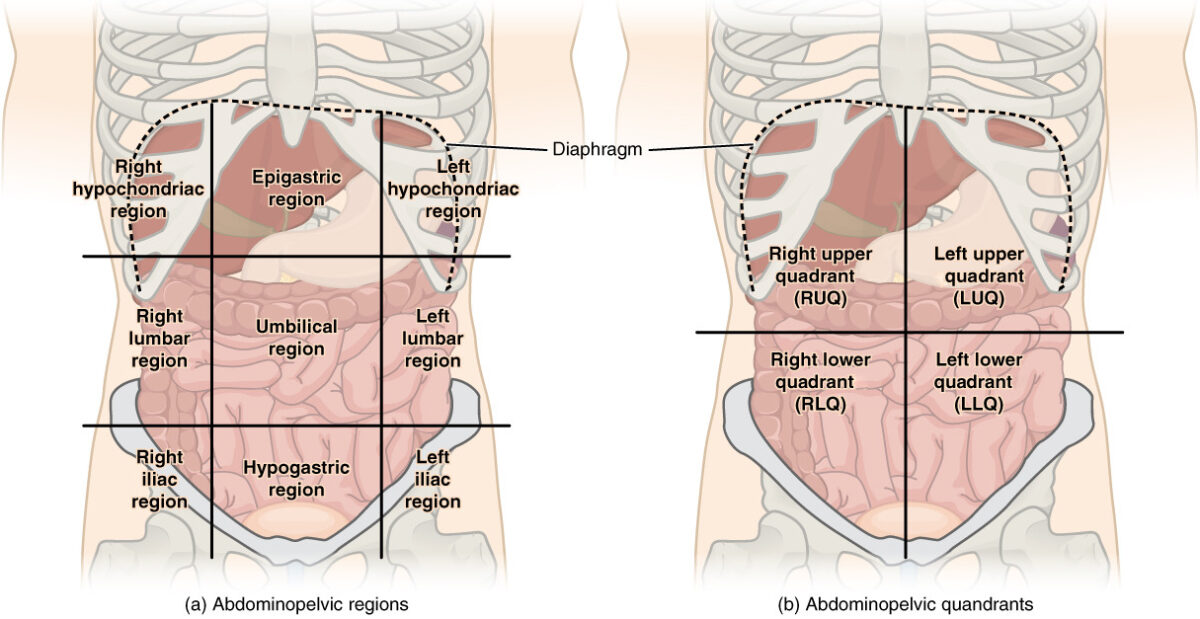
Abdominal quadrant regions:
There are (a) 9 abdominal regions and (b) 4 abdominal quadrants in the peritoneal cavity.
Relationship of intra-abdominal organs to peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy:
The hallmark of acute abdomen is acute onset of severe abdominal pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways that may or may not be associated with other symptoms. A detailed history and physical exam should be performed to determine the correct course of action.

Periumbilical bruising consistent with Cullen sign (hemorrhagic pancreatitis)
Image: “Acute pancreatitis with Cullen’s sign” by Herbert L. Fred, MD. License: CC BY 2.0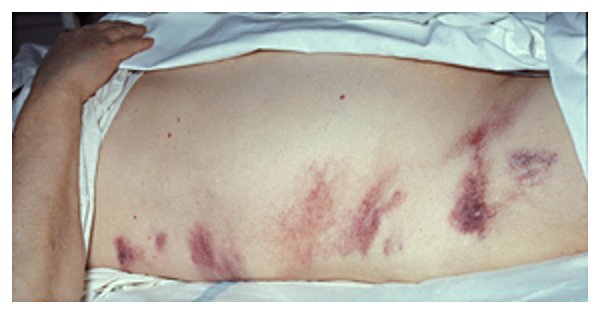
Bruising around the flanks consistent with Grey Turner sign (hemorrhagic pancreatitis)
Image: “Hemorrhagic pancreatitis – Grey Turner’s sign” by Herbert L. Fred, MD and Hendrik A. van Dijk. License: CC BY 2.0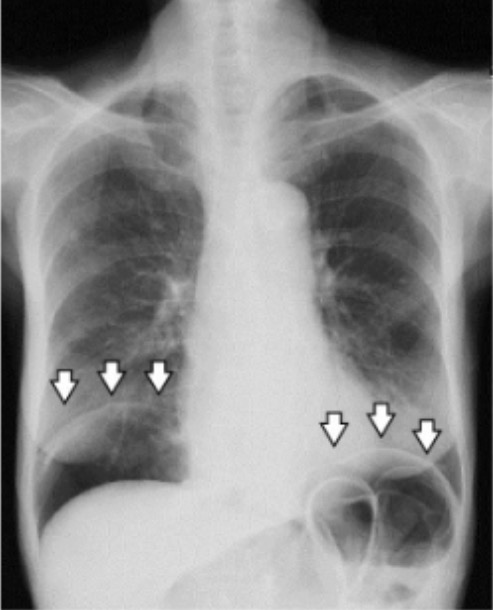
Upright chest X-ray showing pneumoperitoneum (arrows)
Image: “A chest radiograph demonstrating pneumoperitoneum” by Manabu Kaneko et al. License: CC BY 4.0Acute abdomen is a surgical emergency or urgency in the vast majority of cases. The initial evaluation should determine the cases that do not require surgical treatment.
Resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome:
Evaluation:
Surgical treatment is usually needed unless a nonsurgical cause has been established. If surgical intervention is warranted, there are two approaches: