Rhabdomyolysis is characterized by muscle necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage and the release of toxic intracellular contents, especially myoglobin, into the circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment. Rhabdomyolysis can result from trauma or direct muscle injuries; however, non-exertional and non-traumatic etiologies ( heatstroke Heatstroke Heatstroke is an illness characterized as a core body temperature exceeding 40°C (104°F) with accompanying neurological symptoms including ataxia, seizures, and/or delirium. Heatstroke is usually due to the body's inability to regulate its temperature when challenged with an elevated heat load. Heatstroke, immobilization Immobilization Delirium, medication side effects) can also lead to muscle breakdown. The classic triad of symptoms includes myalgia Myalgia Painful sensation in the muscles. Ion Channel Myopathy, weakness, and tea-colored urine, but the presentation can be nonspecific. History and work-up generally point to diagnosis based on elevated creatine Creatine An amino acid that occurs in vertebrate tissues and in urine. In muscle tissue, creatine generally occurs as phosphocreatine. Creatine is excreted as creatinine in the urine. Acute Kidney Injury kinase levels, abnormal electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes with possible renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome, and dark urine without RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology (indicating myoglobinuria). Management of rhabdomyolysis is by using intravenous fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome.
Last updated: Jan 24, 2023
Rhabdomyolysis is a syndrome marked by muscle necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage, resulting in the release of toxic intracellular muscle constituents into the circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment (especially myoglobin).
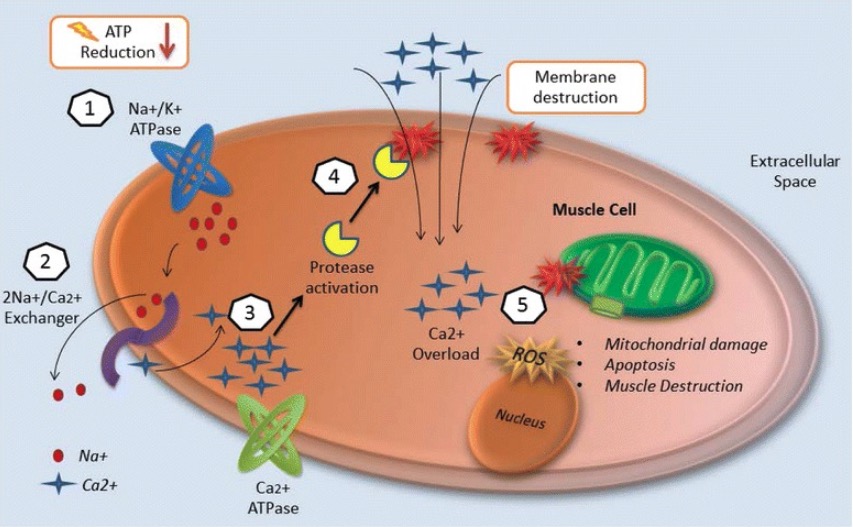
Injury mechanisms of rhabdomyolysis:
1. Energy (ATP) depletion inhibits Na+/K+ ATPase function and increases intracellular sodium.
2. The 2Na+/Ca2+ exchanger increases intracellular calcium.
3. Ca2+ ATPase is not able to pump out intracellular calcium due to energy depletion.
4. Intracellular calcium activates proteases such as phospholipase 2 (PLA2), which destroy the structural components of cell membranes and allow the entry of more calcium.
5. Calcium overload disrupts mitochondrial integrity and induces apoptosis, leading to necrosis of muscle cells.
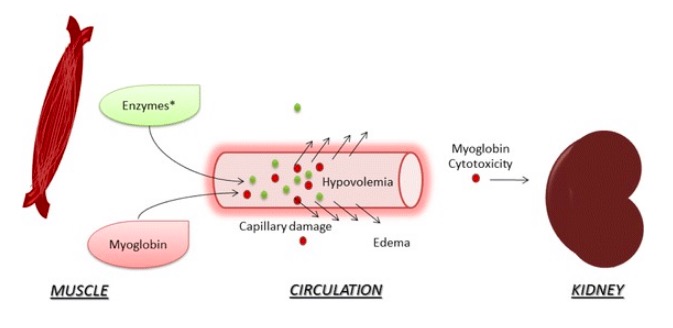
Acute kidney injury (AKI) in rhabdomyolysis (enzymes*: creatine kinase, aldolase, lactate dehydrogenase):
After muscle destruction, myoglobin and enzymes are released into the circulation, damaging capillaries and leading to leakage and edema. Hypovolemia and reduced renal blood flow are associated with AKI. Myoglobin cytotoxicity affects the kidney due to lipid peroxidation and production of reactive oxygen species. Tubular obstruction by myoglobin is also associated with AKI.
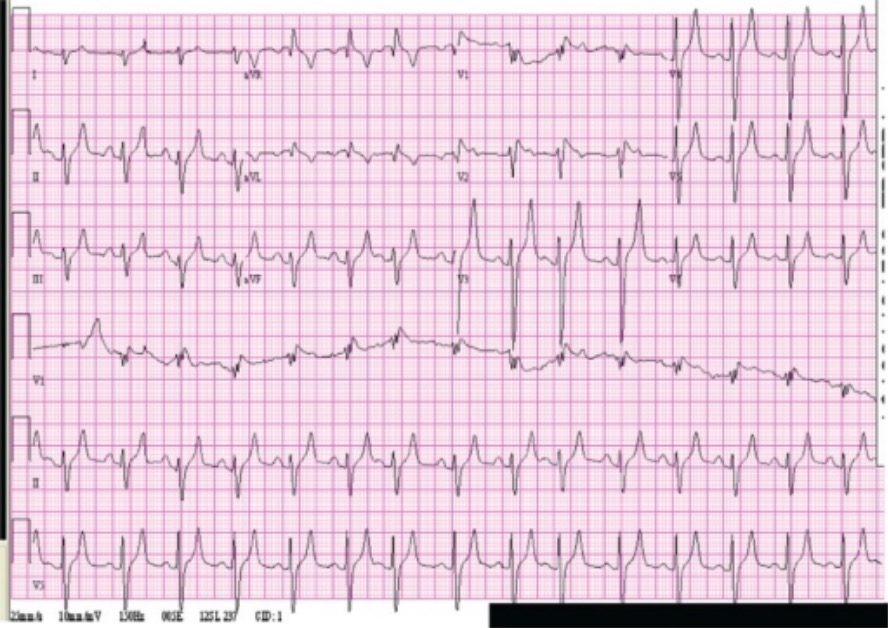
Patient with rhabdomyolysis and hyperkalemia:
Electrocardiogram of a patient treated for rhabdomyolysis, showing peaked T waves and wide QRS. The patient had a serum potassium level of 8 mEq/L.