Angioedema is a localized, self-limited (but potentially life-threatening), nonpitting, asymmetrical edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema occurring in the deep layers of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and mucosal tissue. The common underlying pathophysiology involves inflammatory mediators triggering significant vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs and increased capillary permeability. Clinically, angioedema presents with swelling Swelling Inflammation around the eyes, lips Lips The lips are the soft and movable most external parts of the oral cavity. The blood supply of the lips originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy, tongue Tongue The tongue, on the other hand, is a complex muscular structure that permits tasting and facilitates the process of mastication and communication. The blood supply of the tongue originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy, mouth, bowel wall, extremities, or genitalia. Angioedema may also compromise the airway Airway ABCDE Assessment. Urticaria Urticaria Urticaria is raised, well-circumscribed areas (wheals) of edema (swelling) and erythema (redness) involving the dermis and epidermis with associated pruritus (itch). Urticaria is not a single disease but rather is a reaction pattern representing cutaneous mast cell degranulation. Urticaria (Hives) will be present when the angioedema is mediated by mast cells Mast cells Granulated cells that are found in almost all tissues, most abundantly in the skin and the gastrointestinal tract. Like the basophils, mast cells contain large amounts of histamine and heparin. Unlike basophils, mast cells normally remain in the tissues and do not circulate in the blood. Mast cells, derived from the bone marrow stem cells, are regulated by the stem cell factor. Innate Immunity: Phagocytes and Antigen Presentation, but not when it is due to increases in bradykinin Bradykinin A nonapeptide messenger that is enzymatically produced from kallidin in the blood where it is a potent but short-lived agent of arteriolar dilation and increased capillary permeability. Bradykinin is also released from mast cells during asthma attacks, from gut walls as a gastrointestinal vasodilator, from damaged tissues as a pain signal, and may be a neurotransmitter. Hereditary Angioedema (C1 Esterase Inhibitor Deficiency). Diagnosis is usually clinical but additional testing may include skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions/serum testing for specific antigens and C4 level assessment. Management depends on the underlying mechanism but may include treatment for anaphylaxis Anaphylaxis An acute hypersensitivity reaction due to exposure to a previously encountered antigen. The reaction may include rapidly progressing urticaria, respiratory distress, vascular collapse, systemic shock, and death. Type I Hypersensitivity Reaction, removing any offending agents, antihistamines Antihistamines Antihistamines are drugs that target histamine receptors, particularly H1 and H2 receptors. H1 antagonists are competitive and reversible inhibitors of H1 receptors. First-generation antihistamines cross the blood-brain barrier and can cause sedation. Antihistamines, glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids, and/or therapies that target bradykinin Bradykinin A nonapeptide messenger that is enzymatically produced from kallidin in the blood where it is a potent but short-lived agent of arteriolar dilation and increased capillary permeability. Bradykinin is also released from mast cells during asthma attacks, from gut walls as a gastrointestinal vasodilator, from damaged tissues as a pain signal, and may be a neurotransmitter. Hereditary Angioedema (C1 Esterase Inhibitor Deficiency).
Last updated: May 17, 2024
Angioedema may result from 3 primary mechanisms:
Mast cell-mediated angioedema is typically associated with urticaria Urticaria Urticaria is raised, well-circumscribed areas (wheals) of edema (swelling) and erythema (redness) involving the dermis and epidermis with associated pruritus (itch). Urticaria is not a single disease but rather is a reaction pattern representing cutaneous mast cell degranulation. Urticaria (Hives).
These etiologies are not associated with histamine release or urticaria Urticaria Urticaria is raised, well-circumscribed areas (wheals) of edema (swelling) and erythema (redness) involving the dermis and epidermis with associated pruritus (itch). Urticaria is not a single disease but rather is a reaction pattern representing cutaneous mast cell degranulation. Urticaria (Hives).
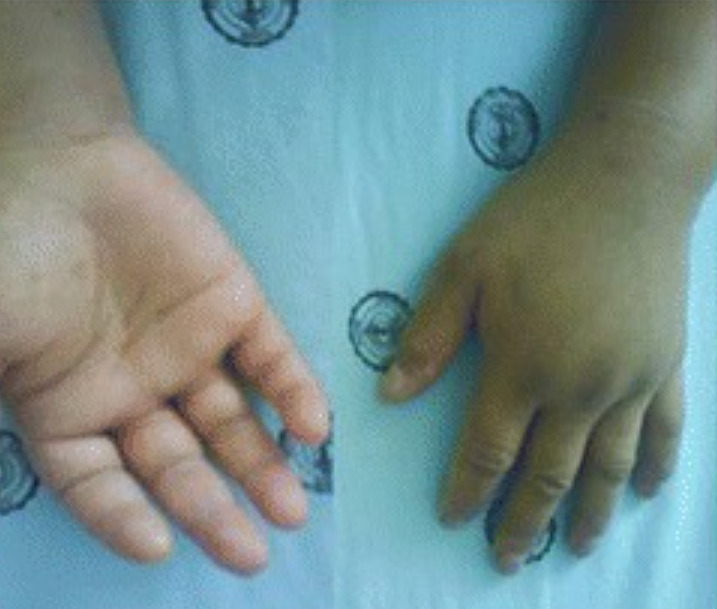
Significant swelling of the hands due to angioedema
Image: “Acute adult-onset Still’s disease presenting as pulmonary hemorrhage, urticaria, angioedema, and leukemoid reaction: a case report and literature review” by Mora Alfonso SA, Rodríguez DM, Londoño JD, Valle-Oñate R, Quintana G. License: CC BY 4.0, edited by Lecturio.
Asymmetrical swelling of the face and lips due to angioedema
Image: “Angioedema of the face” by Boussetta et al. License: CC BY 4.0The diagnosis of angioedema is usually clinical, but testing can help to clarify the etiology. Most cases of chronic angioedema are idiopathic Idiopathic Dermatomyositis.