Asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma is a chronic inflammatory condition of the small airways of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy. The condition is characterized by airway Airway ABCDE Assessment hyperresponsiveness, variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables airway Airway ABCDE Assessment obstruction, and airway Airway ABCDE Assessment inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation. Manifestations include episodic wheezing Wheezing Wheezing is an abnormal breath sound characterized by a whistling noise that can be relatively high-pitched and shrill (more common) or coarse. Wheezing is produced by the movement of air through narrowed or compressed small (intrathoracic) airways. Wheezing, coughing, and shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea. Management of asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma aims to reduce symptoms and minimize future risks and adverse outcomes (hospitalizations, loss of lung function, etc ETC The electron transport chain (ETC) sends electrons through a series of proteins, which generate an electrochemical proton gradient that produces energy in the form of adenosine triphosphate (ATP). Electron Transport Chain (ETC).). Medications commonly utilized include inhalers that allow bronchodilation and inflammatory control. Biologic agents Biologic Agents Immunosuppressants are available for severe asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma.
Last updated: Dec 15, 2025
Contents
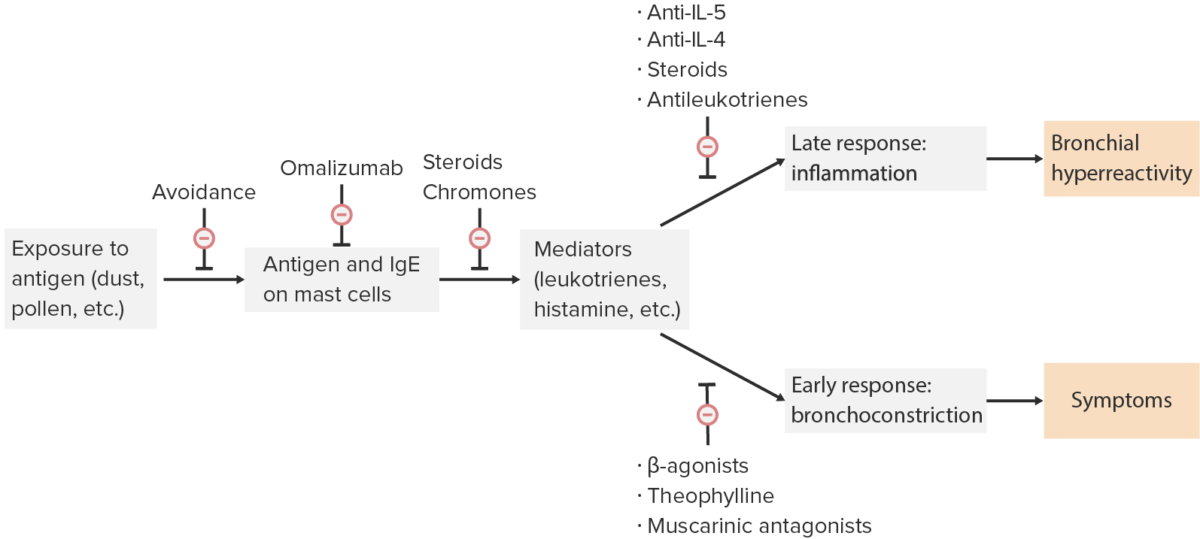
Points in the pathophysiology where asthma medications mediate their action
Image by Lecturio.| Function | Class | Examples |
|---|---|---|
| Bronchodilators | β-agonists |
|
| Methylxanthines | Theophylline | |
| Muscarinic antagonists Muscarinic antagonists Drugs that bind to but do not activate muscarinic receptors, thereby blocking the actions of endogenous acetylcholine or exogenous agonists. Muscarinic antagonists have widespread effects including actions on the iris and ciliary muscle of the eye, the heart and blood vessels, secretions of the respiratory tract, GI system, and salivary glands, GI motility, urinary bladder tone, and the central nervous system. Anticholinergic Drugs |
|
|
| Anti-inflammatory agents | Mast cell Mast cell Granulated cells that are found in almost all tissues, most abundantly in the skin and the gastrointestinal tract. Like the basophils, mast cells contain large amounts of histamine and heparin. Unlike basophils, mast cells normally remain in the tissues and do not circulate in the blood. Mast cells, derived from the bone marrow stem cells, are regulated by the stem cell factor. Angioedema degranulation inhibitors (chromones) | Cromolyn, nedocromil |
| Antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions |
|
|
| Corticosteroids Corticosteroids Chorioretinitis (CS) |
|
|
| Antileukotriene agents | Lipoxygenase inhibitors | Zileuton |
| Leukotriene antagonists | Montelukast, zafirlukast |

An inhaler used for asthma treatment: Inhaled respiratory medications such as bronchodilators and corticosteroids are available in metered-dose inhalers. This device allows delivery of a measured amount of medication into the airway.
Image: “Asthma Inhaler” by NIAID. License: CC BY 2.0Omalizumab (subcutaneous)
Asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma medications are also used for the following conditions: