Erectile dysfunction (ED) is defined as the inability to achieve or maintain a penile erection Erection The state of the penis when the erectile tissue becomes filled or swollen (tumid) with blood and causes the penis to become rigid and elevated. It is a complex process involving central nervous system; peripheral nervous systems; hormones; smooth muscles; and vascular functions. Penis: Anatomy, resulting in difficulty to perform penetrative sexual intercourse. Local penile factors and systemic diseases, including diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, cardiac disease, and neurological disorders, can cause ED. Diagnosis is via physical exam and history. Management is guided by clearly discussing patient expectations after explaining the benefits and risks. Treatment includes conservative management with lifestyle modifications, oral medications, and injectables. Invasive surgical penile implants may be considered when conservative measures fail. Ultimately, both the patient and partner must be in tune with the treatment modalities to optimize their overall satisfaction.
Last updated: Apr 11, 2023
Erectile dysfunction (ED) is the recurrent failure to achieve or maintain consistent rigid penile erection Erection The state of the penis when the erectile tissue becomes filled or swollen (tumid) with blood and causes the penis to become rigid and elevated. It is a complex process involving central nervous system; peripheral nervous systems; hormones; smooth muscles; and vascular functions. Penis: Anatomy for satisfactory sexual intercourse.
Clinical importance:
Globally, at least 150 million men suffer from ED:
Prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of ED is closely related to increased age and presence of other systemic comorbidities Comorbidities The presence of co-existing or additional diseases with reference to an initial diagnosis or with reference to the index condition that is the subject of study. Comorbidity may affect the ability of affected individuals to function and also their survival; it may be used as a prognostic indicator for length of hospital stay, cost factors, and outcome or survival. St. Louis Encephalitis Virus.
Erectile dysfunction is a multifactorial disease process with many contributing factors. There are many factors that can be prevented or adjusted to improve the ability to obtain or maintain erections:
The penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy is made of cylindrical structures (paired corpus cavernosa and corpus spongiosum Corpus spongiosum Penis: Anatomy):
Vascular supply to penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy is supplied by the internal iliac artery:
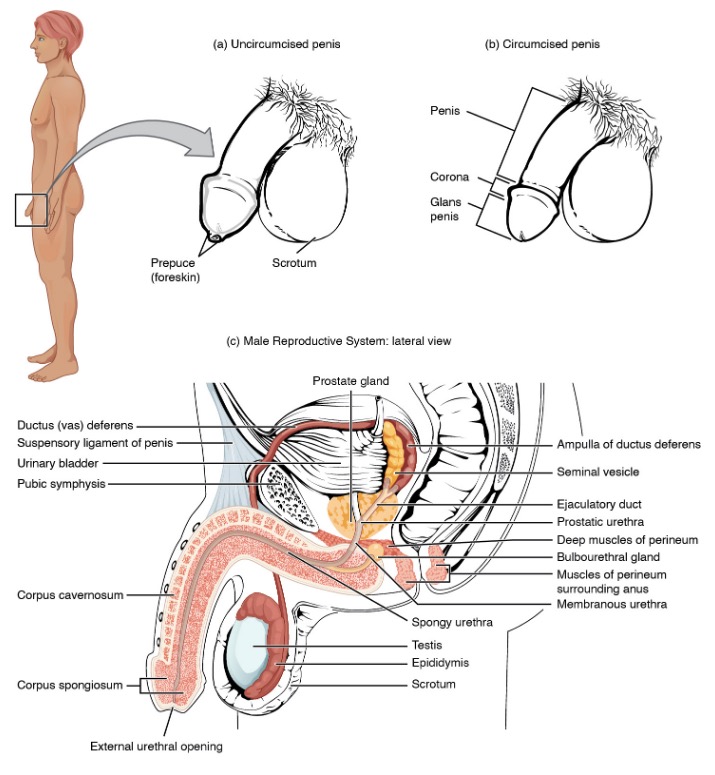
Male reproductive system:
Structures of the male reproductive system include the testes, epididymis, penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the ductus deferens, which is bundled in the spermatic cord. Seminal vesicles and prostate gland add fluids to the sperm to create semen.
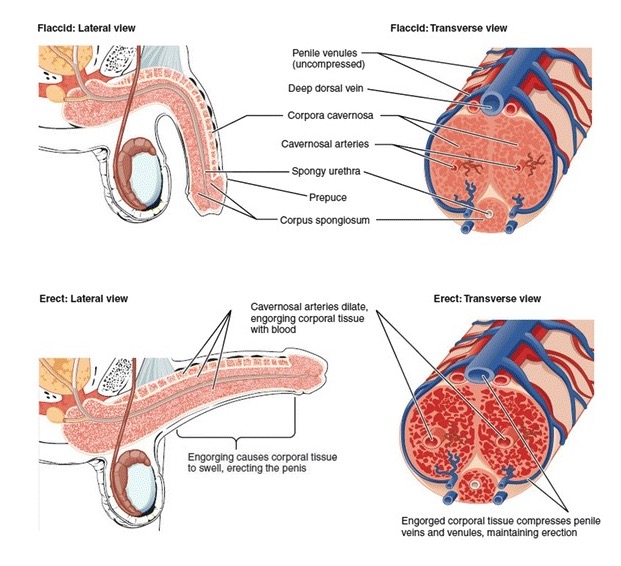
Structural compartments of the penis during the flaccid (top) and erected (bottom) states:
As seen in bottom images (erect: lateral view and erect: transverse view), rapid filling of the sinusoids and subsequent compression of veins and venules maintain penile rigidity.
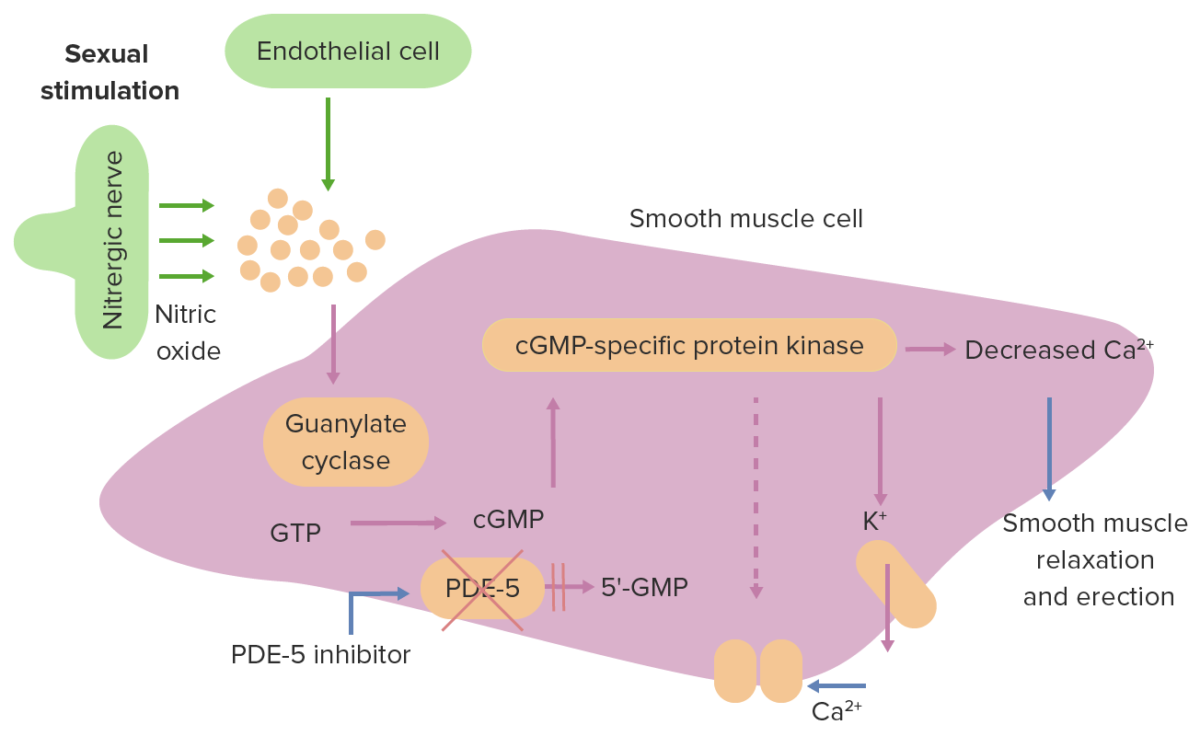
Biochemical mechanism of erection:
Nitric oxide is released from the cavernous nerves upon sexual stimulation, which leads to the activation of guanylate cyclase within the smooth muscle cells of the penis. Guanylate cyclase facilitates the conversion of guanosine triphosphate to cGMP. Specific protein kinases then are acted on by cGMP, causing a decrease in intracellular calcium levels. General effects are smooth-muscle relaxation, vasodilatation, and tumescence. The active cyclic GMP is converted to inactive 5′-GMP by phosphodiesterase type 5 (PDE-5), allowing intracellular calcium levels to normalize, thereby leading to vasoconstriction and loss of tumescence. Phosphodiesterase type 5 inhibitors are used in the management of erectile dysfunction, resulting in tumescence.
Majority of cases are diagnosed based on history and physical examination.
Comprehensive medical and sexual history:
Physical examination:
Laboratory tests:
Ancillary diagnostic tests Diagnostic tests Diagnostic tests are important aspects in making a diagnosis. Some of the most important epidemiological values of diagnostic tests include sensitivity and specificity, false positives and false negatives, positive and negative predictive values, likelihood ratios, and pre-test and post-test probabilities. Epidemiological Values of Diagnostic Tests:
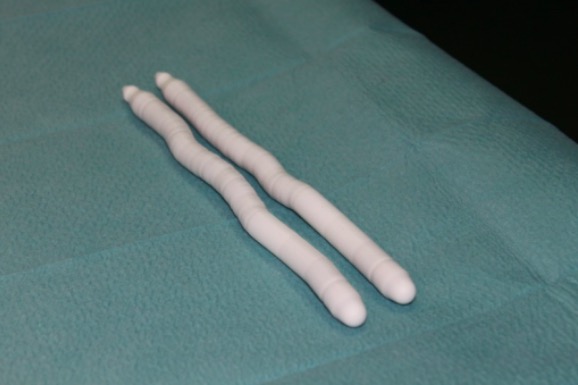
Penile prosthesis: semi-rigid prosthesis in the surgical treatment of Peyronie disease
Image: “Semirigid prosthesis” by MEDAS Medical Center, Bucharest, Romania. License: CC BY 2.0
Penile prosthesis: post-surgical result
Image: “Post operatory result” by MEDAS Medical Center, Bucharest, Romania. License: CC BY 2.0