Encephalitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia, and muscle and joint pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways or with severe symptoms such as seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures, altered consciousness, and paralysis. The diagnosis is based on clinical suspicion, and once suspected, immediate empiric treatment is warranted to prevent catastrophic and long-term neurologic sequelae. Encephalitis is managed with supportive measures and antiviral Antiviral Antivirals for Hepatitis B therapy. Focal neurologic defects are common after encephalitis, and hence, physiotherapy Physiotherapy Spinal Stenosis is usually required.
Last updated: May 16, 2024
Encephalitis is an inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification parenchyma caused by an infection that is usually viral and presents as diffuse or focal neuropsychologic dysfunction.
There are 2 main types of encephalitis:
Viral encephalitis is the most common form of encephalitis. Bacterial, fungal, and parasitic encephalitides are extremely rare.
Viral causes:
Other causes:
Risk factors:
Transmission:
Pathogenesis:
Adults/older children:
Infants:
Distinguishing features (point toward a certain etiology):
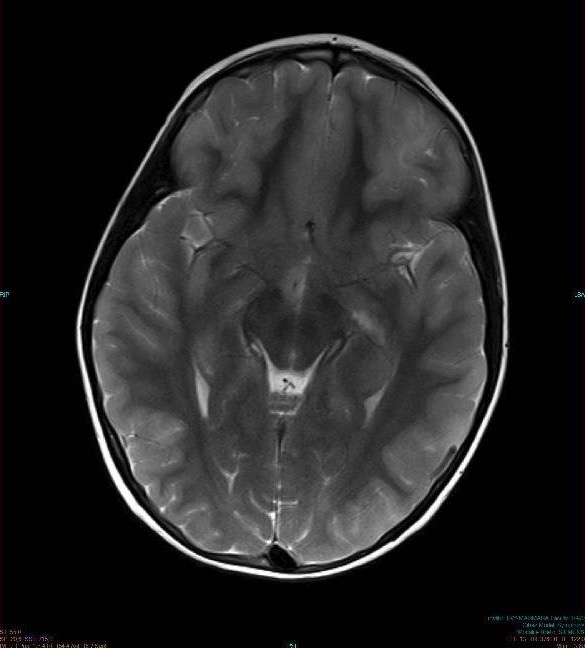
MRI showing Epstein–Barr viral encephalitis:
Contrast enhancement in the posterior side of the bilateral insular cortex, right hypothalamus, and inferior left frontal cortex shows features consistent with encephalitis.
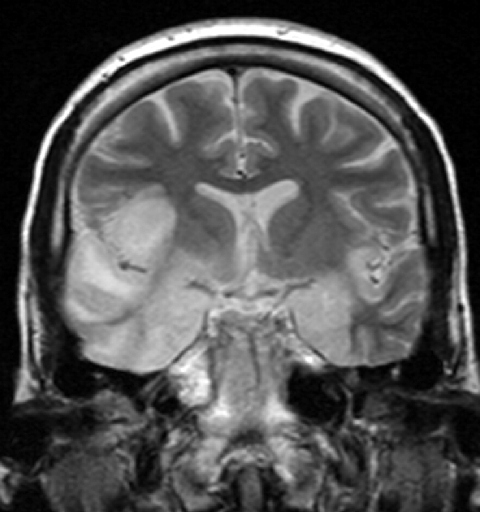
MRI shows increased signal intensity in the temporal lobe of a confirmed case of HSV-1 encephalitis.
Image: “Hsv encephalitis” by Dr. Laughlin Dawes. License: CC BY 3.0EEG EEG Seizures is abnormal in acute encephalitis.
Immediate response to encephalitis is crucial because it can quickly progress to complications.